Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The authors would like to thank the contributions of authors of previous editions of this chapter to the development of this text: John A. Barnard and Kirk M. McHugh (4th ed.), and John F. Kuemmerle (5th ed.).
Gastrointestinal (GI) tissues express a multitude of growth factors, broadly defined as naturally occurring polypeptides that elicit cellular growth, proliferation, or differentiation following binding to surface membrane receptors. The growth factor field arguably took root in the 1950s and 1960s with the identification of a number of soluble biological activities necessary to drive cell division. Over subsequent decades, many additional molecules were identified by efforts to find mediators involved in the transformation of normal cells to tumor cells (which characteristically display rapid proliferation and enhanced survival). These early findings laid the groundwork for a wealth of subsequent studies identifying mechanisms of growth factor secretion, receptors, modes of signaling, downstream pathways, and additional ligands that cosignal within each family. In the GI tract, growth factors perform functions at all stages of life and play critical roles in development, maintenance, repair and regeneration, pro- and anticancer functions, and immune cell regulation. In this chapter, we review several families of growth factors that have well defined and significant roles in the GI tract: epidermal growth factor (EGF), transforming growth factor beta (TGF-β), insulin-like growth factor (IGF), hepatocyte growth factor (HGF), and fibroblast growth factor (FGF). We will also briefly discuss several other families with less well defined but emerging roles in the GI tract. An overview of these growth factors, their principal receptors, and targets of actions are listed in Table 3.1 .
| Growth Factor Family | Receptors | Ligands | Target Cell Types |
|---|---|---|---|
| Epidermal growth factor | EGFR/ErbB1 | EGF, TGF-α, NRG1-4, HB-EGF, amphiregulin, betacellulin, epiregulin, epigen | Epithelium |
| ErbB2 | Endothelium | ||
| ErbB3 | Immune | ||
| ErbB4 | |||
| Transforming growth factor-β | TβR-I | TGF-β, BMP2-7, activin, inhibin, nodal | Epithelium |
| TβR-II | Endothelium | ||
| Immune | |||
| Insulin-like growth factor | IGFR1 | IGF1 | Epithelium |
| IGFR2 | IGF2 | Endothelium | |
| Hepatocyte growth factor | c-Met | HGF | Epithelium |
| Coreceptors (CD44) | Endothelium | ||
| Mesenchyme | |||
| Immune | |||
| Fibroblast growth factor | FGFR1-4 | FGF1, 2, 4, 7, 9, 10, 15/19, 18, 21, 20 (in cancer), 23 | Epithelium |
| Coreceptors (α/β-klotho) | Mesenchyme | ||
| Trefoil factor | CXCR4 | TFF1, TFF2, TFF3 | Epithelium |
| Unidentified others | Immune | ||
| Hedgehog | Ptch1-2 | Shh, Ihh, Dhh | Epithelium |
| Immune |
The naming convention of peptide growth factors typically has relied upon the molecule’s apparent function when initially discovered. While this seems straightforward, subsequent research has invariably identified additional and sometimes even contradictory roles for these peptides; a growth factor may elicit a wholly distinct function than what the name would suggest depending on tissue location and context of expression. For instance, EGF has pleiotropic actions in many tissues including but not limited to the epidermis, and some EGF family members can have seemingly “nongrowth” activities such as promoting apoptosis or regulating ion transport. Transforming growth factor (TGF)-β has roles outside of transformation of normal cells, including wound healing, differentiation, and fibrosis, and in many settings actually acts as a tumor suppressor. Furthermore, though TGF-β and TGF-α have names that would suggest close relatives, they in fact belong to entirely different families of growth factors—TGF-β is the prototypic member of a whole family (the TGF-β superfamily), while TGF-α is an EGF-like molecule. Thus, the reader is cautioned against drawing too many conclusions regarding a peptide’s function from its name.
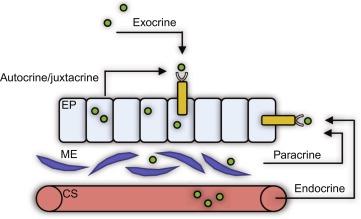
Although other classes of proteins such as cytokines/chemokines and peptide hormones can stimulate cellular growth; in this chapter, we will focus strictly on the traditional peptide growth factors. Cytokines can impact cell growth as a secondary outcome but in general tend to be immunomodulatory in function. Hormones are generated in glandular tissue and are typically secreted into circulation thus allowing for long-range actions. In contrast, peptide growth factors are sourced from a variety of cell types and tissues and are typically categorized as having autocrine, paracrine, or juxtacrine actions ( Fig. 3.1 ). Cytokines, chemokines, hormones, and similar molecules are covered in other chapters.
