Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Reviewed for currency January 14, 2021
Reviewed for currency January 14, 2021
Helicobacter pylori (formerly known as Campylobacter pylori or pyloridis ) was first isolated from humans in 1982. This highly motile, curved, gram-negative rod lives within the mucus layer overlying the gastric mucosal epithelium. H. pylori is commonly found in the human stomach, and when present, it is usually the single dominant species. Essentially all persons colonized with H. pylori have a cellular infiltrate in the lamina propria of the gastric antrum and fundus. The first isolation of H. pylori in pure culture and recognition of its association with gastritis and peptic ulcer disease led to the awarding of the Nobel Prize in Medicine in 2005 to Barry Marshall and Robin Warren, two physicians in Australia. The presence of H. pylori increases the risk of peptic ulcer disease and gastric cancer, but also may be associated with health benefits, including a decreased risk of esophageal reflux and its consequences and protection against childhood asthma and related disorders. With the development of effective therapies to eradicate H. pylori, physicians are faced with the challenge of determining which patients will benefit from therapy and which may be harmed.
H. pylori organisms are small (0.5–1.0 µm in width and 2.5–4.0 µm in length), curved, microaerophilic, gram-negative rods. Because they closely resemble members of the genus Campylobacter, they were initially considered to belong to that genus. However, multiple genotypic and phenotypic characteristics are different from those of campylobacters, and a new genus, Helicobacter, was established. Most mammals studied to date are colonized with one or more distinct Helicobacter species. Examples include Helicobacter mustelae in ferrets, Helicobacter felis in dogs and cats, Helicobacter muridarum in mice, Helicobacter nemestrinae in nonhuman primates, and Helicobacter acinonychis in cheetahs. Individual Helicobacter species preferentially colonize either the stomach or the intestinal tract, and typically are adapted for colonization of specific mammalian hosts.
H. pylori is the most important human-associated species from a medical perspective and may be considered the prototype for this group of gastric organisms. Related gastric bacteria that colonize the human stomach are considered in a separate section of this chapter. Helicobacter fennelliae and Helicobacter cinaedi are intestinal organisms that cause diarrheal illnesses, and H. cinaedi also can cause bacteremia and cellulitis, especially in immunocompromised patients. Because the clinical features of these infections resemble those of Campylobacter spp., they are discussed in Chapter 216 . Helicobacter spp., such as Helicobacter hepaticus, Helicobacter bilis, and Helicobacter rappini, have been identified in the colon and biliary tract of rodents, and there is human carriage as well. Preliminary evidence suggests that these species might colonize the diseased human biliary tract, but whether they contribute to biliary pathology is uncertain. Thus there are both gastric and intestinal residential Helicobacter species in humans. In contrast to H. pylori, the residential intestinal species are not known to cause disease in nonimmunocompromised humans.
H. pylori cells are highly motile, with a rapid corkscrew motion, and have multiple, polar, sheathed flagella. Although these cells are classically curved or spiral in fresh cultures, spherical (coccoid) forms are present in older cultures. The major biochemical properties of H. pylori and several related bacteria are shown in Table 217.1 . A prominent biochemical characteristic of gastric helicobacters is production of urease. H. pylori urease is a hexadimer consisting of 61- and 28-kDa subunits, both of which are essential for activity.
| CHARACTERISTIC | H. PYLORI | HELICOBACTER MUSTELAE | HELICOBACTER FELIS | CAMPYLOBACTER JEJUNI |
|---|---|---|---|---|
| Urease | + | + | + | − |
| Catalase | + | + | + | + |
| Oxidase | + | + | + | + |
| H 2 S production | − | − | − | + |
| Guanosine plus cytosine content (%) | 35–38 | 36 | 42.5 | 33–36 |
| Hippurate hydrolysis | − | − | − | + |
| Nitrate reduction | − | + | + | + |
| Resistance to nalidixic acid (30-µg disk) | + | − | + | − |
| Cephalothin (30-µg disk) | − | + | − | + |
| Growth at 42°C | − | + | + | + |
| Growth at 37°C | + | + | + | + |
| Growth at 25°C | − | − | − | − |
The complete genome sequences of hundreds of different H. pylori strains have been determined, and the transcriptome of one strain has been analyzed in detail. Comparison of these genome sequences has permitted the definition of a core genome, and numerous strain-specific genes have been identified, including genes that encode restriction-modification enzymes and others that encode cell surface components. In comparison to many other bacterial species, H. pylori has few two-component regulatory systems. Frameshift mutations occur commonly within open reading frames encoding certain H. pylori proteins, which suggests that H. pylori may use mutation to control phenotype, with the host selecting for the “most fit” organism within a particular environmental niche. Plasmids are present in most H. pylori isolates; they vary in size, and their functional properties are mostly unknown at present. Bacteriophages also have been detected in H. pylori.
