Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The guarded prognosis of hip dislocations has been well recognized and frequently reported. Although pure dislocations fare better than fracture-dislocations, recent reports indicate that unsatisfactory long-term results are common even with pure dislocations and can be anticipated in up to one-half of this better-prognosis group. Delayed treatment and failure to recognize and treat associated injuries have historically contributed to poor results. More recently, however, improved imaging modalities, including magnetic resonance arthrography (MRA), have improved postdislocation clinical diagnoses that may benefit from surgical intervention. Emerging techniques, including surgical dislocation of the hip and arthroscopic management, may improve outcomes through better-focused evaluations and less invasive therapeutic interventions. As always, the treatment of hip dislocations remains directed toward emergent reduction and attainment of a stable, congruent joint.
The hip is an intrinsically stable joint.
The labrum ensures that at least 50% of the femoral head is covered by the osteocartilaginous labral–acetabular complex in any position of hip motion.
The femoral neck is most often anteverted in its relationship to the transcondylar axis; males were found to have an average of 7 degrees of anteversion, with a range of 2 degrees of retroversion to 35 degrees of anteversion.
The hip is an intrinsically stable joint. More than 400 N of force (90 pounds) is required simply to distract the femoral head from the acetabulum. Hip stability is directly related to the bony and labral anatomy of the acetabulum and femoral head. The thick fibrous capsule with ligamentous condensations and the local muscular anatomy augment the inherent stability afforded by the ball-and-socket configuration of the hip.
Inherent bony stability is achieved through the size and relationship of the femoral head and femoral neck to the acetabular socket, which is deepened by an osteocartilaginous labrum. The femoral head forms approximately two-thirds of a sphere and is situated on a femoral neck approximately three-quarters the diameter of the femoral head. This relationship in size between the femoral head and the femoral neck allows the femoral head to be deeply seated within the acetabular socket without compromising either stability or range of motion.
The acetabulum is formed from the convergence of the ischium, ilium, and pubis at the triradiate cartilage. Biomechanical testing of newborn cadavers found the joints to be extremely stable at birth, although some debate exists as to the actual stabilizing structures. It is unclear whether the acetabulum deepens with development, but anatomic studies reveal in adult hips that approximately 40% of the femoral head is covered by the bony acetabulum at any position of hip motion. The articular surface of the acetabulum is horseshoe-shaped, with articular cartilage covering the posterior, superior, and anterior portions of the acetabular cavity. The cartilaginous labrum is attached to the perimeter of the portion of acetabulum covered by articular cartilage. The acetabular notch or cotyloid fossa lies in the midinferior portion of the acetabulum. The transverse acetabular ligament crosses the most inferior portion of the acetabular notch, extending from the posteroinferior end of the labrum to its anteroinferior limit. The ligamentum teres originates from the acetabular notch ( Fig. 52.1 ).
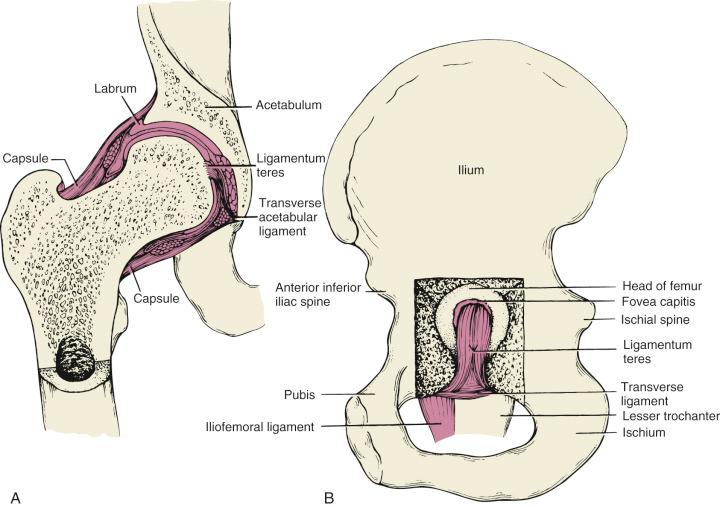
The labrum deepens the acetabulum and increases the stability of the joint. The labrum ensures that at least 50% of the femoral head is covered by the osteocartilaginous labral–acetabular complex in any position of hip motion. These motions include extension (from a prone position) of 20 to 30 degrees, flexion of 120 to 135 degrees, abduction of 45 to 50 degrees, adduction of 20 to 30 degrees, and internal (medial) and external (lateral) rotation of 45 degrees each. Individuals vary, and rotational measurements differ if the rotation is tested in hip extension or flexion.