Growth factor signaling in the GI tract is tightly regulated, in part due to the varied sources and targets of these peptides. It is important to keep in mind the ligand source and receptor location to understand fully differences in signaling outcomes. Growth factors are produced in a variety of tissues and histological strata including the epithelium, the subepithelium, exogenous sources such as breastmilk, and anatomically distinct sources (i.e., luminal EGF secreted from salivary and Brunner’s glands ). In some instances, notably with TGF-β and IGF, the source of growth factor can also be from recruited immune cells. Signaling specificity is supported by restricted or differential receptor expression on different cell types, including epithelial cells, endothelial cells, mesenchyme/fibroblasts, smooth muscle cells, and immune cells, among others. Regulated induction or suppression of ligand and receptor levels (e.g., Refs. ) can alter the responses of specific cell types or the overall tissue as well. Substantial work on each family of molecules in the past half century has revealed specific signaling pathways and alterations in intracellular activity that are stimulated by these growth factors. As some of these signaling pathways and intracellular events are shared, it is important to keep in mind the source(s) of ligands as well as expression patterns of the target receptors in understanding the context-dependent roles and specific outcomes.
Signaling initiated by growth factors occurs through a sequence involving ligand release (or presentation of tethered ligand) and extracellular binding to receptor; recognition of this event is then transmitted to intracellular signals through a variety of methods (predominantly, but not exclusively, kinase activity). Generally, a number of ligands can act through the same receptor. This initially was interpreted as a functional redundancy, but in the past few decades, it has become clear that while there is substantial overlap between shared ligands, conformational and contextual (including spatial and kinetic) differences in responses also come into play that finely tune the output. Thus, availability of a panel of highly similar but not quite identical ligands allows for greater flexibility in control of cell behavior. A significant amount of effort has gone into clarifying these aspects of growth factors in the GI tract, resulting in an evolving understanding of the physiological roles of closely related growth factors, but to a large extent this aspect of the field is still in its infancy. The spatial distinctions, differences in expression, and compartmentalization of related growth factors that share common receptors should be kept in mind when interpreting how the growth factor may function in vivo. These differences and any known implications for physiological function will be discussed within each subsection.
The groundwork laid in understanding the activity and function of peptide growth factors in cell culture was instrumental for determining the role of many of these molecules in maintenance of tissue homeostasis. Furthermore, understanding their activity has allowed us to recognize cases where inappropriate gain- or loss-of-function is involved in the development of disease. At the same time, understanding the basic biology and biochemistry of these molecules has allowed for harnessing this knowledge to advance therapeutics and disease treatment. For instance, in mouse models, a number of growth factors are dispensable for normal homeostatic maintenance/tissue turnover but absolutely required for appropriate and efficient response to injury and inflammation. In other cases, overexpression or lack of expression of growth factor signaling can result in profound baseline GI disturbances, implicating specific factors in tissue homeostasis, and in several cases are associated with disease states such as cancer.
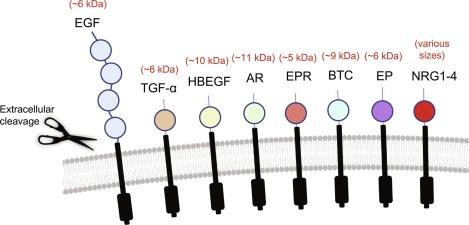
The EGF family is a large group of peptide growth factors that, through activating one or more of the ErbB receptor tyrosine kinases ( Fig. 3.2 ), influence cell proliferation, differentiation, migration, function, and survival in the GI tract. EGF, the prototypic member of this family, was initially described in 1962 as a protein in mouse submaxillary gland extracts that promoted premature eye opening and incisor eruption in newborn mice. Decades of subsequent study on this “tooth-lid factor” have demonstrated critical roles for EGF and its relatives in most cell types in the body. The EGF family has expanded to include additional peptides including TGF-α, heparin-binding EGF-like growth factor (HB-EGF), heregulins/neuregulins (HRG/NRG), amphiregulin (AR), betacellulin (BTC), epiregulin (EPR), and epigen (for review, see Refs. ). These molecules share substantial sequence homology and, with varying degrees of affinity, the same receptors. Thus, they evoke overlapping but not completely identical biological activities, with differential receptor binding providing a first layer of explanation for the differences.
