Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The purpose of this chapter is to integrate the most common clinical scenarios faced in obstetric practice with pathologic examination of the placenta. Because much of the pathology has been covered descriptively in Chapter 31, Chapter 32 , the principal intent of this chapter is to discuss pathologic conditions as they present clinically, focusing on pathologic conditions that lead to premature birth, induction of labor, and peripartum and postpartum hemorrhage. Only previously uncovered pathologic aspects of clinical disorders are discussed in more detail. The penultimate section of this chapter briefly addresses pathologic aspects of twin gestations, and the final section of this chapter addresses four discrete clinicopathologic entities, termed constellation disorders (amniotic fluid infection, maternal vascular malperfusion, fetal vascular malperfusion, and chronic abruption) with suggested pathologic reporting of these conditions.
Premature birth , defined as birth between 20 and 37 completed weeks' gestation, is one of the most serious and costly problems in obstetric practice. Although preterm birth usually occurs in a minority (6% to 15%) of pregnancies, depending on geographic and demographic features, it accounts for 75% of perinatal mortality and more than 50% of long-term morbidity. Preterm labor, defined as regular uterine contractions accompanied by a change in cervical dilation, effacement, or both, precedes approximately 50% of preterm births. Premature births can be clinically divided into (1) spontaneous premature births, including those preceded by preterm labor, preterm premature rupture of membranes, and/or cervical incompetence, and (2) those resulting from labor induced by the obstetrician for significant fetal or maternal disorders. Spontaneous premature births account for approximately two-thirds of preterm deliveries. Preterm delivery can also be subdivided into several categories based on gestational age or cause. In general, pathologists should examine all preterm placentas. With spontaneous preterm labor, diagnostic findings that correspond to the clinical course are usually but not always present. Placental examination in induced preterm delivery is important for documenting placental findings that may have contributed to or resulted from the underlying clinical disorder that necessitated induction.
The pathogenesis of preterm birth is likely closely related to the pathogenesis of preterm labor; however, at present, neither is completely understood. Currently, the majority of spontaneous preterm births are thought to be accounted for by four distinct pathways: (1) maternal or fetal stress, (2) excessive myometrial and cervical stretching, (3) decidual hemorrhage (abruption), and (4) infection or exaggerated response to genital tract microbes. In turn, it has been suggested that preterm labor be considered an obstetrical syndrome with multiple potential etiologies (e.g., inflammation/infection, uteroplacental ischemia, uterine over-distension) and predisposing factors, including maternal hypertensive disorders, fetal growth restriction, and non-reassuring fetal testing. These predisposing factors are also among the most common indications for preterm induction of labor.
Other common indications for spontaneous or induced interruption of pregnancy before term include polyhydramnios, oligohydramnios, maternal abdominal surgery in the second and third trimesters, maternal medical disorders, cigarette smoking, cocaine use, prior cervical conization, and uterine anomalies. Intrauterine infection is frequently associated with preterm birth, with reported rates of 25% to 40%. The likelihood of chorioamnionitis is further influenced by the clinical setting: the risk is approximately 31% in idiopathic premature delivery, 42% following preterm premature rupture of membranes, and 81% in premature delivery related to cervical incompetence. The presence of chronic inflammatory cells in the basal plate (i.e., chronic deciduitis) has been associated with preterm birth and, therefore, may play a role in the initiation of partuition. Inflammatory decidual reaction seems to be an important initiator of parturition. Vaginal bleeding caused by placental abruption or placenta previa is another common factor symptom associated with a high risk of preterm delivery, occurring in 10% of cases. These considerations offer a segue into the following sections related to preterm birth.
Acute chorioamnionitis is the most common histologic diagnosis made in placentas sent for pathologic evaluation. Preterm births account for the majority of cases, with a decrease in prevalence with advancing gestational age. Almost all spontaneous preterm births at 21 to 24 weeks' gestation demonstrate histologic chorioamnionitis, whereas it is present in only 5% to 10% of cases at 35 to 36 weeks' gestation. Overall, acute chorioamnionitis has been reported in 21% to 24% of term placentas and as many as 67% of preterm placentas. Many associated complications exist, the frequencies of which are also gestational age dependent, including maternal or fetal sepsis, premature membrane rupture, preterm labor, and adverse long-term neurodevelopmental outcome.
Intrauterine infection can occur via four main routes, the first of which is by far the most common: (1) ascending from the cervix, vagina, and perineum (also called amniotic fluid infection syndrome ), (2) hematogenous maternal-to-fetal spread, (3) iatrogenic introduction via invasive techniques, and (4) retrograde spread through the fallopian tubes.
In each of these situations, in response to maternal innate immune system detection of microorganisms, inflammatory chemokines and cytokines (e.g., interleukin 8, interleukin 1β, tumor necrosis factor) are released. Microbial endotoxin and additional maternal inflammatory mediators, including matrix-degrading enzymes, contribute to progressive cervical dilation and eventual membrane rupture. Leukocytic prostaglandins stimulate uterine contractions, and labor is initiated.