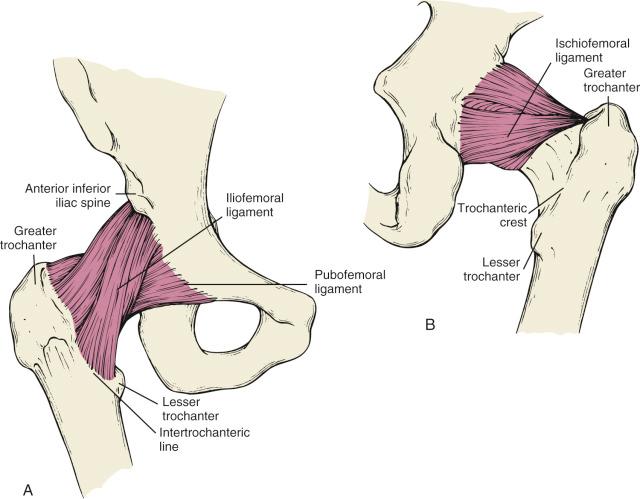
A capsule surrounds the hip joint, extending posteriorly from the acetabular rim to the midfemoral neck and anteriorly from the acetabular rim to the intertrochanteric ridge. The primary capsular fibers run longitudinally and are supplemented by much stronger ligamentous condensations that run in a circular and spiral fashion. The iliofemoral ligament courses inferiorly from the iliac body and anterior inferior iliac spine in two distinct directions. One band continues directly inferiorly to insert on the intertrochanteric line just anterior to the lesser trochanter. The second band courses obliquely in a spiral fashion to insert on the intertrochanteric line overlying the greater trochanter. An additional anterior ligamentous condensation extends from the anterior border of the superior pubic ramus to the intertrochanteric line and is called the pubofemoral ligament. This ligament is believed to serve as a checkrein against pathologic extension of the hip. Posteriorly, the ischiofemoral ligament is a broad and less dense condensation extending in an oblique and horizontal fashion from the ischial border of the acetabulum to the superior base of the femoral neck and the region of the trochanteric fossa ( Fig. 52.2 ).
The femoral neck is most often anteverted in its relationship to the transcondylar axis (coronal plane) of the femur. Cadaveric studies have demonstrated significant variability in average anteversion and in range of anteversion based on gender and genetic background. White males, for example, were found to have an average of 7 degrees of anteversion, with a range of 2 degrees of retroversion to 35 degrees of anteversion. White females had an average anteversion of 10 degrees, with a range of 2 degrees of retroversion to 25 degrees of anteversion. In contrast, Hong Kong Chinese males averaged 14 degrees of anteversion, with a range of –4 to 36 degrees, and Hong Kong Chinese females averaged 16 degrees of anteversion, with a range of only 7 to 28 degrees.
Ultrasonographic measurements performed by Upadhyay and colleagues on a series of patients who had sustained a posterior hip dislocation demonstrated significantly less anteversion on both the injured and the uninjured sides compared with a control group. Diminished anteversion might therefore be a predisposing factor to hip dislocations. Further discussion of this possibility is included in the following section on mechanisms of injury.
Hip dislocations are almost always due to high-energy trauma.
Femoral head position, based on an instantaneous position secondary to hip rotation and on the anatomic structure of the hip, determines the type of injury.
Femoral head fractures, impactions, and osteochondral injuries occur as the femoral head exits the acetabulum.
Hip dislocations are usually caused by high-energy trauma and, as a result, are often associated with other significant injuries.
The anatomic configuration of the hip joint provides a high degree of inherent stability. As a result, hip dislocations are almost always due to high-energy trauma. Motor vehicle crashes account for more than two-thirds of hip dislocations reported in the literature. Advances in vehicle restraints should theoretically reduce the morbidity and mortality of patients who do sustain hip dislocations resulting from motor vehicle collisions, but recent reports have unfortunately been unable to substantiate this anticipated benefit of passenger restraints. Automobile–pedestrian accidents, falls from heights, industrial injuries, and athletic trauma account for the other reported mechanisms of injury.
Pathologic forces transmitted to the hip joint in all hip dislocations result from one of three common sources: the anterior surface of the flexed knee striking an object, the sole of the foot with the ipsilateral knee extended, and the greater trochanter. Less frequently, the dislocating force may be applied to the posterior pelvis, with the ipsilateral foot or knee acting as the counterforce.
The type of hip injury sustained depends on the amount and direction of applied force, the quality of bone at both the proximal femur and the acetabulum, and the position of the hip. Letournel demonstrated through vector analysis the relationship of the position of the leg and pelvis to the injury sustained, explaining why an individual sustains an anterior dislocation, posterior dislocation, or fracture-dislocation of the hip. In the classic dislocation seen in unrestrained automobile drivers, the left hip tends to dislocate posteriorly, whereas the right hip develops either a posterior fracture-dislocation or an anterior dislocation. At the time of the rapid deceleration of the automobile, the right foot is positioned either on the brake pedal or on the accelerator pedal. The body pivots forward on this fixed foot, and the left knee strikes the dashboard with the hip and knee both flexed to 90 degrees. This force delivered in this position tends to force the femoral head out posteriorly, usually without a fracture. With less flexion of the hip at the time of impact, the femoral head strikes either the posterior or the posterosuperior aspect of the acetabulum, leading to a fracture-dislocation. Similarly, if the right foot is firmly pressed against the brake pedal at the moment of impact, the femoral head strikes the posterior or posterosuperior acetabulum. If an unsuspecting driver is involved in a collision, the right leg may be in a relaxed position on the gas pedal, with the hip externally rotated and abducted. In this position, the inner aspect of the knee strikes the dashboard, resulting in the accentuation of both abduction and external rotation. This extreme position results in anterior dislocation ( Fig. 52.3 ).