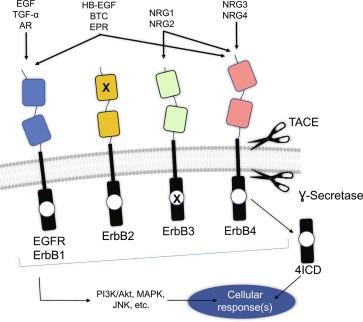
Each EGF family member is synthesized as an integral membrane protein with functionally distinct cytoplasmic, transmembrane, and extracellular domains and typically harbor extracellular proteolytic cleavage sites for processing by distinct members of the “a disintegrin and metalloproteinase” (ADAM) family of sheddases ( Fig. 3.3 ). Following cleavage and processing, EGF-like peptides bind and activate EGFR, ErbB3, and ErbB4. A fourth receptor, ErbB2, is involved in transducing signals from these ligands but does not appear to bind them directly. The receptors were named ErbBs due to their close homology with the v-erbB oncogene encoded by the avian erythroblastosis virus. Alternatively, they are also known as human epidermal growth factor receptor 1-4 (HER1-4). The choice of naming of these receptors in the literature is largely a factor of historical convention within the field of study—for instance, the breast cancer field typically relies on using the HER naming strategy, whereas the GI field generally uses the EGFR/ErbB names. Regardless of the name, upon ligand binding, the receptors are typically stabilized in homodimers (two of the same receptor) or heterodimers (two different ErbBs), leading to increased tyrosine kinase activity, transphosphorylation of the kinase cytoplasmic domain, and presentation of tyrosine-phosphorylated docking sites for downstream signaling adapters and substrates.
Signaling through ErbB/HER receptors is complex, allowing for fine regulation of cellular outcome. A common component of ligand-induced signaling that is recurrent in growth factor biology is receptor dimerization. Within the EGFR/ErbB family, the number of ligands (each with individual affinity profiles for the different receptors), combined with the number of potential receptor dimers, allows for substantial diversity in cellular outcomes. For example, ErbB3 has very low kinase activity, while ErbB2 has no known ligand and typically functions in heterodimers. Furthermore, each receptor has a distinct pattern of c-terminal docking sites for downstream signaling, and different ligands can preferentially stabilize different dimer combinations to elicit different cellular effects. Thus, while signaling through these receptors can clearly have profound effects on cell growth and wound repair in the gut, the family can be “reused” with slight variations to control other cellular functions such as ion transport and differentiation.
The study of EGF over the past half century has been foundational for our modern day understanding of classical ligand-receptor activation and signaling paradigms within the field of molecular and cellular biology. The importance of this body of work was underscored in 1987 when the Nobel Prize was awarded to Stanley Cohen and Rita Levi-Montalcini for the discovery of EGF and nerve growth factor. In the GI tract, EGF is produced in multiple compartments including the salivary glands, intestine, stomach, esophagus, and accessory organs (pancreas and liver). EGF elicits its classical mitogenic effects by binding EGFR on the cell surface, leading to receptor dimerization and tyrosine kinase activity. It is mainly exclusive to EGFR homodimers and EGFR/ErbB2 heterodimers in terms of binding affinity, though low binding to ErbB2/4 dimers has also been reported. Heterodimer activity can be important as asymmetric dimers not only have a broader palette of intracellular docking sites but can also be “biased” toward different ligands and have different internalization-downregulation profiles after activation. Following receptor binding and dimerization, phosphorylation of specific c-terminal tyrosine residues activates signals through a wide array of pathways including ERK MAPK, p38 MAPK, JNK, and PI 3-kinase, resulting in numerous context-dependent cellular outcomes including altered DNA synthesis, intracellular calcium influx, glycolysis, and selective regulation of gene and protein expression.