Although H. pylori is highly homogeneous in the biochemical characteristics analyzed in clinical microbiology, including urease, oxidase, and catalase positivity, there is substantial genetic variation among strains, both in gene content and in nucleotide sequences of individual genes. Humans may be simultaneously colonized with more than one strain of H. pylori, and as many as five different strains have been identified in an individual subject. H. pylori strains are naturally competent (i.e., able to take up heterologous DNA) and frequently undergo intergenomic and intragenomic recombination. The strain-specific restriction-modification systems diminish recombination and may facilitate colonization of a host by several different strains simultaneously. Because of point mutations and recombination, H. pylori are among the most varied of all species in the human biosphere.
Distinct clonal lineages of H. pylori are not readily identifiable when comparing strains from unrelated humans, but multilocus sequence typing has revealed the existence of multiple H. pylori populations with distinct geographic distributions. Classification of strains by this approach is useful for anthropologic studies, and may be relevant to differences in pathogenicity of strains in hosts of different ethnicities, as described in recent studies from South America. The most important dichotomy among H. pylori strains is the presence or absence of the cytotoxin-associated genes ( cag ) pathogenicity island, a 35- to 40-kilobase chromosomal region encoding the secreted protein CagA and genes encoding components of a type IV secretion system that mediates delivery of CagA into host cells. Both cagA + and cagA − strains are present in H. pylori populations in most parts of the world, which suggests that this chromosomal region was acquired in the distant past. The cag status of an H. pylori strain is relevant to the risk of a number of clinical outcomes (as discussed later). Another heterogeneous locus that provides a basis for typing strains is vacA, a conserved gene that encodes a secreted protein (vacuolating cytotoxin) that interacts with epithelial cells. Three regions of vacA have major polymorphisms: the s region (with allelic types s1 and s2), the m region (with allelic types m1 and m2), and the i region (with allelic types i1 and i2). Type s1 vacA genotypes are strongly linked to the presence of cagA, and therefore cagA + and vacA s1–positive genotypes are each associated with similar clinical outcomes.
H. pylori has been isolated from persons in all parts of the world. Similar organisms have been isolated from primates, but other animal sources for H. pylori have not been identified, nor have reservoirs been found in food, soil, or water. It now appears likely that humans are the major, if not sole, reservoir for H. pylori. Analyses of genetic heterogeneity among strains indicate that H. pylori has been present in humans for at least 100,000 years, if not longer, and the current geographic distribution of H. pylori alleles reflects ancient migrations of human populations. The recent finding of H. pylori DNA in a 5300-year-old corpse, frozen in ice, provides further evidence for the long-standing association of H. pylori with humans. These data support the notion that H. pylori is indigenous to humans, as its relatives are to other mammals. Prolonged coevolution of H. pylori with human populations may be linked to reduced pathogenicity. For example, a study from Colombia found that African-ancestry H. pylori was relatively benign in humans of African ancestry but was associated with higher risk of gastric cancer in individuals of Amerindian ancestry.