The degree of internal or external rotation of the hip dramatically affects the position of the head within the acetabulum and therefore the resulting injury complex. Another factor potentially affecting hip dislocation pathology is femoral neck anteversion. In one series of patients studied with ultrasound, significantly less anteversion was found in patients who sustained posterior hip dislocations. Individuals with posterior fracture-dislocations had less anteversion than the control population but more than the pure dislocation group ( Table 52.1 ). These findings strongly imply that femoral head position, based on an instantaneous position secondary to hip rotation and on the anatomic structure of the hip, determines the type of injury.
| Right Hip Mean Anteversion (Degrees) | Left Hip Mean Anteversion (Degrees) | |
|---|---|---|
| Normal subjects | 15.4 | 16.3 |
| Type I dislocation, right hip | 1.1 | 10.4 |
| Type I dislocation, left hip | 4.4 | –3.2 |
| Posterior fracture-dislocation, right hip | 3.2 | –5.5 |
| Posterior fracture-dislocation, left hip | 5.0 | –6.1 |
Pringle demonstrated that extreme abduction with external rotation of the leg can produce anterior dislocations in cadaver specimens. In a flexed-hip position, extreme abduction and external rotation led to anterior obturator dislocation. With the hip extended, these pathologic forces result in a superoanterior (pubic) dislocation. Epstein and Harvey also proposed that anterior dislocations are secondary to hyperabduction of the hip and suggested that either the greater trochanter or the femoral neck impinges on the lateral ilium, which then acts as a lever to push the femoral head out of the acetabulum.
Femoral head fractures, impactions, and osteochondral injuries occur as the femoral head exits the acetabulum. Actual shearing of the superior, anterosuperior, or posterosuperior femoral head can occur as the femoral head strikes the anterior or posterior acetabular lip. Ligamentum teres avulsion fractures from the femoral head are frequently seen. These fragments can range in size from small cartilaginous avulsion fragments to major osteocartilaginous fragments of the femoral head ( Fig. 52.4 ). Such loose fragments can become incarcerated between the femoral head and the acetabular articular surface after reduction of the dislocation. Failure to remove these incarcerated fragments could lead to symptoms of a loose body and articular cartilage erosion.
Femoral neck fractures associated with femoral head dislocations may result from two different mechanisms. Several case reports describing these associated injuries propose that the injury forces that first dislocate the femoral head then force the head against the pelvis. If the energy that produced the dislocation has not been fully dissipated, the continued application of force to the leg while the femoral head abuts the pelvis will fracture the femoral neck or the femoral shaft.
The second proposed mechanism of femoral neck fracture is “iatrogenic” and occurs at the time of manipulative reduction. Most reported cases of so-called iatrogenic neck fractures also report an associated femoral head fracture. This seems to imply that the femoral neck can absorb a significant amount of energy and develop a nondisplaced fracture that is not radiographically visible before the manipulation. Obviously, extreme care must be taken in reviewing the films before the reduction to ensure that a possible nondisplaced fracture is not overlooked. In addition, reduction techniques must be gentle and well controlled; lever-type manipulations must be avoided.
Hip dislocations are usually caused by high-energy trauma and, as a result, are often associated with other significant injuries. Attendant neurologic injuries, musculoskeletal injuries, and intra-abdominal and chest injuries have all been widely reported.
A large variety of knee injuries are associated with hip dislocations. Gillespie reported on a series of 35 associated knee injuries; 25 were attributed to direct trauma to the knee region, and 10 were associated with pathologic stresses applied to the knee ligaments. Among the reported injuries were osteochondral fractures of the patella, tibia, and femur; posterior cruciate injuries; collateral ligament injuries; and traumatic patellofemoral chondrosis. A delay in the diagnosis of these injuries frequently occurred (2 days to 6 months). Tabuenca and Truan reported that 46 of 187 patients (25%) with fracture or fracture-dislocation of the hip had an ipsilateral knee injury. The diagnosis of knee injury was delayed in 7 of the 46 patients, prolonging overall recovery in these patients.
Sciatic nerve injuries have been documented in association with hip dislocations in 8% to 19% of patients. The mechanism of injury is presumed to be stretching of the nerve over the posteriorly dislocated, internally rotated femoral head. Large posterior wall acetabular fragments can also stretch the nerve or even pierce or partially lacerate it. Intraoperatively, the nerve may appear normal or nearly so, in spite of a functional deficit. No cases of sciatic nerve injury have been reported secondary to anterior dislocations.
A complete disruption of the sciatic nerve is unusual. Most commonly, the peroneal portion of the nerve is significantly involved, with little or no evident tibial nerve dysfunction. The peroneal component of the sciatic nerve lies more posterior than the tibial component, so the proximity of this portion of the nerve to the dislocated femoral head may alone account for the higher incidence of peroneal nerve injury, whereas the tibial nerve is usually spared. Gregory proposed that the unusual association of the peroneal portion of the nerve with the piriformis muscle may further place this portion of the nerve at risk.