Sources of secreted EGF in the GI tract include the submaxillary glands and the Brunner’s glands of the duodenum. Both of these sources result in luminal secretion. This is important to note because EGFR is expressed predominantly on the basolateral surface of the intestinal epithelium. Thus, utilizing the luminal pool of EGF requires that the ligand somehow cross the barrier. This originally led to the hypothesis that EGF is a luminal surveillance factor, poised to react to injured mucosa (where the barrier is naturally broken) by stimulating cellular proliferation, migration, and repair. In adults, transepithelial migration of EGF does not readily occur; therefore, luminal EGF is primarily available to pass the barrier when it is breached to promote epithelial wound repair as well as interact with other cells expressing EGFR such as immune cells. Alternatively, there is some evidence for EGFR redistribution to the apical face of enterocytes after injury. However, EGF can also be induced in subepithelial myofibroblasts, and it is released by the Paneth cells near the small intestinal crypt base. This may establish a gradient of available EGF along the crypt-villus (crypt-surface mucosa in the colon) axis in homeostatic turnover, which is then disrupted by injury. Furthermore, the expression of EGF in ulcer associated epithelial cell lineages suggests it can be produced locally throughout the intestine in response to chronic damage. Interestingly, another route through which EGF can access the GI tract in early life is through breast-feeding, as mother’s milk has been shown to be a major source. This suggests EGF has a role in development and maintenance of the intestinal epithelium in this sensitive early period of life, consistent with pig models of development in which weaning-associated villus atrophy can be prevented, and growth curves enhanced, by supplying EGF.
Among other functions in the intestinal epithelium, EGF stimulates cell migration and restitution, increases proliferation, delays intestinal cell shedding, and modulates nutrient and ion transport. EGF infusion or administration results in elevated epithelial cell proliferation, increased small intestinal villi size, and increased intestinal diameter. Additionally, it has been shown to have important roles in the regulation of the intestinal stem cell niche. This role of EGF in maintaining the stem cell niche is highlighted by its requirement in cultures of self-organizing 3D cultures of intestinal mini-guts, known as enteroids, and gastric organoids.
The pleiotropic responses to EGF signaling are of course tightly regulated, both at the cellular and tissue levels. At the most basic level, EGFR activation at the cell surface triggers receptor endocytosis and either recycling or destruction of the receptor depending on strength and duration of signal (for review, see Ref. ); interruption of the internalization-ubiquitinylation-degradation sequence can have profound effects on cellular growth. Additional physiologic feedback loops on ligand expression and availability present another level of control. For example, in the stomach, EGF is digested by gastric acid to less active forms, while EGF also serves to inhibit gastric acid secretion. In the intestine, EGF can induce other ErbB ligands and can itself be negatively regulated by inflammatory cytokines. Multiple reciprocal feedback mechanisms allow for fine tuning of the signaling response and attendant proliferation, wound healing, and other homeostatic activities.
Many examples of enhanced EGF expression or signaling have been demonstrated following an insult to the GI mucosa or in context of disease. In general, these studies identify induction as a cytoprotective response contributing to restoration of health and homeostasis. In rat studies, intraperitoneal injection of EGF (which would have basolateral access to EGFR) conferred protection of the small intestinal mucosa against methotrexate-induced injury. In liver, following partial hepatectomy and in cirrhosis, EGF expression is induced and important for hepatic regeneration. In chronic intestinal inflammation, EGF expression is elevated in the ulcer associated cell lineages, which may contribute to epithelial restitution and repair. Under pathological conditions, EGF has been shown to attenuate intestinal damage and enhance mucosal healing. Animal model results showing that EGFR gain- or loss-of-function are protective or sensitizing to intestinal injury, respectively, strongly support a role for EGF in driving resolution of colitis. In fact, in a limited clinical trial with mild-to-moderate ulcerative colitis patients, the Playford group demonstrated an impressive 83% response rate, including enhanced mucosal healing, to EGF when given as an adjunct to mesalamine.
In addition to studies of adult disease, work with administration to neonatal rodent pups has suggested that proper EGF signaling may be important in the prevention of neonatal intestinal inflammatory disease, such as necrotizing enterocolitis (NEC). Animals receiving EGF are protected from the formula feed-hypoxia model of NEC. This is presumably through suppressing epithelial apoptosis and encouraging rapid and efficient healing of epithelial damage, though secondary actions by other environmental factors such as bile acid pools may also contribute. These findings are also supported by some limited NEC work in human trials and have led to the hypothesis that lack of this growth factor (normally available in expressed breast milk ) may contribute to the increased NEC risk associated with formula feeding. Altogether, there is a substantial body of evidence suggesting that EGF could be useful therapeutically for promoting mucosal repair.