The high prevalence of colonization among persons in settings where sanitary conditions are suboptimal, including institutions for individuals with intellectual disabilities and orphanages, suggests that horizontal fecal-oral transmission or oral-oral transmission occurs. H. pylori has occasionally been isolated from feces, especially from children. H. pylori has also been isolated from dental plaque, and H. pylori DNA may be detected in saliva by the polymerase chain reaction assay, which raises the possibility of oral-oral transmission as well. Studies of persons attending clinics for either sexually transmitted diseases or infertility indicate that sexual transmission does not occur very frequently, if at all. The relative contribution of fecal-oral, oral-oral, or vomitus-oral transmission of H. pylori is not known. H. pylori infection clusters in families, and the presence of the organism in a child is highly associated with large family size and older siblings. On occasion, transmission occurs from person to person via improperly cleaned endoscopes.
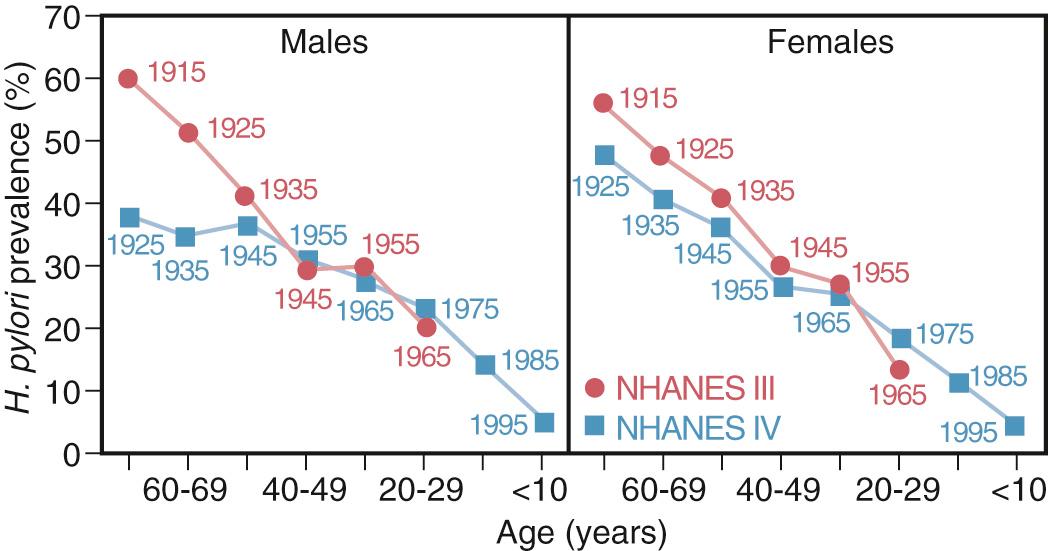
In most populations, H. pylori appears to be almost universally acquired during childhood, but not in the first year of life. Once acquired, H. pylori can persistently colonize the stomach for decades or for an entire lifetime. H. pylori has also been found to transiently colonize children and nonhuman primates, a phenomenon that may be associated with less pathogenic strains, or the selective bottleneck of transmission to a new host, with failure to sufficiently adapt to sustain colonization. The prevalence of H. pylori colonization varies considerably among different populations around the world and is dependent on age and socioeconomic development ( Fig. 217.1 ). In developing countries, by age 10 years, more than 70% of persons carry H. pylori. Among non-Hispanic whites in the United States, little colonization is currently occurring during childhood, and the relatively high prevalence rates in adults reflect acquisition many decades ago. Among blacks and Hispanics, a high prevalence is seen at all ages. The annual incidence of acquisition has ranged from 0.5% among epidemiologists in the United States to 7.4% among persons at an institution for individuals with intellectual disabilities in Australia. The incidence of H. pylori has been progressively declining in the United States and other developed countries, probably as a result of smaller family sizes, decreased crowding, improved sanitation, and more than 70 years of widespread antibiotic use. Thus the age-related increase in prevalence reflects a birth cohort phenomenon (with persons born earlier having higher acquisition rates in childhood), continuing exposure and low-level new colonization into young adulthood, and continuing loss of H. pylori because of collateral effects from antibiotic use. The birth cohort effect predominates. The prevalence of H. pylori is increased among immigrants and persons of lower socioeconomic status. In total, in less than 1 century in the United States, colonization has gone from being ubiquitous to being present in 5% of children ; this is a change in human microecology of major proportion.