Ipsilateral femur fractures have also been frequently reported with hip dislocations. Unfortunately, in some of these reported cases, the initial diagnosis of hip dislocation was not accurate. Because a femoral fracture masks the typical physical findings of a hip dislocation, routine adherence to a policy of radiographic examination of the joint above and below the fracture, as well as always obtaining an appropriate image of the entire pelvis whenever the femur is fractured, should minimize missing this combination of injuries.
A careful assessment of the entire patient as well the dislocated hip is essential, especially in the polytraumatized patient.
Hip dislocations are subdivided into either anterior or posterior based on the location of the femoral head.
The descriptive term central dislocation is an outdated phrase and is no longer relevant to the classification of hip injuries.
Hip dislocations are subdivided into either anterior or posterior dislocations based on the location of the femoral head. A “central dislocation” is in fact a medial displacement of the femoral head secondary to a displaced acetabular fracture. This poorly descriptive term, central dislocation, is an outdated phrase and is no longer relevant to the classification of hip injuries.
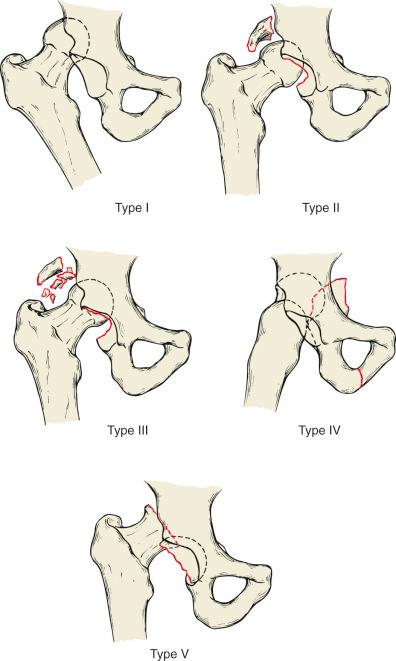
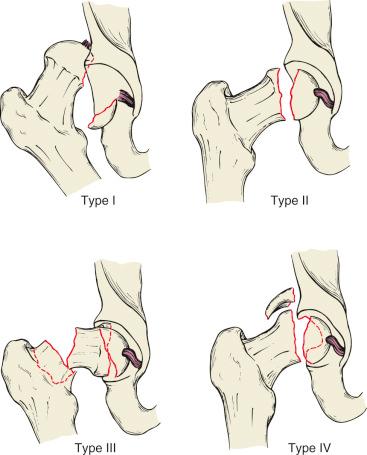
Thompson and Epstein and, later, Stewart and Milford devised similar classification systems for posterior hip dislocations. Both systems were based on the severity of the associated acetabular fracture as well as the presence of a femoral head fracture. A Thompson–Epstein type I dislocation is a pure dislocation with at most an insignificant posterior wall fragment. A type II dislocation is associated with a single large posterior wall fragment. A type III dislocation has a comminuted posterior wall fracture, and a type IV disclocation has an “acetabular floor” (more than posterior wall) fracture. Finally, a type V dislocation is associated with a femoral head fracture ( Fig. 52.5 ).

Stewart and Milford's system was based on the stability of the hip joint and the condition of the femoral head. Type I dislocations have either no fracture or an insignificant acetabular rim fracture. A type II dislocation is associated with either a single or a comminuted posterior wall fracture, but the hip remains stable. Type III injuries are fracture-dislocations with gross instability of the hip joint secondary to loss of structural support, and a type IV dislocation is associated with a femoral head fracture.
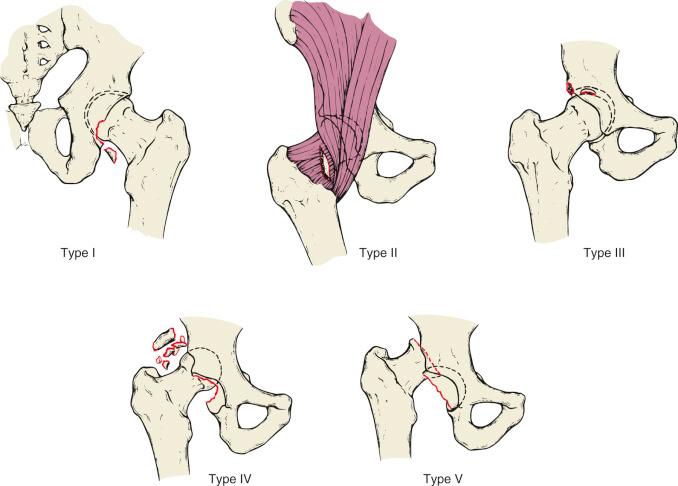
Pipkin classified posterior hip dislocations associated with femoral head fractures based on the location of the femoral head fracture. A Pipkin type I injury has a femoral head fracture inferior to the fovea centralis; a type II injury has a fracture line extending superior to the fovea centralis (and usually including the fovea); a type III injury is any femoral head fracture in association with a femoral neck fracture; and a type IV injury is any femoral head fracture associated with an acetabular fracture ( Fig. 52.6 ).