Despite the potential demonstrated in preclinical work, concerns over possible tumorigenic effects have limited exploration of EGF as a therapeutic agent (for discussion, see Ref. ). While EGF can drive wound repair and recovery of homeostasis, unregulated signaling through its receptor EGFR also plays a role in GI neoplasias. ErbB receptor tyrosine kinases have shown some promise as therapeutic targets in a variety of epithelial cancers including in colon. Altered EGF expression has been described in a number of tumors including pancreatic, esophageal, gastric, hepatic, and colorectal cancers. Furthermore, the potential for EGF to contribute to GI neoplasia has been suggested by mouse models, for example, the development of hepatocellular neoplasia in transgenic mice that overexpress secretable EGF. However, it should be noted that mutation, amplification, or forced overexpression represent radically different mechanisms than activation of the endogenous receptor with its normal ligand, even if the ligand is given therapeutically (acutely, instead of constitutive overexpression). Studies with mice deficient in EGFR signaling indicate that endogenous signaling actually acts as a tumor suppressor in some circumstances. As with many other regulatory peptides, EGF-driven signaling likely sits in a “Goldilocks” zone, with either excessive or insufficient activity leading to disease.
Loss-of-function studies suggest a functional redundancy for EGF exists in the intestinal tract. For example, administration of exogenous peptide is trophic for the GI tract and protects against intestinal injury, whereas EGF knockout mice have neither an overt intestinal phenotype nor exaggerated sensitivity to acute DSS colitis (though chronic colitis has not been well-described in this context). In contrast, the EGFR wav5 mutation, which encodes a receptor with very low activity, does predispose to and worsen colitis. This apparent contradiction is generally thought to be the result of ligand redundancy and/or compensation, though it is also clear from cell culture studies that individual ligands elicit distinct molecular and cellular responses. In fact, to achieve a histologically notable phenotype (in this case, spontaneous duodenal ulceration) in the absence of additional challenge (e.g., nonsteroidal antiinflammatory drug-mediated injury, cytokine injection), Troyer and colleagues deleted three different ligands —EGF, amphiregulin, and TGF-α. It is unclear whether the effects of this triple deletion are exactly equivalent to total loss of EGFR/ErbB1 signaling in the epithelium, as whole body knockout of the receptor is lethal in early life, though the GI tract is definitely perturbed in EGFR −/− pups. Furthermore, data from conditional knockout mice have not yet been reported. Overall, however, targeting ErbB receptors directly tends to have a greater physiological impact than deletion of limited sets of ligands.
Another complication with interpreting the results from ligand knockouts is recent data showing differential involvement for EGF signaling in different cell types; for example, while it is clear that EGFR activation in epithelial cells is protective, in macrophages it can promote inflammatory responses and contribute to colitis, as EGFR deletion from cells of the myeloid lineage (including macrophages) reduced disease in the murine DSS model. Similarly, in Helicobacter -induced gastritis, lack of macrophage-specific EGFR resulted in decreased gastric inflammation, though this was accompanied by increased bacterial load. These results demonstrate a role for EGF signaling in GI physiology and disease beyond its traditional role as a mitogenic factor. Further studies of the cell type-specific effects of EGF (and other ligands), and comparisons between the role of endogenous (and thus physiologically localized) versus exogenous, therapeutic application are warranted.
Next to EGF, the most extensively studied EGF-family ligand in the GI tract is TGF-α. This molecule was initially discovered in the 1980s in screens designed to uncover factors involved in transformation of normal cells to malignant cells. In particular, these efforts were meant to identify factors that could be produced by the cells themselves that have self-regulating autocrine activity. These screens using assays of growth in soft agar as a measure of tumorigenicity identified TGF-α and TGF-β as cooperative drivers of transformation. As noted above, despite their names TGF-α shares sequence homology with EGF rather than TGF-β, competes with EGF for binding sites, and shares many biological activities of EGF owing in part to its affinity and signaling through the same receptor, EGFR.