H. pylori is able to survive and multiply in the acidic gastric environment, which is hostile to the growth of most bacteria. When intraluminal acidity diminishes as a result of gastric atrophy, H. pylori is less able to colonize the stomach, possibly because of competing organisms. H. pylori characteristics that permit gastric colonization include microaerophilism for survival within the mucous gel, spiral shape, flagella for motility within this viscous layer, and urease activity, which generates ammonium ions that buffer gastric acidity. Although most organisms appear to be free-living in the mucous layer, smaller numbers appear to be adherent to the mucosal epithelial cells. Organisms may be found at the luminal surface of the gastric mucosa and also deeper within gastric glands. H. pylori localizes almost exclusively in association with gastric-type epithelium. Affected gastric epithelium may be in the gastric antrum or fundus or may be ectopic in the duodenum or in the esophagus. In contrast, H. pylori does not colonize intestinal epithelium, even when present in the stomach. Several important H. pylori adhesins have been identified, including the outer membrane proteins BabA (which binds to fucosylated Lewis b receptor on gastric epithelial cells), SabA (which binds to sialyl Lewis X receptors), HopQ (which binds to carcinoembryonic antigen-related cell adhesion molecules), AlpA, and AlpB.
The gastric tissue colonized by H. pylori almost always exhibits an inflammatory infiltrate. The lamina propria most commonly contains mononuclear cells, including lymphocytes, monocytes, and plasma cells. Neutrophils and, to a lesser extent, eosinophils may be present in the lamina propria and epithelium. The epithelial glands have a more complex architecture and less mucus when H. pylori is present than when it is absent. In children, a follicular lymphoid pattern is common. The presence of H. pylori induces these changes, and the bacterium is not just a secondary colonizer.
Persons colonized with H. pylori have different gastric secretory physiology than do those who are not colonized. On average, colonized persons have higher gastrin levels, which are reduced by eradication of the organism. The mechanism for increased gastrin production appears to be related to low gastric somatostatin levels, which may reflect cytokine production in the colonized antrum. Increased gastrin may contribute to the increase in parietal cell mass observed in many patients with duodenal ulceration. H. pylori products may directly affect parietal cells, which may diminish acid production. Effects of H. pylori on both the fundus (the site of acid production) and the antrum (which produces factors regulating acid production) may in part be responsible for the multiplicity of outcomes of colonization.
H. pylori does not appear to invade tissues, except as an incidental finding. Thus H. pylori –induced alterations in host tissue are likely a response to extracellular bacterial products or to cellular alterations induced by contact with the organism. Many of the alterations in gastric epithelial cells caused by H. pylori are attributable to CagA, which is secreted and translocated into cells through a type IV secretion system. The 3′ region of cagA contains DNA repeats flanking sites that encode tyrosine phosphorylation motifs. H. pylori populations include individual cells with zero, one, two, or more tyrosine phosphorylation motifs in CagA, which arise through intragenomic recombination. Once injected into the epithelium by the type IV secretion system, Src and Abl kinases phosphorylate these tyrosine residues, and phospho-CagA interacts with multiple intracellular regulatory molecules, including SHP-2 and PAR1b/MARK2, that affect mitogen-activated protein kinases and the actin cytoskeleton; these pathways affect cell shape, cell cycle events, and cytokine production. Nonphosphorylated CagA also can interact with cellular proteins, resulting in altered signaling events. Experiments in animal models indicate that CagA and the type IV secretion system contribute to gastric inflammation and, in some cases, can promote histologic changes that are linked to gastric cancer. The cag type IV secretion system contributes to the entry of heptose-1,7-bisphosphate (an intermediary metabolite of H. pylori lipopolysaccharide biosynthesis) into epithelial cells, which stimulates proinflammatory signaling. The cag island is metastable, and isolates in individual patients may vary in the presence of the island, specific genes or regions, or subgenic sequences, as in the case of the 3′ region of cagA. This instability creates a population of variants that can interact with the host in myriad ways.
