Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Flexor tendon injuries treated with optimal repair techniques may benefit from an early active motion regimen utilizing short arc active flexion exercises initiated within the first postoperative week.
The use of a relative motion extension orthosis has become the standard of care for the treatment of extensor tendon repairs with evidence to support earlier functional hand use and return to work.
Fracture management has shifted toward early mobilization during the initial phases of fracture healing using custom orthoses and safe parameters of motion.
Sensory and motor re-education following nerve injury are directed at strengthening and reinforcing the new and altered neural pathways in the sensory and motor cortex.
A replanted digit will be considered viable after the first 7–10 days after surgery. The therapist must consider the nature of the injury, fracture fixation, quality of tendon and nerve repair, soft tissue, and vascular involvement to manage these complex injuries safely and successfully.
Access video content for this chapter online at Elsevier eBooks+ ![]()
As defined by the American Society of Hand Therapists (ASHT), the practice of hand therapy embodies the art and science of evaluating and treating injuries and conditions of the upper extremity through therapeutic interventions to help return a person to their highest level of function. A hand therapist evaluates and treats any condition related to the upper extremity, optimally, in collaboration with the treating surgeon. This chapter aims to provide an overview to upper extremity surgeons of the approaches used by hand therapists for the treatment of patients with upper extremity nerve, musculotendinous, vascular, ligamentous, and skeletal conditions.
The International Classification of Functioning, Disability and Health (ICF) uses a conceptual model for evaluating the impact of all health states on the individual. These interrelated domains of focus include body functions and structures; activity and performance; and environmental influences. For both the surgeon and hand therapist, the use of occupation-based and impairment-based assessments encompass these areas of focus and serve as the foundation for the informed decision-making that guides treatment.
Occupation-based assessments are self-reported health questionnaires that describe “occupations” as the tasks people need to do, want to do, and are expected to do. A survey of hand therapists identified practice trends of assessments most commonly used in hand therapy settings. The most frequently used occupation-based assessments included activities of daily living (ADL) assessments, described as an informal interview at the time of the evaluation, and the Quick Disability of Arm, Shoulder, Hand Questionnaire (QuickDASH). Other assessments commonly used by hand therapists include the Patient Rated Wrist and Hand Evaluation (PRWHE) and the Patient Specific Functional Scale (PSFS).
Impairments are defined as dysfunction or significant structural abnormality within a specific body part or system. Evaluation of biomedical impairments include the evaluation of pain, edema, wound, vascularity, sensation, range of motion, and strength. Although impairment does not correspond precisely with disability, decreasing impairment can be helpful in decreasing disability. In order to treat each of these impairment domains, one must understand how they are evaluated.
Pain is frequently rated on four types of scales: numerical scales, visual analog scales, verbal rating scales, and the FACES pain rating scale. Although designed as a measure of intensity, these pain ratings reflect more than just the magnitude of pain and are likely influenced by the patient’s pain beliefs, catastrophizing and/or pain interference.
The criterion standard for measuring hand and wrist edema is water volumetry. Although this technique is both reliable and valid, it is time consuming and can be difficult to perform. The figure-of-eight technique has gained popularity due to its ease of use and excellent intra- and inter-rater reliability. This method, modeled after the method described by Esterson and colleagues, involves the use of a tape measure wrapped around specific landmarks on the hand and wrist in order to assess size and compares this value to the patient’s contralateral or non-involved extremity ( Fig. 43.1 ).

Sensation testing is used to determine the status and degree of potential injury to each of the three peripheral nerves in the hand. The Semmes Weinstein Monofilament Test is a widely used threshold test performed with the examiner applying graded monofilaments to the involved dermatome until one is detected by the patient. Strauch’s Ten Test was developed as a more rapid and simple evaluation tool that requires no instrumentation and is administered by the examiner lightly touching the test area and simultaneously comparing that with a known unaffected area. The test is based on a 10-point numeric scale stimulus rating in relation to normal sensitivity and has been shown to have both good inter- and intra-rater reliability. The two-point discrimination (2PD) test is another widely used assessment of hand sensibility. It may be used as a quick test of normal versus abnormal sensibility, though it has been found to lack sensitivity for early detection of nerve entrapment.