TGF-α is readily expressed in the GI tract in fetal and adult stages and found as early as 10 weeks into gestation in humans that persists throughout life. Animal studies also suggest that GI expression of TGF-α may decrease with age. Expression is detectable in most epithelial cells of the GI tract at low levels including stomach, esophagus, small, and large intestines. In the stomach, levels are highest in parietal cells. In the esophagus and intestine, it is predominantly found in differentiated epithelial cell populations. In a similar manner to EGF and other growth factors, TGF-α is proteolytically cleaved from its membrane-bound proprotein by ADAM metalloprotease sheddases into the active form.
At first glance, substantial redundancy between TGF-α and EGF might be expected, and indeed in a number of tissues, the mature TGF-α plays similar roles to EGF in terms of cellular proliferation and differentiation. However, these molecules display clear differences in regulation of expression, localization/compartmentalization, EGFR binding, and biochemical effects on the receptor. For instance, EGF is secreted from distinct sites of the GI tract, whereas TGF-α is more broadly expressed, thus segregating the effects of these two growth factors based on location. TGF-α tends to be available primarily basolaterally, whereas the major portion of EGF seems to be apical. Furthermore, TGF-α and EGF bind EGFR with different kinetics ; this contributes to different profiles of downstream effector binding as well as different endocytic trafficking of ligand- receptor complexes leading to either EGFR recycling or destruction.
In vivo studies have shown that active TGF-α has trophic effects on the GI epithelium and stimulates epithelial growth, enhanced restitution, and cellular proliferation. It is important to note that TGF-α is sorted largely to the basolateral compartment. As its receptor, EGFR is also basolaterally located, it has been suggested that in contrast to EGF juxtacrine or paracrine TGF-α activity may be important for homeostatic regulation of the GI tract. Highlighting this difference in compartmentalization, TGF-α administered enterally shows no significant effects on proliferation, demonstrating a lack of functional redundancy between EGF and TGF-α in this tissue. Alternatively, TGF-α administered parenterally results in stimulation of GI growth and cell proliferation. Furthermore, TGF-α overexpressing mice show hyperplastic gastric mucosa. Knockout mice for this ligand or animals transgenically overexpressing it display increased susceptibility to, or protection from, DSS colitis, respectively. Thus, TGF-α is clearly an essential part of the injury response in the intestine.
As with EGF, TGF-α also plays a role in hepatocyte growth and liver regeneration. In the partial hepatectomy model, TGF-α is induced in liver and circulation and correlates with increased DNA synthesis in the regenerating liver. Interestingly, TGF-α is not required for regeneration as mice deficient in this ligand are still able to exhibit hepatocyte proliferation. This suggests EGF or other EGFR-signaling molecules compensate and restore liver mass in these settings. It is interesting to note, however, that TGF-α overexpressing animals have increased liver mass and elevated DNA synthesis and hepatocyte proliferation, demonstrating the significant effect of TGF-α on liver growth.
TGF-α also has a variety of nonmitogenic roles in the GI tract. Like EGF, it limits gastric acid secretion, but is also rendered less active by gastric acid in the stomach demonstrating a regulatory loop in its activity. TGF-α has also been shown to modulate ion and nutrient transport, stimulate mucin secretion, and mesenteric and mucosal blood flow and promote smooth muscle contraction. Together, these roles appear to promote tissue maintenance and repair following GI injury.
Not surprisingly in light of how TGF-α was discovered, this ligand is deregulated in many GI cancers, including esophagus, stomach, and colon. Several lines of evidence suggest the overexpression of TGF-α is associated with severity of tumorigenicity. For instance, TGF-α expression positively correlates with tumor severity and is expressed in serum in the case of GI tumors, including gastric, pancreatic, and colon. Furthermore, activation of the TGF-α receptor, EGFR, is increased in GI cancer opening the field for therapeutic intervention using several FDA-approved EGFR inhibitors that could act in part by limiting the action of TGF-α (gefitinib, erlotinib, cetuximab, panitumumab, and lapitinib). Efforts to identify patients who would be most responsive to specific treatments or chemotherapeutic agents are still underway.
NRG growth factors (also known as heregulins, HRG) are a subclass of EGF-like molecules that were initially identified in the 1990s in screens for ErbB3 and ErbB4 ligands. Since this time, the study of NRGs has expanded dramatically, and roles for this family of growth factors have been identified in cardiac development, neuronal function, metabolism, epithelial cell development and survival, and immune cell activation. The NRGs harbor mitogenic roles including growth, differentiation, and survival of epithelial, glial, and muscle cells in vitro.