Besides CagA, several other secreted or released H. pylori proteins are relevant. The secreted pore-forming protein VacA can cause several alterations in gastric epithelial cells (including alterations in endosomal compartments and cell death), and can also target several types of immune cells (T cells, B cells, mast cells, and macrophages). Certain forms of VacA (type s1) are active in cellular assays in vitro, whereas other forms of VacA (type s2) are inactive in these assays. T-cell activity is downregulated by both VacA and H. pylori γ-glutamyl transpeptidase; this downregulation may contribute to H. pylori persistence, as well as protection against allergic and asthmatic conditions. HtrA, a secreted protease, facilitates access of H. pylori to the basolateral surface of gastric epithelial cells. Urease may be shed by H. pylori cells, has been observed in affected tissues, and is a chemoattractant and activator of host phagocytic cells.
The presence of H. pylori overlying the gastric mucosa activates epithelial cells to produce proinflammatory cytokines and activates mononuclear and polymorphonuclear cells to produce cytokines, superoxide, and other proinflammatory molecules. Although H. pylori colonization of the stomach is consistently accompanied by an inflammatory gastric host response, several factors serve to downregulate host responses. Bacterial lipopolysaccharide usually has proinflammatory activities, but H. pylori lipopolysaccharide has remarkably little. Similarly, H. pylori flagellin is modified so that it is poorly recognized by Toll-like receptor 5 (TLR5). H. pylori lipopolysaccharide may express type II Lewis antigens (Le x , Le y , neither, or both of these antigens), as well as type I antigens (Le a , Le b ). This observation is significant because these antigens are present on gastric epithelial cells, and there is evidence that the host Lewis phenotype selects for the particular Lewis expression of the H. pylori population. This may represent a form of molecular mimicry that promotes H. pylori persistence. T-regulatory cells in the gastric mucosa may downregulate local inflammatory responses. Finally, H. pylori glucosylation of host-derived cholesterol contributes to immune evasion.
Both bacterial and host factors may be determinants of outcome. Virtually all patients with duodenal ulceration are colonized by strains possessing cagA (and thus the cag pathogenicity island). Similarly, cagA + strains have been associated with a higher risk of stomach cancer than cagA − strains. In East Asia, most H. pylori strains are cagA + , which may account for the relatively high incidence of gastric cancer in this part of the world. Strains from patients with ulcers or stomach cancer more commonly contain type s1 vacA and more frequently express the BabA adhesin compared with strains from patients without these diseases. Differences among colonized hosts in cell-mediated immunity and cytokine responses to H. pylori are other possible determinants of outcome variability. Humans are polymorphic in the genetic loci involved in regulating proinflammatory cytokine production, and allelic variation in genetic determinants of interleukin-1β and interleukin-10 production affects risk of gastric cancer in H. pylori –positive persons.
Findings similar to those observed in humans develop in several animal models of infection, including nonhuman primates and Mongolian gerbils. The development of experimental H. pylori infections in these models and in human volunteers has allowed new avenues for exploring host-microbe interactions.