Range of motion (ROM) is frequently used to assist in assessing the presence or absence of pathology, to establish a baseline for treatment planning, evaluate the effects of therapeutic interventions, and as an outcome measure for research. The ASHT recommends optimal standard testing positions and documentation criteria to create consistency among practitioners. Established methods of measurement of hand ROM include visual estimation, goniometry, and composite finger flexion to distal palmar crease (DPC). Given that visual estimation has been shown to be less reliable, goniometry has become an essential component to any musculoskeletal evaluation. Composite finger flexion may also be used if multiple joints are involved ( Fig. 43.2 ). Standard goniometry and the measurement of composite finger flexion have been shown to have good inter-rater reliability.

Grip strength has been widely used as an indicator for overall muscle strength and as a measure of hand function. The ASHT recommends the use of the Jamar dynamometer in the second handle position be used when evaluating grip strength and further clarifies that patients should be seated with the shoulder adducted and in neutral rotation, the elbow flexed to 90° and the forearm and wrist in neutral position. Established normative data for grip strength in healthy adults in the United States demonstrate that the dominant hand possesses a 10% greater grip strength than the non-dominant hand in healthy subjects when the right-hand is dominant. Dynamometer measurements assist therapists and surgeons with clinical decision-making, particularly in the realm of appropriate timing for return to activities such as weight-bearing, return to work, and return to sport.
Collaboration between the surgeon and therapist is imperative for maximizing patient outcomes in the treatment of upper extremity injuries and conditions.
Occupation and impairment-based outcome measures are used at the time of evaluation and throughout treatment to evaluate the impact of therapeutic interventions and provide objective comparisons for determining progress.
Occupation-based assessments, such as the QuickDASH, evaluate the ability of a patient to perform their meaningful and purposeful activities. Impairment-based measures, such as pain, ROM, and grip strength, identify an abnormality in a specific body part or system.
