Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Numerous nonstructural hip disorders may be amenable to arthroscopic intervention.
Successful operative hip arthroscopy is first dependent on proper patient selection, careful patient positioning, and accurate portal placement.
Routine hip arthroscopy should include both central and peripheral compartments.
Snapping hip syndromes, including iliopsoas tendon and iliotibial (IT) band, can be addressed.
Various disorders reside in the peritrochanteric space, including bursitis and abductor tendinopathies; they are collectively grouped as the greater trochanteric pain syndrome.
Abnormalities in the subgluteal and ischiofemoral spaces can collectively be called deep gluteal syndrome . These cases can typically be managed nonoperatively. In rare cases that fail conservative management, arthroscopy may have a role.
Femoroacetabular impingement (FAI) and dysplasia are the two most common structural problems implicated in hip pathology. However, numerous nonstructural problems are associated with disorders of the hip joint and hip region. These include macrotrauma, repetitive overuse microtrauma, consequences of kinetic and kinematic disorders, and intrinsic tissue disease. Hip problems manifested by painful symptoms are often the culmination of multifactorial causes. Underlying disease may render some joints more susceptible to acute injury. For example, acute subluxations and dislocations encountered among contact sports, which are relatively low-velocity injuries compared with those resulting from vehicular trauma, often have underlying findings of impingement. It is likely that owing to the underlying morphology, the hip is rendered more susceptible to luxation by the levering effect. In order to aid physicians in determining what the origin(s) of the symptoms may be, the layer concept was introduced. This compartmentalizes the hip into 4 layers; the osteochondral (I), inert (II), contractile (III) and neuromechanical (IV) layers. Structural pathology would principally involve abnormalities of the 1st and occasionally the 4th layer. The 2nd and 3rd layers include the static (capsule, labrum, ligamentum teres) and dynamic (musculature crossing hip) stabilizers of the joint. Abnormalities in these 2 layers along with certain pathology in the 4th layer (leading to sciatic nerve entrapment) could be considered as the sites of origin for nonstructural hip pathology.
Numerous soft tissue disorders around the hip can cause problems and may be amenable to endoscopic intervention. The collective group of coxa saltans, which includes snapping of the iliopsoas tendon and IT band and possibly other less evident entities, can be corrected endoscopically. Bursectomy can be performed, and many cases of recalcitrant trochanteric bursitis may actually represent painful abductor tendinopathies. Keep in mind that some of these disorders may be incidental, normally occurring observations and others can occur as a normal consequence of aging or of subtle gait abnormalities. It is a challenge to the clinician to distinguish pathologic processes from normal variations. It is also important to keep in mind that several disorders may coexist and that the clinician must differentiate which are the principal problems and how they should best be managed. Recommendations may range from simple activity modifications to structured conservative treatment to surgical intervention.
For nonstructural problems, the most common indication for arthroscopy is pain caused by some type of pathologic condition that can be corrected by arthroscopic techniques. Rarely is arthroscopy considered in the presence of a painless disorder. Often, patients may present for assessment with modest symptoms that are not sufficient to create a functional problem. Under these circumstances, thoughtful observation and other nonoperative treatments may be appropriate. If symptoms are worsening in the presence of recognized pathology, it may be prudent to be proactive in considering surgical intervention. Keep in mind that various disorders may coexist, which can include pathologic conditions and anomalies that are not responsible for the patient's symptoms. For example, hip joint pathology may occur in conjunction with a snapping iliopsoas tendon, which may or may not be a contributing cause of pain warranting correction.
Contraindications to hip arthroscopy are few. Most important is simply ensuring that the patient's condition is amenable to and appropriate for arthroscopic intervention. Another important consideration is ensuring that the patient's expectations can be practically met by the procedure. Surgery in the presence of unreasonable expectations will be a failure regardless of the skill with which the procedure is performed. Advanced disease states, such as severe degenerative arthritis, are contraindications simply because arthroscopy cannot reasonably be of any benefit. Some severe deformities, wound problems, and medical conditions may contraindicate arthroscopy or possibly even any type of surgery.
Imaging studies are an important part of the diagnostic workup and surgical planning. Radiographs reveal joint morphology and underlying structural disorders as well as the presence of degenerative disease. It is important to keep in mind that damage within the joint is typically substantial before radiographic changes become evident. Thus, reasonable joint space preservation may not preclude the existence of considerable degenerative disease. Also, subtle radiographic changes should be taken as serious evidence of advanced pathology.