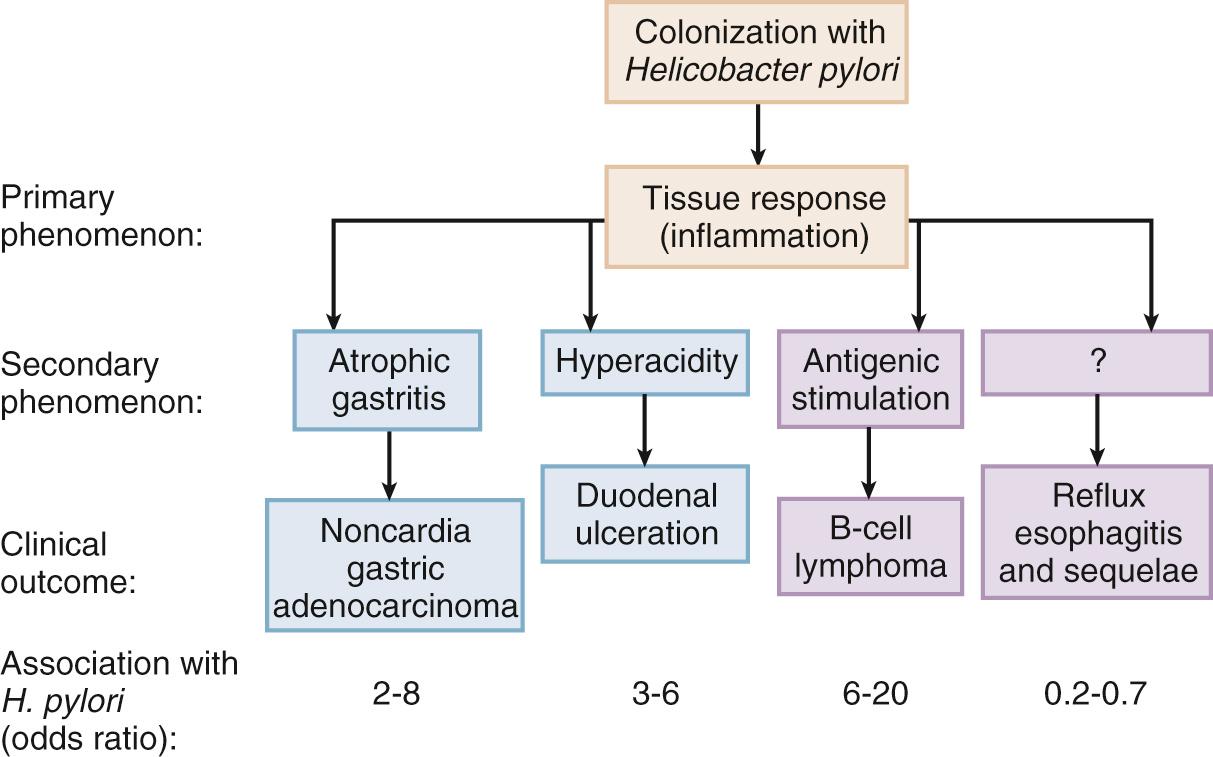
In the majority of H. pylori –colonized persons, the presence of this organism is not associated with any readily identifiable clinical consequences. Nevertheless, colonization is associated with certain types of upper gastrointestinal pathology, and appears to protect against other diseases ( Table 217.2 ). From a clinical standpoint, the major consequences of H. pylori colonization are as follows.
| LESION | ASSOCIATION WITH H. PYLORI |
|---|---|
| Chronic diffuse superficial gastritis | Nearly always associated |
| Type A (pernicious anemia) gastritis | Negative association |
| NSAID gastropathy | Negative or no association |
| Acute erosive gastritis (e.g., alcohol, aspirin) | No association |
| Gastric ulceration | Commonly observed in patients who are not ingesting NSAIDs or aspirin |
| Duodenal ulceration | Usually associated with idiopathic lesions (non–drug induced, non–Zollinger-Ellison syndrome) |
| Gastric adenocarcinoma | Positively associated with (noncardia) cancers of the gastric body and antrum |
| Gastric lymphoma | Strongly associated with MALT-type B-cell lymphomas |
| Idiopathic thrombocytopenic purpura | Often associated |
| Nonulcer dyspepsia | Little or no association |
| Gastroesophageal reflux disease | Presence of cag + strains has protective association |
| Barrett's esophagus | May colonize distalmost gastric epithelium in patients with gastric colonization ; presence of cag + strains has protective association |
| Adenocarcinoma of the esophagus | Presence of cag + strains has protective association |
| Childhood asthma and related allergic disorders (allergic rhinitis, eczema, and skin sensitization) | Presence of cag + strains has protective association |
Natural, voluntary, or accidental H. pylori acquisition may cause an acute upper gastrointestinal illness with nausea and upper abdominal pain. Vomiting, burping, and fever may also be present. Symptoms last from 3 to 14 days, with most illnesses persisting less than 1 week. A diagnosis of food poisoning may be made in persons seeking medical attention. For many individuals, the acquisition of H. pylori is clinically silent. Most data suggesting symptomatic acquisition relate to adults, but worldwide, most acquisition actually occurs in children ; the relative proportion of symptomatic and asymptomatic acute acquisition at any age is not known. In the weeks after acquisition, intense gastritis develops; hypochlorhydria ensues and may persist for as long as 1 year. In children, there is a transient increase in serum pepsinogen I levels. One adult volunteer who ingested H. pylori seemed to have had an acute self-limited infection ; the frequency of this phenomenon is not known.