There is limited correlation between impairment and disability. Understanding of the patient’s goals and collaboration between the patient, therapist, and surgeon is crucial for maximizing patient outcomes.
Rehabilitation following extensor tendon injury is largely guided by the zone of injury and the anatomy and biomech-anics of the extensor mechanism in each zone ( Fig. 43.3 ). A zone I injury, referred to as a mallet injury, presents as the inability to extend the distal interphalangeal (DIP) joint of the finger due to detachment of the terminal tendon. This injury can be the result of soft-tissue rupture or avulsion of the extensor tendon along with a small fragment of bone. Terminal tendon excursion during full DIP joint motion is between 1 and 2 mm for all digits. Due to this small amount of excursion, as little as 1 mm of terminal tendon lengthening can result in 25° of DIP joint extension lag which may correlate with clinical disability.
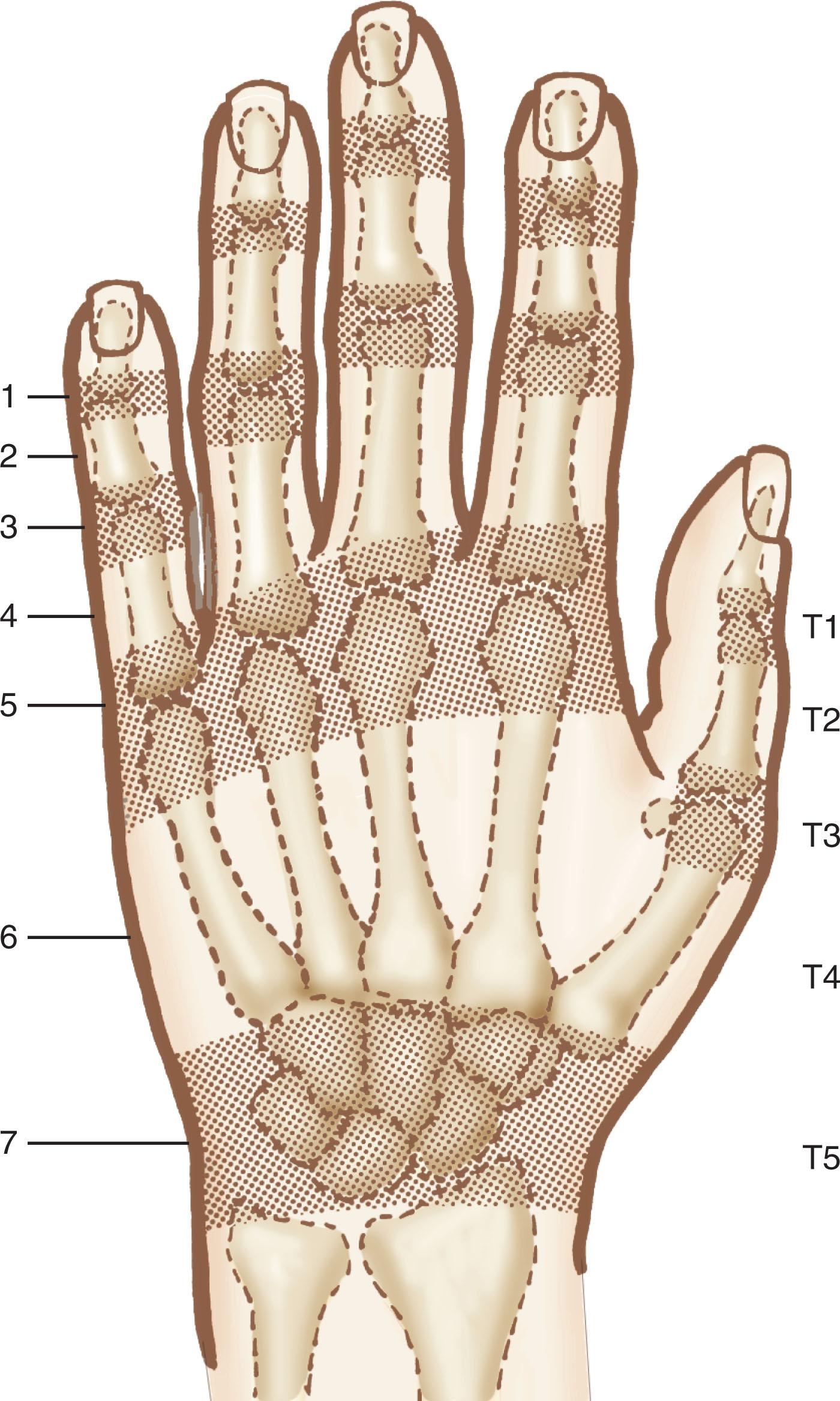
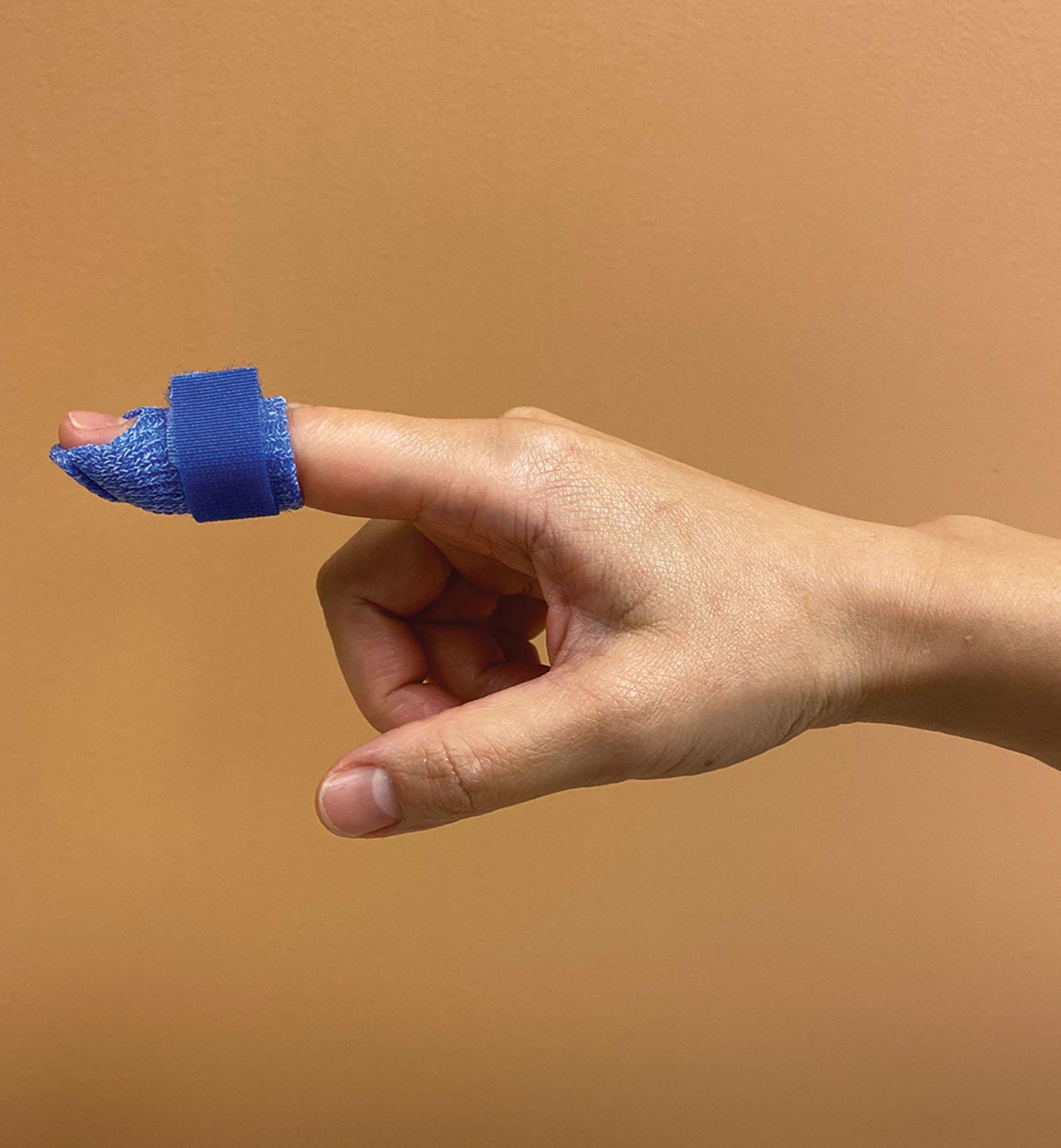
Although both surgical and non-surgical treatment of mallet finger injuries can lead to excellent clinical outcomes, immobilization is the treatment of choice in uncomplicated cases. Patients are placed in an orthosis that holds the DIP joint in neutral or slight hyperextension continuously for 6–8 weeks, with the proximal interphalangeal (PIP) joint free to prevent stiffness ( Fig. 43.4 ). After that time, patients may be advised to continue with nighttime immobilization for up to 4 additional weeks. Many studies have compared various orthoses for the management of mallet injuries though there has been no conclusive evidence to support one type over another. In a study comparing three different orthoses – stack, dorsal aluminum, and custom thermoplastic – no difference in extensor lag was identified based on orthosis type, however, the custom orthosis was less likely to result in complications. Although the type of orthosis may not significantly impact lag difference, patient compliance in wearing the orthosis has been shown to affect outcome in the treatment of these injuries.