Mammals harbor four neuregulin genes (NRG1-4). NRG transcripts are readily detected in the liver, stomach, small intestine, and colon. Substantial splice variation as well as multiple transcriptional start sites per gene allow for production of a wide array of distinct molecules, including for example up to 15 different NRG1 peptides and 4 or more NRG4s. The functional significance of the different variants of each gene product have, for the most part, not yet been explored. The most widely studied ligand, NRG1β (a.k.a. HRG1β), is expressed throughout the GI tract including esophagus, stomach, intestine, and colon. Aside from a few recent papers on NRG4, most of what is known about neuregulins in the gut is based on work with NRG1β. It should also be noted that the majority of functional studies, especially in cell culture or administration to animals, have used soluble extracellular domain peptides (i.e., the “business end” of the molecule). Thus, many of these findings will be cross-applicable not only to a number of different isoforms but also leave out entirely the impact of regulatory effects on cleavage/secretion or potential juxtacrine signaling from tethered ligand.
The majority of NRGs are synthesized as preproteins inserted in the plasma membrane, thus requiring proteolytic cleavage by ADAM sheddases. Notable exceptions include the B-type variants of NRG4, which are missing the transmembrane domain and appear to be expressed in the cytoplasm, with as-yet unknown function. Since the 1990s, experimental evidence has uncovered the affinity of the shed ligands for each of their various ErbB receptors. NRG1 and NRG2 bind and activate both ErbB3 and ErbB4 (with some splice variant-driven specificity between α and β variants preferring ErbB3 and ErbB4, respectively), while NRG3 and NRG4 exclusively bind ErbB4, at least in cell culture experiments.
Functionally, NRGs and their receptors in the intestine have been shown to have roles in cytoprotection, regulation of chloride secretion, development of the enteric nervous system, and epithelial secretory cell differentiation. NRG4, in particular, has antiapoptotic effects on the intestinal epithelium ; on the other hand, it can elicit cellular death responses in other cell types such as inflammatory macrophages. The ability to kill inflammatory macrophages while protecting the intestinal epithelium from cytokine-induced apoptosis is the likely explanation for the protective effects of NRG4 in colitis models. Additionally, ErbB4 (the NRG4 receptor) has been associated with hypoxia signaling and can stabilize hypoxia-induced factor-1α, which tends to be protective in the gut. ErbB4 stabilization of hypoxia-induced factor-1α was associated with altered regulation of cellular metabolism, which together with studies showing NRG4 has a protective effect versus obesity-associated inflammation suggests a likely role for NRGs in the link between hypoxia and metabolism, which may be very important in the gut.
Dysregulation of NRG signaling has been linked to GI disease development. Whole-exome sequencing revealed that NRG1 is frequently mutated in IBD-associated colorectal cancer. Polymorphisms or deletions of this gene as well as of NRG3 are associated with Hirschsprung’s disease. NRG1 and 2 are both decreased in KRAS-mutant colon cancers. NRG1 and NRG4 expressions are suppressed in total parenteral nutrition-associated intestinal inflammation (where excessive intestinal epithelial apoptosis is observed), but can be rescued by EGF administration. NRG4 expression is decreased in human inflammatory bowel disease and rodent models of colitis. Interestingly, restoration of NRG4 ameliorates disease parameters in several animal models of colitis, suggesting harnessing neuregulin signaling may be a beneficial therapeutic target in the GI tract.
Heparin-binding epidermal growth factor-like (HB-EGF) growth factor was initially identified as a mitogenic factor present in the conditioned media of a tumor macrophage cell line. Its expression is induced by TNF and oxidative stress, among other proliferative stimuli. Like other EGF-related peptides, HB-EGF is synthesized as a transmembrane protein and proteolytically cleaved by ADAM sheddases to generate its mature, active soluble form. The dominant activities of HB-EGF are stimulating cell proliferation, survival, and cell motility. HB-EGF binds EGFR and ErbB4 to induce phosphorylation. Limited evidence exists supporting different functions of HB-EGF between these two receptors. For example, in cells expressing ErbB4 but not EGFR, the effect of this ligand is chemotactic as opposed to proliferative.