It now is clear that, after acquisition, H. pylori persists for years, if not decades, in most persons ( Fig. 217.2 ). Not every exposure to H. pylori leads to persistent colonization, because of either lack of adaptation to the particular host or coincident or proximate use of antibiotics. Tissue and serologic responses to colonization develop in essentially all persistently colonized persons. The acute H. pylori –induced upper gastrointestinal symptoms resolve and do not return in most persons; most with persistent H. pylori colonization are asymptomatic. However, studies of patients with nonulcer dyspepsia indicate that H. pylori may be slightly more common in such patients than in age-matched control subjects and that H. pylori colonization may be one of the causes of this common but poorly defined and heterogeneous group of disorders. Supporting this hypothesis are the results of some studies indicating that some patients with nonulcer dyspepsia who are colonized with H. pylori show better responses to antimicrobial therapy than treatment with placebo, an effect not seen in patients with nonulcer dyspepsia who do not have H. pylori colonization. However, in other studies, no difference between H. pylori treatment and placebo was found. In total, H. pylori is probably responsible for fewer than 10% of cases of nonulcer dyspepsia. Even if such an association exists, no markers are available to identify those patients with nonulcer dyspepsia in whom antibiotics would have a beneficial effect. Better definition of nonulcer dyspepsia and ascertainment of both H. pylori and host genotypes in individual patients should lead to a better understanding of whether H. pylori persistence is associated with symptoms in particular patients in the absence of ulceration or neoplasia.
More than 90% of patients with “idiopathic” duodenal ulceration (i.e., not associated with nonsteroidal antiinflammatory drug use or Zollinger-Ellison syndrome) carry H. pylori, a prevalence significantly higher than in age-matched control subjects. Previous H. pylori colonization is associated with a three- to fourfold increased risk of development of duodenal ulceration, and the risk is even higher in patients colonized with cagA + strains.
H. pylori may colonize the duodenum but only overlies metaplastic islands of gastric-type epithelium (gastric metaplasia). The occurrence of H. pylori colonization and gastric metaplasia is highly associated with active duodenitis, a precursor lesion to ulceration, and the presence of H. pylori in the duodenum is associated with a markedly increased risk of duodenal ulceration. One model proposes that H. pylori –induced hypergastrinemia results in increased acid production, which leads to the development of gastric metaplasia in the duodenum; H. pylori colonization of the metaplastic gastric tissue then results in duodenitis and ulceration.
Although a significant body of evidence associating H. pylori colonization with idiopathic duodenal ulceration has accumulated, a causative role of H. pylori in ulcer disease is unproven; none of the experimental human studies has shown progression to ulceration, and why peptic ulcer disease has a remitting and relapsing course in the face of persistent colonization has never been resolved. However, a large number of treatment studies using antimicrobial agents have helped define the natural history of ulcer disease. First, the use of antimicrobial agents (in the absence of acid-suppressive therapy) can heal duodenal ulcers at a rate similar to that observed with acid-suppressive therapy alone. Second, after ulcer healing, eradication of H. pylori is associated with significantly lower recurrence rates than if the organism remains present. When antimicrobial therapy that eradicates H. pylori is added to short-term acid-suppressive therapy, long-term ulcer relapse rates are markedly reduced, although not completely eliminated. Altogether, these findings implicate H. pylori as playing a role in duodenal ulcer pathogenesis and demonstrate that antimicrobial therapy rather than long-term acid-suppressive therapy is indicated for most patients because it changes the natural history of idiopathic duodenal ulcer disease. Recent studies have provided evidence that, after H. pylori eradication, the incidence of reflux esophagitis is doubled compared with the reflux incidence associated with failed eradication. Thus, removal of H. pylori from the stomach of patients with duodenal ulceration has both benefits and costs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here