Extensor zone III/IV injuries have been reported to result in the highest percentage of fair to poor outcomes. In zone III injuries, compromise of the central slip often results in a boutonnière deformity. These injuries can be difficult to diagnose as patients may initially present with full ROM if some amount of the extensor hood is still intact. It is not until the lumbricals attenuate that the PIP joint may fall into a flexion deformity, hyperextending the DIP joint. Once the deformity presents, it can be difficult to treat. Historically, when treated nonoperatively patients are immobilized for 3–6 weeks with the PIP joint in extension, the DIP joint, metacarpophalangeal (MCP) joint, and wrist joints free. This may be followed by 6 more weeks of nighttime extension immobilization. Patients are instructed in active flexion exercises of the DIP joint while holding the PIP joint in extension to promote retraction of the lateral bands dorsally from a volarly subluxed position.
Although immobilization is widely used, both Evans and Merritt advocate for early motion orthosis-based therapy in the treatment of chronic boutonnière injuries and those undergoing acute repair. Evans et al . found that patients treated with an early active short arc motion protocol had better outcomes than those treated with immobilization. This protocol, initiated within 48 hours after surgical repair, uses a template orthosis that allows PIP joint flexion up to 30° and DIP joint flexion up to 25°. The patient is placed in full PIP joint extension with the DIP joint free at all other times. While this short arc motion protocol continues to be widely used, it requires strict patient compliance and a long course of therapy. Merritt advocates for use of the relative motion flexion (RMF) orthosis to treat boutonnière deformities following surgical repair or closed treatment. The injured digit is placed in 15–20° greater MCP joint flexion than their neighboring digits for 6 weeks and otherwise permits full active range of motion (AROM) and functional hand use. For a fixed-chronic boutonnière, serial casting is first implemented in order to obtain as much PIP extension as possible (at least −20°) and is followed with the RMF orthosis for 12 weeks.