HB-EGF has been identified in gastric parietal cells, but its intrinsic expression elsewhere in the GI tract under homeostatic conditions is low. Exogenous sources of HB-EGF include recruited macrophages and breast milk. In the intestine, HB-EGF is rapidly induced in response to acute injury, where it has been shown to protect against hypoxic injury and may play a role in wound healing. In intestinal, kidney, and liver epithelial cells, enforced expression of or treatment with HB-EGF prevents cell death in response to apoptotic stimuli (such as TNF), demonstrating its role as an epithelial survival factor. These findings suggest growth factor signaling elicited by a recruited cell type or source (i.e., macrophages, breast milk) may be an important role in the protection of GI epithelium following damage. In this regard, HB-EGF has been studied fairly extensively for activity against NEC. Exogenous HB-EGF treatment is effective in preventing incidence and severity of formula feed/hypoxia-induced NEC in rat pups, as is overexpression in transgenic mice ; conversely, knockout animals were more susceptible to experimental NEC. Protection with HB-EGF is accompanied by improved barrier function, reduced epithelial apoptosis, and a reduction in damage to intestinal microcirculation. Interestingly, HB-EGF also altered the balance of macrophage polarization in the gut to a more repair-directed (so-called “M2” population) phenotype in this model, suggesting that similar to NRG4 and EGF, HB-EGF has important effects on the innate immune cells during inflammation, though each ligand seems to have a very different mechanism of action in these cells.
Amphiregulin (AR) was first described in 1988, and is named for its ability to stimulate or inhibit cell growth depending on the cell type under study. AR is expressed in the GI tract in normal and neoplastic cells and binds exclusively to EGFR. At baseline, it is expressed at low levels, primarily in the small intestinal epithelium and surface epithelium of the colon. Levels in both the epithelium and the mesenchyme increase in inflammatory bowel disease and colon cancers. Studies have shown AR stimulates epithelial cell growth and may promote tumorigenesis via an autocrine loop ; it may also be packaged in exosomes and stimulate tumor growth through this mechanism. In vivo studies of AR-null mice show no obvious baseline defects in the GI tract without additional challenge, supporting a normal physiological role primarily involving response to injury or inflammation rather than homeostatic turnover.
Similar to amphiregulin, epiregulin (EPR) can have either stimulatory or inhibitory effects on the growth of cells depending on context. This ligand, first described in 1995, is produced both by stromal fibroblasts and epithelial cells, and like AR is induced by challenge. EPR appears to be important for repair, as deletion results in increased susceptibility to DSS-induced colitis. However, EPR knockouts show no overt developmental defects, suggesting this ligand is also more important in response to injury than homeostasis. It is dispensable for intestinal tumorigenesis, but can contribute to tumor growth and to expansion of Lgr5 + stem cells during regeneration and carcinogenesis.
Betacellulin (BTC) was first identified in 1993 from a mouse insulinoma cell line and appears to be expressed in pancreas and throughout the epithelium of the small intestine and colon. It is also a component of expressed milk, at least in cows. Relative to EGF, it signals through distinct patterns of EGFR phosphorylation suggesting distinct signaling outcomes. In fact, a recent analysis clustering EGFR ligands based on recruitment (and timing) of downstream effectors grouped EGF, amphiregulin, and EPR together, with BTC, TGFα, and epigen forming a second cluster and HB-EGF standing unique. Furthermore, like HB-EGF BTC can bind ErbB4 as well as EGFR, adding additional complexity to its potential function. BTC stimulates crypt cell proliferation and increases intestinal size, dependent on EGFR signaling, in mice, and may have antiapoptotic effects on intestinal epithelial cells. Furthermore, in a transgenic overexpression system, BTC promoted tumor development (multiplicity) in Apc min mice. The explicit role for this ligand in normal physiology or whether it is required for intestinal tumorigenesis remains unclear.
The intestinal function for epigen, the most recently identified ligand in this group has not to date been reported. EPGN expression in the small bowel and colon is supported by online datasets in the Gene Expression Omnibus ( https://www.ncbi.nlm.nih.gov/geo/ ). Thus, it likely has as-yet-undescribed roles in intestinal physiology.
All or nearly all of the ligands that bind ErbB family receptor tyrosine kinases are represented in the GI tract. While there appears to be substantial overlap in the function of these ligands, detailed analyses have demonstrated both shared and distinct roles in GI physiology. In-depth studies focused on understanding the individual regulation, biochemistry, and function of these ligands have the potential to uncover new approaches to leveraging signaling driven by these ligands for clinical use in GI disorders.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here