Until only recently, it was believed that the fetus developed in an essentially sterile environment, and when intrauterine infection occurred, it was most often a consequence of ascending infection from the cervix, vagina, and/or perineum. Recent studies using comparative 16S ribosomal DNA-based and whole-genome shotgun metagenomics methods have demonstrated a unique low-biomass microbiome in human placentas. Furthermore, taxonomic analyses have revealed association of the placental microbiome with preterm birth. These studies at least call into question the long-standing belief that the majority of intrauterine infections are caused by ascending infection; however, the role of the placental microbiome in preterm birth, as well as other inflammatory conditions, requires future study because many questions remain to be addressed.
Microorganisms can be demonstrated with conventional culture technique in fewer than half of preterm births. However, recent molecular microbiologic techniques, such as polymerase chain reaction (PCR), have improved the detection rate, especially in the cases with negative amniotic fluid culture. Among numerous bacterial species that have been isolated, the most common organisms found in the amniotic cavity are genital Mycoplasma species, in particular Ureaplasma urealyticum , followed by Mycoplasma hominis, Streptococcus agalactiae, Escherichia coli, Fusobacterium species, and Gardnerella vaginalis . Candida albicans and other fungi also may occasionally cause acute amniotic fluid infection.
The clinical diagnosis of “acute chorioamnionitis” in women in preterm labor may be challenging owing to variable presentation and variable or inconsistent use of terminology and clinical diagnostic criteria. The results of a recent workshop focusing, in part, on the evaluation of women diagnosed with clinical chorioamnionitis, acknowledges that this term is clinically applied to a heterogeneous group of infectious and inflammatory conditions and also that this term conveys a definitive infectious etiology when one many not be present. Therefore, the term “intrauterine inflammation, infection, or both” is recommended. Furthermore, in the situation of maternal fever (>39° C or 102.2° F on one occasion or >38° C or 100.4° F on two occasions at least 30 minutes apart) absent other symptoms, the term isolated maternal fever is recommended. The diagnosis of intrauterine inflammation, infection, or both is recommended when maternal fever is present, as well as one or more of the following: fetal tachycardia (>160 beats/minute for >10 minutes), elevated maternal white blood cell (WBC) count (>15,000), purulent fluid from the cervical os, or biochemical or microbiologic amniotic fluid results consistent with microbial invasion of the amniotic cavity.
The clinical outcome of acute chorioamnionitis, including maternal and fetal inflammatory response, has been previously discussed in Chapters 31 and 32 .
Features of ascending amniotic infection that can be appreciated on gross examination have been discussed previously in Chapter 31, Chapter 32 (see “ Ascending Infection in Amniotic Fluid Infection ”). From the clinical perspective, it is important to remember that gross pathologic features are variable and correlation with microscopic pathology is imperfect, but that histologic identification of maternal with or without fetal inflammation trumps gross features of inflammation.
Microscopic features of acute chorioamnionitis have been discussed previously in Chapter 32 (see “Ascending Infection” ) and in multiple sections by location of inflammation (e.g., umbilical cord, membrane roll) in Chapter 31 . Schema for staging and grading maternal and fetal inflammatory responses are presented in Table 32.1 .
As also discussed in Chapter 32 , placental cultures and special stains have a limited role in identifying causative organisms. Using conventional culture techniques, microorganisms can be demonstrated in fewer than half of preterm births. Gram and silver stains (e.g., Gomori methenamine silver [GMS], methenamine silver stain [MSS]) can be used to confirm the presence of microorganisms but are usually insufficient to determine species. The specificity of viral immunohistochemical stains (e.g., CMV, HSV I/II) often allow identification of the causative organism. Recently, PCR-based techniques using bacterial 16S or fungal 18S ribosomal RNA have improved the detection rate, especially in the cases with negative amniotic fluid culture. Among numerous bacterial species that have been isolated, the most common organisms found in the amniotic cavity are genital Mycoplasma species, in particular U. urealyticum , followed by M. hominis, S. agalactiae, E. coli, Fusobacterium species, and G. vaginalis . Candida albicans and other fungi also may occasionally cause acute amniotic fluid infection.
The main histologic differential diagnosis when considering acute chorioamnionitis is chronic chorioamnionitis, a process that may, at least in some cases, represent maternal anti-fetal rejection. In chronic chorioamnionitis the inflammatory infiltrate also involves the chorionic plate but is instead composed of maternal CD8 + T cells. The extent of the infiltrate is often less severe and less diffuse than the infiltrate seen in acute chorioamnionitis. It is also important to remember that maternal and/or fetal neutrophilic inflammation is not de facto equivalent to infection; correlation with additional clinical and pathologic findings is needed.
Q: If there is no clinical query of chorioamnionitis but I see subchorionic neutrophils, should I make the diagnosis?
A: Maternal inflammation limited to the subchorionic zone is best termed acute subchorionitis (early/evolving chorioamnionitis).