Zone V injuries, which involve the sagittal bands, commonly occur from a human bite, an open laceration, or a closed rupture. When treated with immobilization, the digits are positioned with the MCP joint in static extension and IP joints free ( Fig. 43.5 ). While conventional postoperative management in this zone has been to immobilize for 4–6 weeks, early active motion has become the standard of care across many institutions to limit the loss of flexion that often results from prolonged immobilization in extension.

In a recent international survey, hand therapists selected the relative motion extension (RME) orthosis, commonly referred to as a yoke splint, as the “most used” approach for postoperative management of zones V and VI extensor tendon repairs. The RME orthosis is described as a part of the Immediate Controlled Active Motion (ICAM) program, which provides a timeline for managing orthosis wear for zone IV–VII injuries. Initially the patient is placed in the RME orthosis continuously, with or without a wrist orthosis, and instructed to move through full ROM within the confines of the orthosis. If used, the wrist orthosis can be discontinued at 3 weeks post surgery, and the RME orthosis discontinued by 6 weeks post surgery ( ![]() ) ( Fig. 43.6 ).
) ( Fig. 43.6 ).
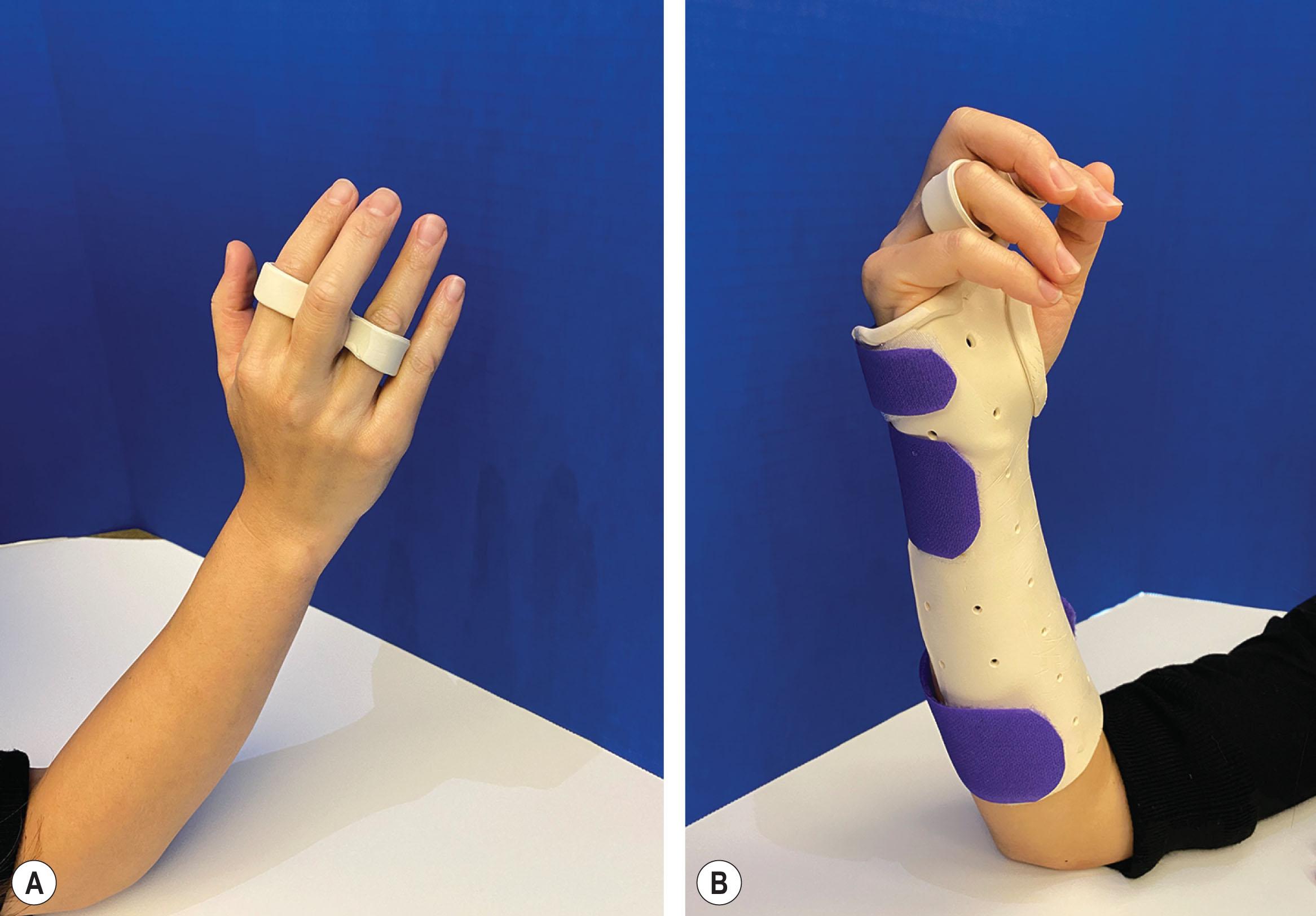
Traditionally, the wrist orthosis was considered essential to protect repairs in this zone; however, more recent evidence has challenged the need for wrist immobilization and has supported the use of the RME orthosis alone. A survey by Hirth et al . has suggested that it may be possible for zone V and VI injuries to be managed safely using the RME orthosis only. Their paper reviewed four studies involving zone V and VI extensor tendon repairs in which the RME orthosis was the only orthosis used postoperatively and resulted in good–excellent ROM outcomes without tendon ruptures. Surgeon preference, quality of repair and patient factors should be considered in determining if the wrist component is necessary for repairs in this zone.
The extensor pollicis longus (EPL) tendon is prone to rupture over the distal end of the radius secondary to a distal radius fracture, rheumatoid arthritis, direct injury or chronic attrition. Rupture of this tendon may be missed at time of evaluation. If the EPL tendon is ruptured, the abductor pollicis longus (APL), abductor pollicis brevis (APB), and flexor pollicis brevis (FPB) as well as extensor pollicis brevis (EPB) are all capable of producing weak extension of the IP joint, leading a clinician to mistakenly conclude that the EPL is intact. To more accurately isolate the EPL tendon, the patient is asked to place their palm flat on the table and attempt to extend the thumb up off the table (retropulsion). The examiner can palpate and sometimes visualize the EPL tendon ulnar to the EPB tendon