A classification system for posterior dislocations that combines elements of earlier classification systems was proposed by Levin and is presented in Table 52.2 and Fig. 52.7 . This classification is designed to guide the treatment of hip dislocations. A Levin type I posterior dislocation is either a pure dislocation or is associated with an insignificant posterior wall fracture. Postreduction computed tomography (CT) demonstrates a concentric reduction, no widening of the joint, no incarcerated fragments between articular surfaces, and no femoral head or posterior wall impaction fractures. Occasionally, a postreduction CT image demonstrates a small bone fragment within the acetabular fossa secondary to a ligamentum teres avulsion. Such fragments are of no clinical significance unless they are incarcerated between the articular surfaces of the femoral head and the acetabulum.
| Type I | No significant associated fractures; no clinical instability after concentric reduction |
| Type II | Irreducible dislocation without significant femoral head or acetabular fractures (reduction must be attempted under general anesthesia) |
| Type III | Unstable hip after reduction or incarcerated fragments of cartilage, labrum, or bone |
| Type IV | Associated acetabular fracture requiring reconstruction to restore hip stability or joint congruity |
| Type V | Associated femoral head or femoral neck injury (fractures or impactions) |

Levin type II posterior dislocations are pure dislocations without associated femoral head or acetabular fractures in which the femoral head is irreducible by closed manipulation. A hip is presumed to be irreducible only if a closed reduction under general anesthesia fails to bring the femoral head back into the acetabulum.
A Levin type III posterior dislocation is one in which the postreduction clinical examination reveals an unstable hip or one in which the postreduction imaging studies reveal a widened joint space or an incarcerated cartilaginous or osseous fragment. The instability can be secondary to failure to fully seat the femoral head due to an incarcerated fragment, an extensive labral detachment, or massive capsular and ligamentous disruption.
A Levin type IV posterior dislocation is associated with a significant acetabular fracture requiring reconstruction. Surgery in these patients is indicated to restore joint stability or joint congruity, or both. These fracture-dislocations of the hip are more appropriately classified according to their acetabular fracture pattern.
Levin type V posterior dislocations are associated with femoral head or femoral neck injuries. The femoral head injuries may be indentations, depressions, or cleavage fractures. These injuries are classified further based on the femoral head fracture classification system.
Anterior hip dislocations occur much less frequently than do posterior ones. Thompson and Epstein classified these injuries based on their anterior location (superior or inferior) as well as on the presence of associated acetabular fractures. Longer-term evaluations of these injuries have revealed a much less favorable prognosis than was initially believed. A significant portion of the poor results may be related to associated femoral head injuries.
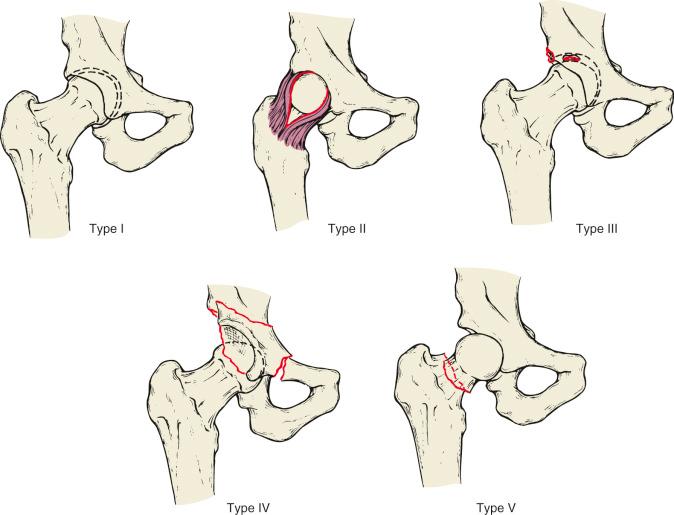
Both classifications divided anterior dislocations into subgroups of superior and inferior types and then simply subdivided these into groups based on associated fractures. However, these distinctions did not influence the treatment of anterior dislocations. Therefore Levin proposed a system for classifying anterior dislocations that follows his scheme for posterior dislocations but includes the term anterior following the subtype (e.g., type I anterior dislocation; Fig. 52.8 and Table 52.3 ).

| Type I | No significant associated fractures; no clinical instability after concentric reduction |
| Type II | Irreducible dislocation without significant femoral head or acetabular fractures (reduction must be attempted under general anesthesia) |
| Type III | Unstable hip after reduction or incarcerated fragments of cartilage, labrum, or bone |
| Type IV | Associated acetabular fracture requiring reconstruction to restore hip stability or joint congruity |
| Type V | Associated femoral head or femoral neck injury (fractures or impactions) |
The initial physical examination must include an evaluation of the entire involved limb.
Abrasions overlying the patella should alert the physician to the possibility of occult knee ligament injuries.
Sciatic nerve injuries are frequently seen, and an accurate diagnosis should be made before any closed or open manipulation of the hip.