Cervical incompetence is a clinical diagnostic term that is synonymous with cervical insufficiency and is classically defined as recurrent second-trimester pregnancy loss following painless cervical dilatation, attributed to the inability of the cervix to retain the gestation. Cervical incompetence can result from prior traumatic injury to the cervix associated with a prior delivery or previous surgery (e.g., conization, amputation), congenital uterine anomalies, such as those resulting from diethylstilbestrol (DES) exposure, or intrinsic deficiencies in cervical collagen and elastin. The incidence of cervical insufficiency is estimated to be 1% of all pregnancies and as many as 20% of midsecond trimester spontaneous pregnancy losses. In general, cervical incompetence is classified on a continuum, in that gradations of cervical length may influence risk. Recent studies have examined cervical length as a screening tool utilizing transvaginal ultrasound, demonstrating progressive increase in risk as a function of reduced cervical length, with a cut-off point assigned according to gestational age, being demonstrated. The ideal gestational age for screening transvaginal ultrasound is 16 to 24 weeks, with reported cervical length ranges from 1.5 to 5 cm. Cervical length less than 2.5 cm falls below the 10th percentile for 16 to 24 weeks, and at 21 to 25 weeks, 1.5 cm is the second percentile. This screening test is not considered useful after 28 weeks' gestation, when physiologic cervical shortening occurs.
The cervix plays a critical role in protecting the intrauterine environment. Before parturition, the cervix is firm, composed predominantly of collagen. Any condition that degrades collagen enhances cervical softening and pliability, which sets the stage for dilatation. As previously mentioned, this process involves several mediators, including prostaglandins and cytokines; thus, it is not surprising that inflammation is frequently seen in the setting of preterm labor. The cervical canal normally contains mucus with antibacterial properties. With cervical dilatation, these antibacterial properties are impaired, increasing the risk of ascending infection, which subsequently stimulates progressive cervical dilatation. As a result, the cervix becomes incompetent to retain intrauterine contents, and preterm delivery ensues.
The typical clinical presentation of preterm delivery associated with cervical incompetence is painless cervical dilatation with protruding or ruptured membranes and abrupt delivery. Efforts at prevention have focused on the cervical cerclage. However, only a proportion of women with prior early gestational losses experience repeat miscarriage, irrespective of management; thus, the value of cerclage placement in a given case has been controversial. Furthermore, cerclage does not entirely prevent preterm birth in all women with short cervical length assessed by transvaginal ultrasonography. There is no proven benefit of prophylactic cerclage in women at low or medium risk of second-trimester loss, regardless of cervical length by ultrasound.
The possibility of cervical incompetence can only be evaluated indirectly on placental examination. Often, cervical incompetence is associated with significant acute chorioamnionitis, therefore, the placenta, umbilical cord, and/or membranes may show gross features of acute chorioamnionitis (previously discussed). The placentas associated with cervical incompetence may also show marginal, retroplacental, or subchorionic hemorrhage. We have termed this constellation of findings inflammatory abruption, a pattern that raises concern for cervical incompetence (discussed later), or at the very least for an increased risk of recurrent preterm delivery.
Without intervention, cervical incompetence often results in preterm delivery. In women without signs of intrauterine infection or painful uterine contractions, emergency cerclage placement prior to 26 weeks' gestation has been shown to prolong pregnancy compared to conservative management. History of prior preterm birth is a risk factor for subsequent preterm birth; however, only a proportion of women with prior early gestation in the setting of cervical incompetence experience repeat miscarriage, regardless of management strategy. As such, the value of cerclage placement in a given case has been controversial. Furthermore, cerclage does not entirely prevent preterm birth in all women with short cervical length. There is no proven benefit of prophylactic cerclage in women at low or medium risk of second-trimester loss, regardless of cervical length by ultrasound.
As with the gross examination, cervical incompetence cannot be determined based on microscopic examination. However, associated features such as acute chorioamnionitis, acute deciduitis, and “inflammatory abruption” may be seen.
After placental examination, and in the context of clinical correlation (e.g., spontaneous pre-viable delivery), the pathologist can raise concern for cervical incompetence/recurrent preterm delivery based on the constellation of findings; however, the diagnosis is ultimately a clinical one. It remains important for the pathologist to exclude mimics of acute chorioamnionitis (such as, chronic chorioamnionitis) and non-inflammatory abruption.
Q: What is the most accurate way to word a comment raising concern of clinical cervical incompetence, based on pathologic findings in a placenta with chorioamnionitis and “inflammatory abruption” in the pre-viable period?
A: After enumerating the findings in the diagnosis, a comment can be added that: “The constellation of findings noted above and occurring in the pre-viable period raises concern for an increased risk of recurrent preterm delivery. Clinical correlation is recommended.”
Histologic abruption is more prevalent with advanced stage maternal inflammation (stages 2 and 3) in second-trimester compared with third-trimester deliveries. The term inflammatory abruption applies to cases of inflammation-induced maternal bleeding and is more prevalent with advanced stage maternal inflammation (stages 2 and 3) in second-trimester compared with third-trimester deliveries. Inflammatory abruption must be distinguished, at least conceptually, from classic placental abruption (see Chapter 32 ) resulting from maternal vascular disorders that typically occur later in gestation, and from chronic abruption (see later).