Conventional magnetic resonance imaging (MRI) is an important component of most preoperative planning for hip surgery. Its reliability for detecting intraarticular pathology may be variable, but it is often helpful to rule out disorders that will not benefit from arthroscopy, such as avascular necrosis, transient regional osteoporosis, and many others. Gadolinium arthrography with MRI (magnetic resonance arthrography [MRA]) is better but is not completely reliable for detecting all intraarticular pathology. Injecting anesthetic along with contrast is a valuable tool in substantiating that the hip joint is the source of symptoms. In cases of multiple pain generators, intraarticular injection helps to distinguish how much the hip is contributing. Similarly, ultrasound (US)-guided injection of extraarticular regions (psoas, greater trochanteric, deep gluteal) may prove to be a valuable diagnostic and treatment tool. Assessing the patient's response to the injection can be important in making the decision for surgery. In general, imaging studies are good for assessing labral pathology but may be less reliable in detecting associated articular damage. This is important when counseling patients because the uncertain extent of articular damage is often a limiting factor in the success of arthroscopy. Computed tomography has a significant role in assessing bony architecture and the 3-dimensional morphology of the joint but is less often enlightening for soft tissue problems about the hip.
Problematic snapping of the iliopsoas tendon and the IT band is mostly identified from the history and examination findings. This snapping is usually a dynamic phenomenon, not predictably reproduced with examination under anesthesia, and the arthroscopic findings do little to substantiate the diagnosis. Abductor tendinopathies can be a normal consequence of aging but can also be a source of relevant clinical pathology. Thus, the clinical findings dictate how aggressive one should be with lesions encountered in the peritrochanteric space.
The technique illustrated is being performed with the patient in supine position. The important principles for performing safe, effective, reproducible arthroscopy are the same whether the patient is in the lateral decubitus or supine orientation. Portal placements, relationships of extraarticular structures, and arthroscopic anatomy are all the same regardless of positioning.
A standard fracture table or custom distraction device is needed to achieve effective joint space separation. The C-arm is important for precise placement of instrumentation within the joint. Extra-length arthroscopy instruments are also available to accommodate the dense surrounding soft tissue.
The procedure is commonly performed with the patient under general anesthesia. It can be performed under epidural but requires an adequate motor block to ensure optimal distractibility of the joint.
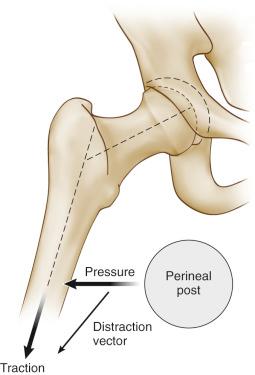
The perineal post is heavily padded and lateralized against the medial thigh of the operative hip ( Fig. 52.1 ). This aids in achieving the optimal traction vector ( Fig. 52.2 ) and reduces pressure directly on the perineum, lessening the risk of neuropraxia of the pudendal nerve. Neutral rotation achieves a constant relationship between the topographic landmarks and the joint. Slight flexion may relax the capsule, but excessive flexion should be avoided because this places undue tension on the sciatic nerve and may block access to the anterior portal. Typically, about 50 pounds of force is needed to distract the joint. In general, the goal is to use the minimum force necessary to achieve adequate distraction while keeping traction time as brief as possible. Two hours is usually recognized as a reasonable limit for traction.

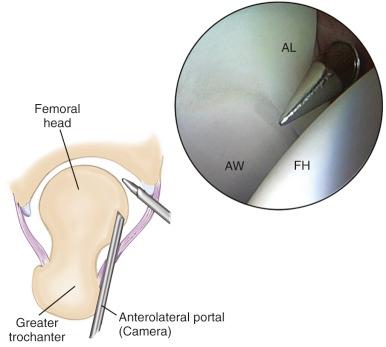
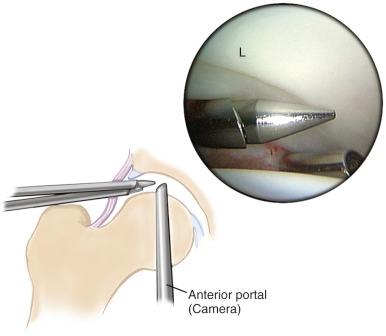
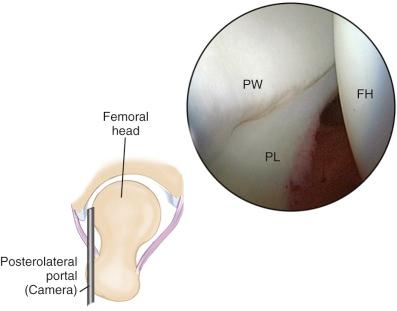
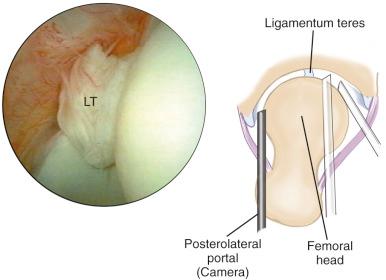
Three standard portals provide optimal access for the central compartment ( Figs. 52.3 and 52.4 ). Two of these (anterolateral and posterolateral) are placed laterally over the superior margin of the greater trochanter at its anterior and posterior borders. The anterior portal is placed at the site of intersection of a sagittal line drawn distally from the anterior superior iliac spine and a transverse line across the tip of the greater trochanter. With careful orientation to the landmarks in relation to the joint, these portals are a safe distance from the surrounding major neurovascular structures. Additional portals may be needed occasionally. Most common is a more distal mid-anterior portal for placing anchors in conjunction with labral repair. The more distal position is necessary to ensure that the anchor diverges at the rim to avoid perforating the acetabular surface.