Patients presenting with dislocations and fracture-dislocations of the hip are in severe discomfort. They complain of an inability to move their lower extremity and may also complain of numbness distally. Typically, they have been involved in high-energy trauma such as motor vehicle accidents, industrial accidents, or falls from heights.
Individuals suffering multiple injuries often experience pain at numerous sites and, as a result, may not be able to localize specific injuries. Associated injuries to the chest, abdomen, spine, and extremities all compromise the patient's ability to isolate and differentiate symptoms. A high percentage of patients with hip dislocations are obtunded or unconscious when they arrive in the emergency department and, as a result, are unable to assist the physician in the initial evaluation.
The classic appearance of an individual with an isolated posterior hip dislocation is a patient in severe pain with the hip fixed in a position of flexion, internal rotation, and adduction ( Fig. 52.9 ). Patients with an isolated anterior dislocation hold the hip in marked external rotation with mild flexion and abduction ( Fig. 52.10 ). Despite these classic descriptions, the appearance and alignment of the extremity can be dramatically altered by ipsilateral extremity injuries.
The initial physical examination must include an evaluation of the entire involved limb. Care must be taken to check for the presence of a partial or complete sciatic nerve injury. Sciatic nerve injuries are frequently seen, and an accurate diagnosis should be made before any closed or open manipulation of the hip. Lumbosacral plexus injuries are associated with major pelvic trauma, but a careful neurologic examination in a cooperative patient may be required to demonstrate their presence, and injury may not be evident until sufficient patient comfort is attained.
Abrasions overlying the patella or proximal anterior tibia are often evidence of the site of application of the injury force. These findings should alert the physician to the possibility of occult knee ligament injuries, patellar fractures, or osteochondral fractures of the distal femur. Pelvic ring injuries and spine injuries may also be associated with hip dislocations, and these areas must be carefully assessed.
Nerve function should be carefully assessed before a manipulative reduction. Obviously, if the patient has sustained a head injury or is unconscious or uncooperative, the neurologic examination will be incomplete. This should be noted on the patient's medical record.
All dislocated hips must be reduced as soon as possible. This is especially the case when nerve palsy is present, to relieve stretching of the nerve. In a retrospective review of 106 dislocated hips, Hillyard and Fox compared the incidence of sciatic nerve injury in 69 hips relocated before transfer with 36 patients transferred from another hospital with the hip still dislocated. There was a higher incidence of major sciatic nerve injury (complete sciatic or peroneal motor deficit) in patients transferred with the hip still dislocated ( P = 0.0453). Time to relocation was significantly longer in patients with major motor nerve injury ( P = 0.016). The presence of an associated fracture in their series had no influence on sciatic nerve injury rates, but the length of time the hip remains dislocated clearly seems to influence the incidence and severity of major sciatic nerve injury.
Surgical exploration is not indicated for associated neurologic injury, except when initially normal neurologic function is lost secondary to the reduction. In this situation, the surgeon must ascertain whether the nerve has become incarcerated either in fracture fragments or in the hip joint. Some investigators recommend immediate surgical repair of displaced posterior wall fragments that are associated with sciatic nerve injuries. This may protect the nerve from further injury by the fracture fragments. The implications of sciatic nerve injury are addressed later in this chapter.
All patients must have a screening anterior-posterior (AP) radiograph of the pelvis or an equivalent CT scan.
The review of the initial screening AP pelvic radiograph must be done carefully and systematically.
Additional films usually include a postreduction AP view of the hip and a CT scan but may also include additional plain films (internal and external oblique views, Judet views).
A critical role for magnetic resonance imaging (MRI) after traumatic hip dislocation has not been well established.
Because hip dislocations are strongly associated with high-energy trauma and multiple injuries, the physician should assume the possibility of such injuries. All patients suffering from blunt trauma who have an altered mental state, or local signs or symptoms, must have a screening anterior-posterior (AP) radiograph of the pelvis or an equivalent CT scan. Similarly, all patients with significant lower extremity injuries, spine fractures, or abdominal or chest injuries should also have one of these studies. Alert and fully cooperative injured patients may not need pelvic radiographs if they are hemodynamically stable and no symptoms or signs suggest an occult pelvic fracture or injury of the hip region.
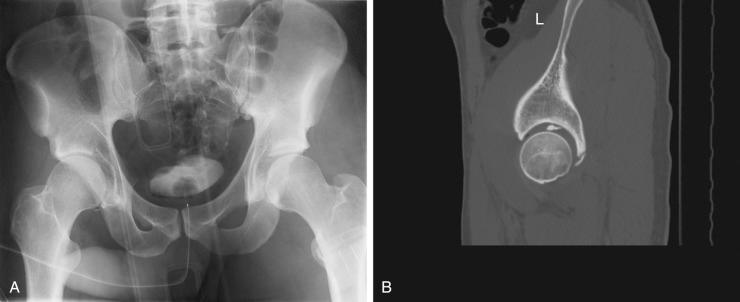
The review of the initial screening AP pelvic radiograph must be done carefully and systematically. The femoral heads should appear symmetrical in size, and the joint spaces should be symmetrical throughout the arc of the acetabulum as well as when comparing left and right. In the presence of a posterior hip dislocation, the femoral head appears smaller on the AP radiograph. In an anterior dislocation, the femoral head appears slightly larger than that in the normal hip. The Shenton line should be smooth and continuous. The relative appearance of the greater and lesser trochanters may indicate pathologic internal or external rotation of the hip. An adducted or abducted position of the femoral shaft should also be noted. Finally, careful evaluation of the femoral neck must rule out the presence of a femoral neck fracture before any manipulative reduction. A true AP view of the proximal femur may be required to evaluate this region before attempting closed reduction maneuvers. And if a CT scan is obtained instead of an AP pelvis radiograph, it must demonstrate both femoral neck regions satisfactorily.