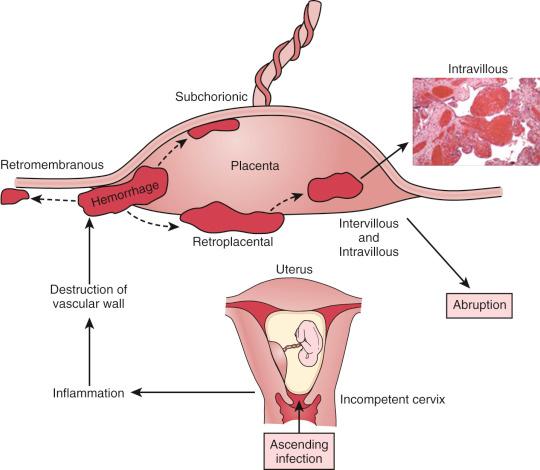
The pathogenesis of inflammatory abruption begins with cervical dilatation, which allows infectious organisms to ascend through the endocervical canal, infecting first the decidua adjacent to the internal os, leading to acute deciduitis and chorioamnionitis. Decidual inflammation is believed to then contribute to aberrant coagulation. In this model, a plausible pathogenesis is that proinflammatory cytokine release from acute deciduitis destroys extracellular matrix and maternal vessel walls, causing perivascular leakage of plasma proteins and coagulation factors, loss of vessel integrity, and ultimately leading to hemorrhage ( Fig. 33.1 ). Bleeding usually originates in the marginal area of the placenta ( Fig. 33.2A ), undermining the placental edge and extending into the subchorionic and retroplacental zones (see Fig. 33.2B ). Because the placenta is relatively fragile in mid-gestation, dissecting intervillous hemorrhage is also commonly seen (see Fig. 33.2C ).
The clinical presentation of inflammatory abruption is variable depending on the extent of infection and hemorrhage. Gestational bleeding is not a reliable indicator of abruption.
Placental abruption of any type is associated with adverse perinatal outcomes including stillbirth, preterm delivery, and intrauterine fetal growth restriction; however, outcome studies tend not to distinguish among types of abruption, and conclusions and magnitude of risk are likely biased toward outcomes typical of classic placental abruption.
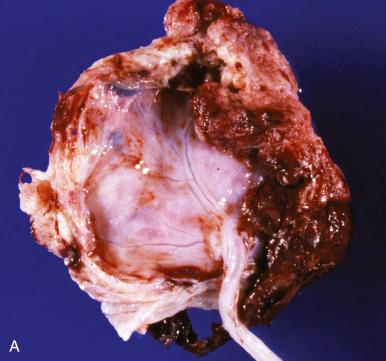
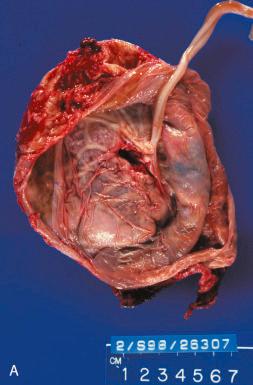
The placenta may show similar features as seen in acute chorioamnionitis, such as discolored membranes, as well as evidence of bleeding. Bleeding usually originates in the marginal area of the placenta (see Fig. 33.2A ), undermining the placental edge and extending into the subchorionic and retroplacental zones (see Fig. 33.2B ). If not disrupted during delivery or en route to pathology, adherent blood clot may be found on the maternal surface.
In inflammatory abruption, evidence of acute deciduitis, acute subchorionitis, and/or acute chorioamnionitis will be seen. Additionally, subchorionic and/or intervillous hemorrhage are often present; the placenta is relatively fragile in mid-gestation, therefore maternal blood more readily dissects into the disc parenchyma (see Fig. 33.2C ).
Based on the finding of blood clot adherent to the maternal surface of the placenta on gross examination, the differential diagnosis may include classic placental abruption and chronic abruption; however, these can usually be excluded microscopically based on the absence of associated acute inflammation in the chorionic plate, decidua, membranes, and/or umbilical cord and by correlation with the clinical history.
Q: If the patient is hypertensive and has a pre-viable delivery with abruption, how can I be sure the abruption isn't a consequence of underlying hypertension?
A: Hypertension-induced abruption in mid-gestation is rare; if present, one would expect to see additional features of maternal malperfusion, such as fetal and/or placental growth restriction, decidual arteriopathy, patterns of villous ischemia, and so on. One would also not expect to see chorioamnionitis. Correlation with the clinical history (features of infection, clinical severity of hypertension) should also be informative.
The term chronic abruption applies to cases of maternal venous hemorrhage leading to marginal premature placental separation. Chronic abruption is associated with several conditions including oligohydramnios, in which case the clinical constellation is termed chronic abruption-oligohydramnios sequence . Chronic placental bleeding typically occurs days or weeks before delivery and is reflected in the placenta by a constellation of features termed diffuse chorioamnionic hemosiderosis (DCH) (see later).
Placental abruption is defined as premature detachment of the placenta. Classical placental abruption is associated with maternal vascular disorders caused by arterial bleeding, whereas venous hemorrhage leads to marginal and chronic abruption. The classic clinical presentation with abdominal pain, heavy vaginal bleeding, and fetal distress is seen with large acute arterial abruption (see Chapters 31 and 32 for discussion of abruptio placentae). By contrast, venous abruption often presents with low-level, persistent, or recurrent vaginal bleeding, often in the absence of other signs of maternal or fetal disease. Maternal history associated with DCH includes subchorionic hematoma diagnosed by ultrasound in the first trimester, recurrent vaginal bleeding, and brown discolored amniotic fluid.