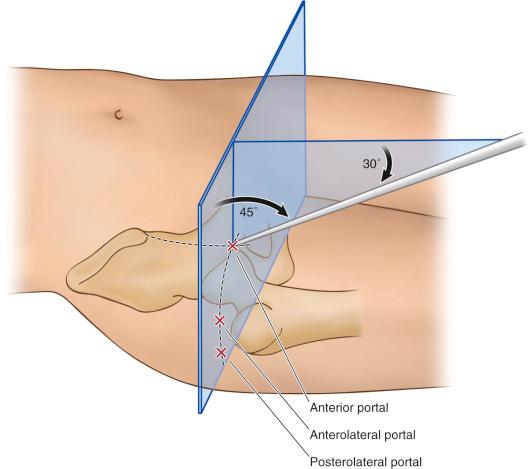
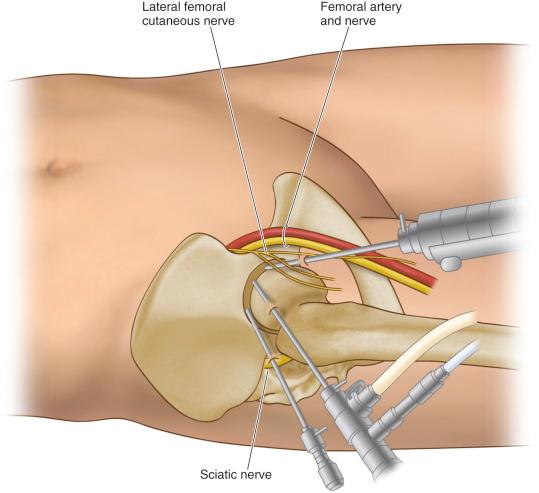
After traction is applied, a spinal needle is placed from the anterolateral position and the joint is distended with fluid. The anterolateral portal is then established under fluoroscopic control for introduction of the arthroscope ( Fig. 52.5 ). Careful attention is necessary to avoid perforating the labrum or scuffing the articular surface. Using the 70-degree scope, the anterior and posterolateral portals are placed under direct arthroscopic view as well as under fluoroscopy for precise entry into the joint. Diagnostic and operative arthroscopy is then achieved by interchanging the arthroscope with instruments between the three established portals. Use of both 70-degree and 30-degree scopes provides optimal viewing despite limitations of maneuverability within the joint ( Figs. 52.6 through 52.9 ). If needed, supplemental portals can be placed under similar arthroscopic control.
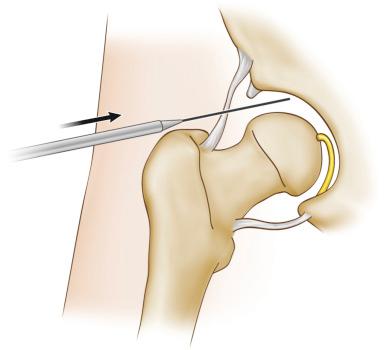
Routine arthroscopy of the peripheral compartment is performed after arthroscopy of the intraarticular compartment has been completed. The instruments are removed, the traction released, and the hip flexed approximately 45 degrees ( Fig. 52.10 ). This relaxes the capsule, providing access to the peripheral compartment. Note that when correction of impingement is performed, a capsulotomy is needed for exposure and facilitates movement between the central and peripheral compartments without the need to remove the instruments. This technique is described in Chapter 54 .

At least 2 portals are used routinely to access the peripheral compartment. These include the anterolateral portal and an ancillary portal established 4 to 5 cm distally. A broad safe zone in which to work is present and numerous variations on portal placement are available. It is simply important to be consistent in portal choices for reproducibility of placement and for orientation to the anatomy of the periphery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here