and confirm that the IP joint is being extended. The examiner can then ask the patient to resist IP joint extension. Of note, patients may develop a pseudotendon in the setting of an attritional EPL rupture which may also contribute to some isolated IP joint extension, though this is frequently weaker when compared to the contralateral side. When identified in the acute setting, these injuries may be treated with primary repair. In a more chronic setting, these injuries are often treated with tendon grafting or tendon transfers, with the most common being the transfer of the extensor indicis proprius (EIP) tendon to the EPL stump. While there is some literature supporting early active motion following these tendon transfers, patients are typically immobilized for 3-4 weeks in a forearm-based thumb spica orthosis, with the wrist in neutral and the thumb in abduction and extension. Gentle progressive active motion is started after this time.
Uncomplicated mallet injuries are best treated with continuous immobilization in DIP joint extension. There is limited evidence demonstrating superiority of one orthosis over another; however, compliance with orthosis wear affects outcome and the clinician must consider what orthosis may be best tolerated.
There is growing support in the literature and clinical practice for treating both chronic and acute zone III boutonnière injuries with an early mobilization program, such as Evans’ short arc motion protocol or Merritt’s RMF orthosis.
Treatment for zone V–VII injury has shifted away from continuous MCP joint immobilization towards an ICAM protocol using the RME orthosis, with or without wrist immobilization.
Due to the dorsal extensor expansion contributing to thumb IP extension, thumb EPL ruptures can be missed. Once identified, they often require a tendon transfer with EIP to EPL being the most common, followed by a short course of immobilization and progressive active mobilization.
The study of flexor tendon injury continues to be an area of robust academic and clinical research as advancements in surgical repair guide advancements in rehabilitation. Following a strong multistrand repair, the selection of an appropriate rehabilitation regimen has the potential to minimize extrinsic adhesion formation, optimize tendon glide, and maximize motion and function of the hand.
An ideal postoperative therapy program would create the greatest amount of tendon excursion with the lowest force on the healing tendon to minimize adhesion formation, gapping, and rupture. With these goals in mind, current flexor tendon rehabilitation management should take into consideration the timing for initiating tendon mobilization, the effect of wrist positioning on tendon gliding force and excursion, and the application of early active tension on the repaired tendon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here