DCH is associated with many adverse neonatal outcomes, such as preterm delivery, intrauterine growth restriction (IUGR), persistent pulmonary hypertension of the newborn, “dry lung syndrome,” and neurologic impairment.
Chronic/persistent vaginal bleeding induces placental changes that manifest as (1) circumvallation (a consequence of blood dissecting beneath the membrane attachment to the placental disc); (2) degenerating retromembranous, subchorionic, or marginal blood; and (3) muddy brown or green-brown discolored membranes and chorionic plate, which may appear similar to long-standing meconium staining ( Fig. 33.3A ).
Microscopic examination reveals scattered to abundant hemosiderin deposition that appears as refractile dark brown pigment on hematoxylin and eosin (H&E) stained slides. The hemosiderin is usually phagocytosed by macrophages within the extraplacental membranes and chorionic plate (see Fig. 33.3B ). Other pathologic features of chronic maternal circulatory compromise (e.g., accelerated villous maturation, villous agglutination, increased intervillous fibrin, proliferation of intermediate trophoblast) may also be seen in placentas with chronic abruption. This malperfusion constellation likely reflects diminished placental efficiency due to circumvallation, because there is no association between DCH and maternal hypertensive-type disorders.
Confirmation of the pigment as hemosiderin can be demonstrated by Prussian blue iron stain (see Fig. 33.3C ), which stains hemosiderin blue. Of note, blood breakdown pigments, such as bilirubin, will appear yellow on H&E stained slides and will not be highlighted by Prussian blue stain.
Based on the finding of blood clot adherent to the maternal surface of the placenta on gross examination, the differential diagnosis may include classic placental abruption and inflammatory abruption. These can usually be excluded microscopically based on the absence of hemosiderin deposition in extraplacental membranes and/or the chorionic plate, the absence of circumvallation, and the absence of established chorioamnionitis.
Q: How many features of DCH are required to make the categorical diagnosis?
A: We recommend identification of degenerated maternal blood with associated hemosiderin-laden macrophages in the membranes and chorionic plate, and involving at least half of the area sampled. There should also be a third piece of corroboratory evidence (such as circumvallation) and/or associated clinical features (such as non-acute vaginal bleeding, oligohydramnios, preterm delivery, or fetal growth restriction).
Induction of labor can be categorized as elective or indicated. Elective induction is becoming more popular, primarily for convenience of the practitioner or patient. Currently, routine elective induction at term is not justified because induced labor is associated with an increased cesarean delivery rate. By contrast, indicated labor induction is performed when the benefits to either the mother or the fetus outweigh those of continuing the pregnancy, even after factoring in risks attributable to induction. Indications may vary from rather stable clinical conditions (e.g., membrane rupture without labor, suspected fetal macrosomia) to emergency conditions (e.g., non-reassuring fetal status). Women whose labor is induced have an increased incidence of chorioamnionitis and cesarean delivery compared with those who labor spontaneously. Whether elective or indicated, induction procedures, augmentation with oxytocin, and operative obstetrics procedures (e.g., cesarean sections) are associated with increased risk of both fetal and maternal morbidities. This section discusses the more common fetal and maternal indications for induction of pregnancy, as well as some of the serious associated complications that can arise from induction procedures.
Toxemia or hypertensive disorders of pregnancy are commonly occurring conditions that may lead to significant maternal and fetal morbidity and mortality. Based on classification by the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy, there are four hypertensive disorders that occurin pregnancy: (1) preeclampsia/eclampsia, (2) chronic hypertension, (3) chronic hypertension with superimposed preeclampsia, and (4) gestational hypertension.
Preeclampsia/eclampsia: Defined as either (1) hypertension with proteinuria (≥300 mg/24 hours or 1+ dipstick) or (2) hypertension without proteinuria but with any one of the following: thrombocytopenia, impaired renal function, elevated liver function, pulmonary edema, or cerebral or visual symptoms. Preeclampsia can be subdivided into mild and severe preeclampsia. Severe preeclampsia is considered when any of the following conditions are present: diastolic blood pressure of 110 mm Hg or more, epigastric pain, oliguria, elevated serum creatinine, thrombocytopenia, elevated liver enzymes, pulmonary edema, or new onset cerebral or visual disturbances. Eclampsia refers to the onset of seizures in patients with severe preeclampsia.
Chronic hypertension: Defined by hypertension that (1) antedates pregnancy, (2) is diagnosed before 20 weeks' gestation and is not attributable to gestational trophoblastic disease, or (3) is first diagnosed after 20 weeks' gestation and persists after 12 weeks postpartum.
Superimposed preeclampsia on chronic hypertension: Diagnosed when there is (1) new onset proteinuria (≥300 mg/24 hours) in the setting of chronic hypertension or (2) acute elevation in proteinuria, blood pressure, or thrombocytopenia on top of chronic hypertension and proteinuria.