After the diagnosis of a hip dislocation, additional imaging studies are required before definitive surgical treatment. Most often, these additional studies are obtained after a closed reduction has been achieved.
Once the diagnosis of a hip dislocation is made, additional radiographs are obtained before any open surgical intervention. Usually, these films are obtained after a successful closed reduction, but on occasion, they are obtained before an open reduction of an irreducible femoral head. Additional films usually include a postreduction AP view of the hip and a CT scan but may also include additional plain films.
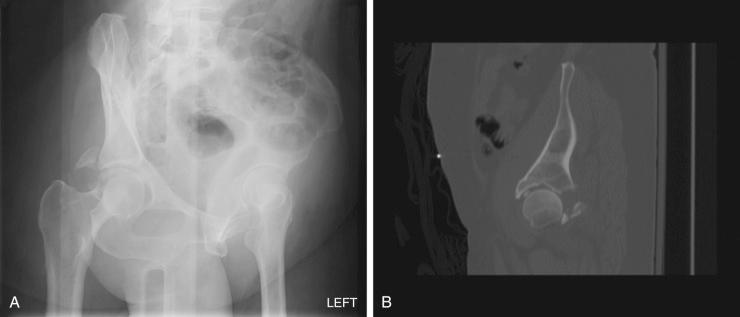
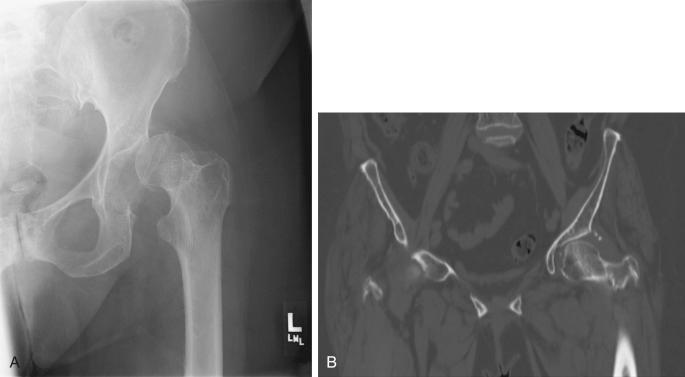
Plain film analysis should include an AP radiograph centered on the affected hip. Internal and external oblique views (Judet views) at 45 degrees centered on the affected hip are obtained if a CT scan is not available and may be desirable in some cases even with CT availability. These views are always obtained if a significant acetabular fracture is present. The AP radiograph should be carefully reviewed to determine the presence of incarcerated osteochondral fragments and asymmetry of the joint space. The iliac oblique (with the opposite side anterior) view brings the beam perpendicular to the iliac wing. It is best for evaluation of the integrity of the posterior column and the anterior wall. The obturator oblique (ipsilateral anterior oblique) view is parallel to the iliac wing (perpendicular to the obturator ring). It is the best view for evaluating the integrity of the posterior acetabular wall, as well as the pelvic brim and the posterior part of the obturator ring ( Figs. 52.11 and 52.12 ).
In addition, each oblique view presents a different profile of the femoral head. Femoral head depressions and fractures should be noted. The precise interpretation of these initial films is critical if open surgery is required before obtaining CT analysis. The proper choice of surgical approach may depend on the correct preoperative identification of associated acetabular or femoral head fractures. If necessary, they can be obtained in the operating room after induction of anesthesia.
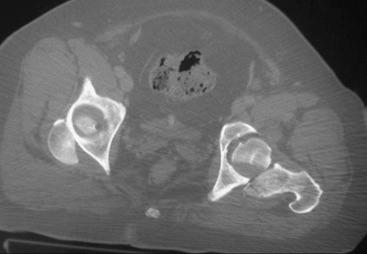
CT should be routinely obtained after a successful closed reduction of a dislocated hip. If a successful closed reduction is impossible and an open reduction is planned, a CT scan should be obtained if this study will not unduly delay reduction of the hip. Emergency CT scanning is readily available in most hospitals and has demonstrated accuracy in the evaluation of the traumatized abdomen. A specific request for 3-mm cuts through the hips and additional cuts through the sacroiliac joints may be required to ensure that CT scans done for evaluating the abdomen also include these regions.