Gestational hypertension (formerly known as “transient hypertension”): Diagnosed by an elevated blood pressure of 140/90 mm Hg or greater for the first time during pregnancy, without proteinuria, and with normalization of blood pressure by 12 weeks after delivery.
Among these four categories, preeclampsia is the most prevalent condition, and this term is often used interchangeably with the term toxemia. Preeclampsia/eclampsia usually starts after the 32nd week of pregnancy but begins earlier in patients with hydatidiform mole or preexisting kidney disease or hypertension. The onset is usually insidious, characterized by hypertension and edema, followed by proteinuria. Headaches and visual disturbances are common. Eclampsia is heralded by central nervous system involvement, including convulsions and potential coma. Mild preeclampsia can be controlled by bed rest, a balanced diet, and antihypertensive agents, but induction of delivery labor and delivery is the only definitive treatment of established preeclampsia and eclampsia. Recently, low-dose aspirin, if started before 16 weeks' gestation, has been shown to prevent more than half of the cases of preeclampsia among high-risk women and reduce the risk of IUGR and perinatal death.
Preeclampsia is a multiorgan disease process of incompletely defined pathogenesis, although abnormal placentation leading to placental ischemia appears to be a critical and necessary component. Potential inciting causes or contributing factors can be classified into four groups: (1) abnormal trophoblast invasion of uterine vessels, (2) immunologic intolerance between maternal and fetoplacental tissues, (3) maternal maladaptation to cardiovascular or inflammatory changes of normal pregnancy, and (4) genetic predisposition ( Box 33.1 ). Most proposed pathogenetic pathways suggest poor placental perfusion causes release of various factors that lead to maternal signs and symptoms. This may involve abnormalities in related events: trophoblast invasion and the development of physiologic alterations in placental vessels required to perfuse the placental bed adequately. With endovascular invasion, cytotrophoblasts invade and remodel the uterine spiral arterioles. Under normal conditions, invading cytotrophoblasts undergo phenotype changes, with loss of E-cadherin expression and acquisition of expressed endothelial receptors: VE-cadherin, platelet-endothelial adhesion molecule-1, vascular endothelial adhesion molecule-1, α4, and αvβ3 integrins. In preeclampsia, invading cytotrophoblasts are unable to assume the surface receptor phenotype of vascular endothelial cells. These defects in cytotrophoblast differentiation are associated with shallow implantation, leading to incomplete conversion of low-capacitance, high-resistance uterine vessels into high-capacitance, low-resistance vessels needed to maintain a normal pregnancy state. The net effect is reduced blood flow and placental ischemia. It is further thought that this decreased utero-placental perfusion induces expression of placental vasoconstrictor molecules (thromboxane, angiotensin, endothelin) concomitant with inhibition of vasodilators (prostaglandin I2, prostaglandin E2, nitric oxide).
Abnormal placental implantation, with defects in the following:
Cytotrophoblastic differentiation
Endovascular invasion
Spiral arteriole remodeling
Angiogenic factors
Increased sFlt-1 (sVEGFR-1)
Decreased PlGF and VEGF
Reduced placental blood flow/placental ischemia
Immunologic intolerance between fetoplacental and maternal tissue
Altered coagulation/platelet function
Increased thrombosis and DIC
Platelet activation
Cardiovascular maladaptation and vasoconstriction; increased maternal vascular resistance
Increased circulating vasoconstrictor substances
Altered renin/angiotensin mechanism
Vascular endothelial damage or dysfunction
Genetic predisposition: Maternal or paternal thrombophilias
DIC, Disseminated intravascular coagulation; PlGF, placental growth factor; sFlt-1, soluble fms-like tyrosine kinase 1; sVEGFR-1, soluble vascular endothelial growth factor receptor-1; VEGF, vascular endothelial growth factor.
Immunologic and inflammatory processes have gained attention as important contributory mechanisms of preeclampsia. The “immunization concept” involves impaired formation of maternal blocking antibodies to placental antigenic sites, which is supported by the increased rate of preeclampsia in multifetal gestation, and the additive number of antigenic sites on multiple placentas compared with the total amount of maternal blocking antibody. Another line of evidence supporting the significant role of immunologic factors is an increased risk of preeclampsia in multiparous women who are impregnated by a new consort. Several studies have demonstrated a significant lower proportion of helper T cells in preeclamptic women compared with normotensive pregnancies. Inadequate helper T lymphocytes may be involved in the evolution of preeclampsia through their role in secreting specific cytokines that promote placental implantation.
Inflammatory changes are usually considered a response to tissue ischemia. Activated leukocytes release a number of cytokines and interleukins, which lead to oxidative stress and free radical formation, interfere with prostaglandin status and nitric oxide formation, and add to endothelial injury.
Circulating soluble vascular endothelial growth factor receptor-1 (sVEGFR-1), which binds both placental growth factors (PlGFs) and vascular endothelial growth factors (VEGFs), has received much attention in recent years. Normally, near term, serum levels of sVEGFR-1 increase and PlGF and VEGF decrease, reflecting a reduction in angiogenic activity. In preeclampsia, this shift is initiated much earlier than normal, with pathologic consequences. Preeclamptic placentas overproduce sVEGFR-1, which, when administered to pregnant rats, produce the characteristic systemic and renal abnormalities seen in preeclamptic patients. This premature application of antiangiogenic “brakes,” including sVEGFR-1, appears to play a pivotal role in the evolution of disease.
The mechanism of preeclampsia appears to also involve the renin-angiotensin system and prostaglandins. Normal pregnant women develop a resistance to the vasoconstrictive and hypertensive effects of angiotensin, but women with preeclampsia lose such resistance, developing a propensity for hypertension. Prostaglandins of the E series, produced in the utero-placental vascular bed during pregnancy, are thought to mediate the normal resistance of pregnant women to angiotensin. Prostaglandin production is decreased in the placenta of preeclamptic women. Thus, the increase in angiotensin hypersensitivity, characteristic of preeclampsia, may be due to decreased prostaglandin synthesis by the preeclamptic placenta. There is also evidence that placental renin production is increased in preeclampsia, providing an additional vasoconstrictive molecule. Finally, placental ischemia leads to a higher output of thromboplastic substances; concomitantly, antithrombin III levels are reduced.
Other disorders that share clinical and pathologic features with preeclampsia include the autoimmune family of disorders (lupus erythematosus, lupus-anticoagulant disorder/antiphospholipid syndrome) and connective tissue disorders, such as scleroderma; hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome; and some cases of “idiopathic” fetal growth restriction presumed to share a similar pathogenesis as known disorders, but for which the pathologic substrate is not identified.
Preeclampsia complicates approximately 5% of pregnancies, usually in the last trimester and more commonly in primiparous than multiparous women. Other associated risk factors include maternal age over 35 years old, chronic hypertension, multifetal gestation, and obesity. With mild preeclampsia, affected patients may manifest only modest hypertension, proteinuria, and edema. However, the degree of proteinuria may fluctuate widely over a 24-hour period, even with severe disease; thus, a single random sample may fail to demonstrate what truly significant proteinuria is. With more severe disease, patients may develop signs and symptoms of reduced organ perfusion secondary to vasospasm and endothelial activation; these include thrombocytopenia, visual disturbance, epigastric pain, and oliguria. Thrombocytopenia may be due to microangiopathic hemolysis induced by severe vasospasm, or to platelet activation and aggregation. Epigastric or right upper quadrant pain may be manifestations of hepatocellular ischemia, necrosis, or edema that stretches Glisson's capsule. It is often accompanied by elevated hepatic enzyme levels. Proteinuria and hypertension usually disappear within 1 to 2 weeks after delivery, except in patients whose findings antedated pregnancy.
The placental pathology of hypertensive maternal disorders is discussed in Chapters 31 and 32 , the latter within the “Maternal Vascular Malperfusion” section.
Q: I have a small placenta with several prominent features of maternal malperfusion, yet there is no history of a maternal hypertensive disorder. What should I recommend?
A: The patient should be serologically tested for autoimmunity, if there is not an already established autoimmune disorder.
The placental pathology of abruption placentae is discussed in Chapters 31 and 32 , the latter within the “Acute Catastrophic Demise” section. Caveat: The causes of induced delivery in the setting of maternal bleeding will naturally overlap with those of spontaneous antepartum hemorrhage.
The two main differential considerations of antepartum hemorrhage are (1) abruptio placentae and (2) placenta previa. An abruptio placentae, or premature placental separation, is manifested by significant vaginal bleeding in the late second to third trimesters. However, abruption can also be clinically silent, and patients may present without vaginal bleeding (although abdominal pain and rigidity may still be present). So-called concealed abruption may occur in as many as 20% of cases clinically classified as abruption following fetal and placental delivery. Bleeding because of placental abruption is not typicallylife threatening to the mother but may threaten thefetus, resulting in stillbirth about 35% of the time. Fetal distress, which may eventuate in chronic morbidity or mortality, is due to hypoxia secondary to maternal and sometimes fetal hemorrhage; susceptibility for untoward outcome appears enhanced in the setting of concealed abruption. Other clinical manifestations of abruption include premature labor, labor with hypertonic uterine contractions, “port wine” amniotic fluid noted at cesarean section, and large clots passed with the placenta followingvaginal delivery. There are multiple predisposing factors associated with placental abruption, and patients may present with clinical features of preeclampsia, gestational or chronic hypertension, or uterine over-distention (multiple pregnancy or polyhydramnios) or history of cocaine abuse or maternal abdominal trauma (e.g., unexpected falls, motor vehicle accidents). Multiple predisposing factors associated with placental abruption include maternal hypertension, preeclampsia, uterine over-distention (multiple pregnancy or polyhydramnios), cocaine abuse, and maternal abdominal trauma (e.g., unexpected falls, motor vehicle accidents).