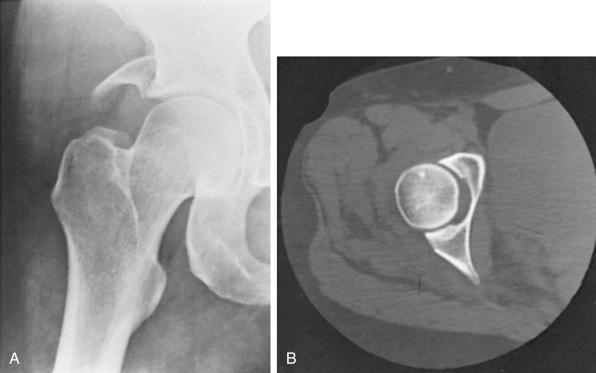
The value of CT is its ability to assess the femoral head, to demonstrate the presence of small intraarticular fragments, and to assess the congruence of the femoral head and acetabulum. Baird and colleagues placed 2- and 4-mm methyl methacrylate spacers in cadaver hip joints and then performed plain radiographs and CT scans on these specimens. The CT scans routinely revealed the 2-mm spacers, whereas the plain radiographs failed to demonstrate their presence. Fig. 52.13 demonstrates an incarcerated osteochondral fragment not visualized on postreduction plain radiographs.

CT imaging better visualizes the size, location, and displacement of acetabular wall fractures. Ebraheim and associates described the use of soft tissue windows with enhancement techniques of CT images in an attempt to improve the visualization of intraarticular fragments. Fairbairn and coworkers described the presence of gas bubbles in the hip joint seen on CT scan. This finding in a hip not having a documented dislocation could reflect a hip that was subluxed and spontaneously reduced. Calkins and colleagues devised a scale that attempts to correlate the percentage of the displaced acetabular wall as measured on CT with hip stability. Although some basic parameters can be developed from this study, a significant degree of variability exists, making precise correlations impossible ( Figs. 52.14 and 52.15 ). CT has also proved to be valuable in demonstrating displaced impaction injuries of the acetabular articular surface ( Fig. 52.16 ).
The value of CT in demonstrating femoral head injury has been reported by a number of investigators. Occult impactions, indentations, and other fractures have all been clearly visualized on CT. The degree of displacement of the fractures is accurately assessed by CT.
A critical role for MRI after traumatic hip dislocation has not been well established. Numerous investigations have reported the diagnosis of labral disruptions, femoral head contusions and microfractures, sciatic nerve injury, intraarticular fragments, and pelvic vein thrombophlebitis. In the acute setting, MRI might become most valuable in evaluating a widened hip joint in the presence of a normal CT scan (to image interposed soft tissues and incarcerated fragments). In addition, a diagnosis of a labral disruption may be documented by high-resolution MRI in a hip that is unstable despite normal CT analysis ( Fig. 52.17 ). Magnetic resonance phlebography can assess the pelvic veins for occult thrombophlebitis. MRI has been proposed to monitor for the development of osteonecrosis at the femoral head, but early investigations have not supported this use.
Isotope imaging with either technetium-labeled phosphate compounds or technetium 99m–sulfur colloid is not indicated in the postinjury imaging of hip dislocations. Meyers and coworkers suggested using technetium 99m–sulfur colloid to predict femoral head viability after hip dislocation. The value of such studies has not, however, been demonstrated.
The management of a hip dislocation is divided into an initial phase of achieving a rapid reduction of the dislocation followed by a secondary phase of planning and performing definitive care. This division into phases is necessary because of the initial urgency of reducing the hip to decrease the risk of long-term complications. Numerous investigators reported a strong correlation of avascular necrosis (AVN) of the femoral head with the amount of time during which the hip remains dislocated. After the femoral head has been reduced, urgency is diminished. The appropriate diagnostic workup, including CT analysis of the hip, can then be completed. Surgical intervention, if necessary, can be undertaken when the patient has become physiologically stable and higher-priority injuries have been addressed.
Closed reduction should be reserved for simple dislocations not associated with any fractures.
All fracture-dislocations should be treated by immediate open surgery to remove loose fragments from the joint and to reconstruct fractures.
A hip that is stable after reduction does not require traction.
The Allis method of reduction relies primarily on traction applied in line with the deformity.
If the hip cannot be reduced by closed manipulation under general anesthesia, an immediate open reduction must be performed.
Although it is generally agreed that dislocated hips should be reduced rapidly, some debate exists in the older literature as to whether this should be by closed or open methods and whether reductions should be attempted under sedation in an emergency department or in an operating room setting under general anesthesia. Most investigators, however, recommend an immediate attempt at a closed reduction. Epstein and DeLee recommended that closed reduction be reserved for simple dislocations not associated with any fractures. They urged that all fracture-dislocations should be treated by immediate open surgery to remove loose fragments from the joint and to reconstruct fractures. Thompson and Epstein demonstrated improved long-term results in a retrospective comparison of open treatment with closed treatment. It is probable that the improved results of immediate open reduction were related to the ability to visually clear the acetabulum of all loose fragments, which at the time of Epstein's work could not be radiographically demonstrated. The introduction of CT and its routine use in postreduction evaluation obviate the need for routine immediate open reduction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here