Although uncommon, placental abruption remains a significant cause of maternal and morbidity andperinatal mortality. Maternal complications are primarily related to blood loss, including long-term risk ofcardiac disease, whereas fetal complications are related to hypoxia due to placental malperfusion. The natureof risk or complication to the mother depends on the severity of the bleeding and to the fetus on theseverity of the bleeding compounded by gestational age. Bleeding because of placental abruption is not typically lifethreatening to the mother but is associated with the need for blood transfusion, emergency hysterectomy, disseminated intravascular coagulopathy, and renal failure. Fetal complications include stillbirth; and in live births low birth weight, preterm delivery, and features of neonatal asphyxia.
In the setting of antepartum hemorrhage, the main clinical differential diagnosis is placenta previa. This differential diagnosis can typically be resolved by imaging studies. If gross examination is performed, features that support the diagnosis of placenta previa include point of membrane rupture that reaches the edge of placental disc and marginal and velamentous umbilical cord insertions; however, these features are not specific. Furthermore, cases of both placenta previa and placenta abruption may exhibit maternal surface disruption, and both placenta previa and chronic abruption may exhibit marginal retroplacental blood clots.
Based on gross examination finding of adherent blood clot, the pathologic differential diagnosis includes inflammatory abruption and chronic abruption. The gross and microscopic features distinguishing these entities have been previously discussed.
Q: What if there is a clinical diagnosis of abruption but the pathologic features (retroplacental bleeding with overlying placental infarction) are not fully present?
A: In this case, a comment can be made: “Diagnostic features of placental abruption are not present. However, abruption occurring shortly before delivery may not manifest diagnostic pathologic changes.”
Diabetes mellitus (DM) is a common medical complication of pregnancy and can be separated into two groups: (1) pre-gestational or overt DM, in which diabetes is established prior to pregnancy; and (2) gestational DM, in which diabetes is first diagnosed during pregnancy. Based on the White classification system, diabetes in pregnancy can be subclassified into classes A to H. Class A is gestational DM, whereas classes B to H are overt DM, subdivided by end-organ damage, such as retinopathy, nephropathy, or cardiovascular system involvement. Gestational diabetes mellitus (GDM) is generally subcategorized into class A1 and A2. In GDMA1, patients exhibit an abnormal oral glucose tolerance test (OGTT) and normal fasting blood glucose levels, and their disease is typically managed with diet and exercise. In GDMA2, patients exhibit abnormal OGTT and fasting blood glucose levels, and their disease typically requires insulin to achieve normoglycemia, depending on the presence of fasting hyperglycemia levels. (A1 is diagnosed when the OGTT is abnormal with normal fasting blood glucose levels; typically, this type is diet controlled. A2 is diagnosed when both the OGTT and the fasting blood glucose level are abnormal; typically, this type needs additional drug therapy [insulin, glyburide].) GDMA2 is diagnosed when the fasting plasma glucose is 105 mg/dL or greater. Clinically, this classification is quite important, because different clinical outcomes may result. Diagnoses for each of these entities (e.g., chorangiosis) have been discussed previously.
DM can have direct effects on both the mother and the fetus. Pregnant women with DM have increased risks of preterm labor, hypertensive disorders of pregnancy, birth trauma, and cesarean section. Untoward fetal outcomes include spontaneous abortion, congenital anomalies, macrosomia, shoulder dystocia, birth injury, and stillbirth, in addition to a panoply of neonatal complications, such as hypoglycemia, hypocalcemia, hyperbilirubinemia, and polycythemia. The risk of complications is variable. For example, fetal anomalies are increased threefold to fourfold in women with overt DM or GDMA2, whereas women with GDMA1 have malformation rates similar to the general nondiabetic pregnant population. Additionally, intrauterine fetal demise is increased in women with overt DM, but not GDMA1. Reported associated fetal anomalies are multifold and include caudal regression, situs inversus, neural tube defects, cardiac anomalies, anal atresia, and renal anomalies. Diabetes, however, is not associated with an increased risk for fetal aneuploidy.
Macrosomia is one of the major fetal consequences of GDM and may lead to several adverse events, such as shoulder dystocia, birth trauma to the fetus or mother, and an increased cesarean delivery rate. Macrosomia, caused by fetal hyperinsulinemia, results from a fetal response to maternal hyperglycemia. Fetal pancreatic beta cells secrete insulin, stimulating somatic and visceral overgrowth, and excess adiposity. Fetal hyperinsulinemia may also result in neonatal hypoglycemia shortly after birth.
In the setting of maternal diabetes with fetal macrosomia, gross examination of the placenta typically reveals a large placenta (more than 90th percentile for gestational age), commensurate with fetal size.
Common though nonspecific microscopic findings include relative villous immaturity for gestational age and chorangiosis (see Fig. 31.58 ). These features are also seen in placentas from macrosomic infants born to women without clinically defined gestational diabetes.
The differential diagnosis varies based on which nonspecific microscopic findings are observed.
Q: I have a large placenta with chorangiosis but without a maternal history of diabetes. Should I comment?
A: Occasionally, mothers will deliver macrosomic infants with large placentas showing chorangiosis, yet will not have clinically met the threshold criteria for diabetes. In those circumstances, a comment such as the following can be made: “Placental features fit the phenotype that can be seen in maternal diabetes. Clinical correlation with maternal glucose metabolism during pregnancy may be informative.”
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here