Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The stomach is a complex organ with unique mechanical, sensory, endocrine, and immunological properties. Alterations in gastric motility and sensation have been implicated in several gastrointestinal disorders, including gastroparesis, functional dyspepsia, rumination syndrome, and dumping syndrome. 1 Understanding the evaluation and management of these disorders requires a thorough knowledge of the physiology of gastric motility and sensation.
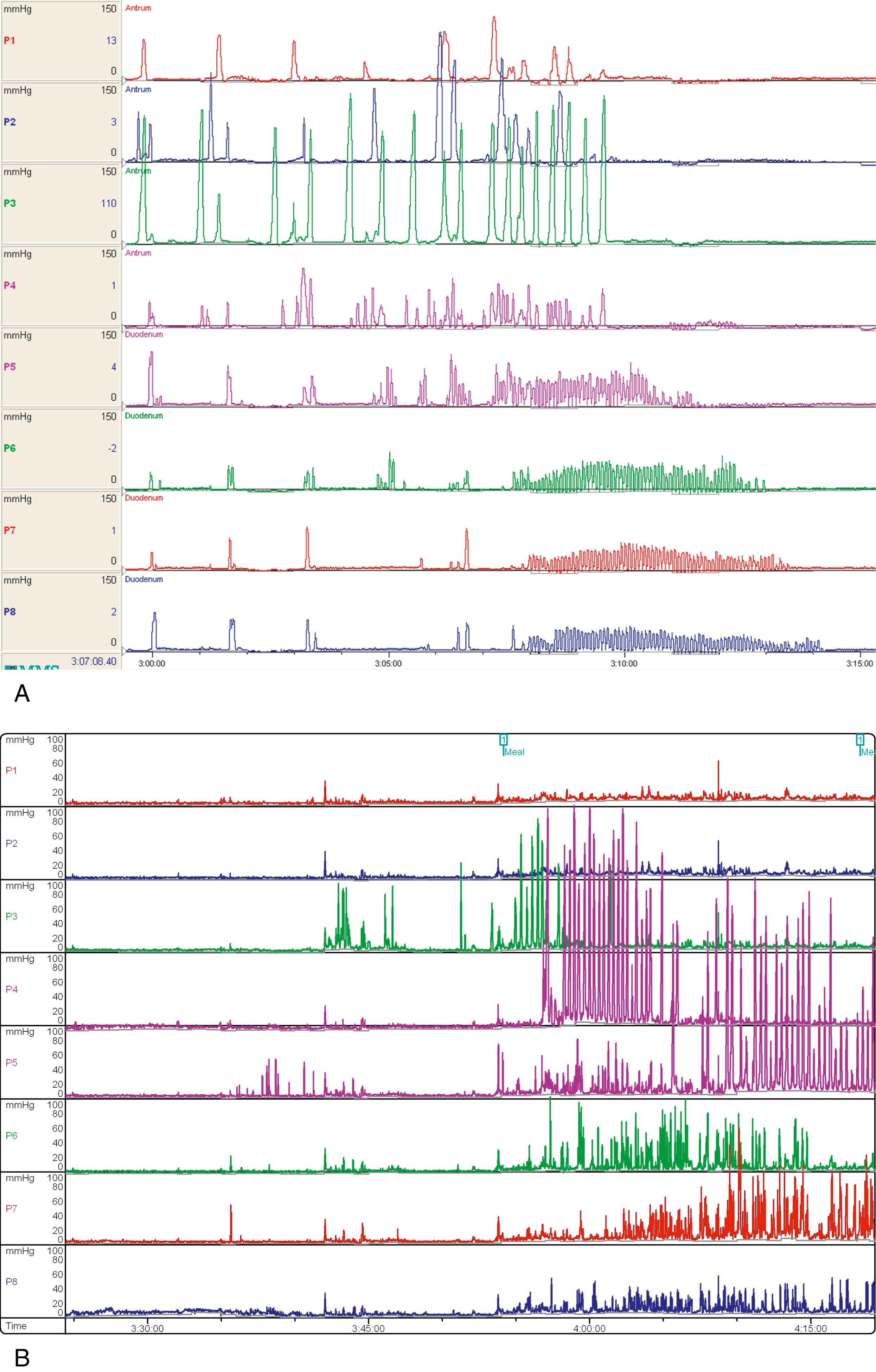
Normal gastric motor function can be divided into activity during the fasting period and activity in response to a meal. During the fasting period, gastric motor function is characterized by a cyclical pattern of motor activity involving both the stomach and the intestine called the migrating motor complex (MMC). This pattern generally starts about 2 to 4 hours after ingestion of a meal and consists of three phases that repeat approximately every 40 minutes in infants and up to every 90 to 120 minutes in adults. , Phase I consists of a period of motor quiescence. Phase II consists of a period of intermittent pressure activity, with sporadic contractions of varying amplitude. Phase III consists of an activity front with increased pressure activity, including rhythmic, high-amplitude contractions, that begins in the antrum or proximal small intestine and propagates distally toward the ileum. Contraction frequencies during phase III reach 3 per minute in the stomach and 10 to 12 per minute in the proximal small intestine. The phase III activity front is depicted in Fig. 28.1 . The MMC is thought to act as a “gastrointestinal housekeeper,” sweeping luminal contents toward the colon. In children with gastrointestinal motility disorders, a morphologically normal MMC is considered an important hallmark of health and is associated with tolerance of enteral feeding, decreased need for parenteral nutrition, and improved response to prokinetic medications. , ,
After ingestion of a meal, MMC activity is suppressed. Gastric tone decreases in the proximal stomach to accommodate ingested food without a significant increase in intragastric pressure. The proximal stomach consists of the gastric fundus and the proximal one-third of the gastric body. Gastric accommodation involves both receptive and adaptive relaxation. Receptive relaxation is triggered by oropharyngeal and gastric stimulation upon swallowing and leads to relaxation of the lower esophageal sphincter and proximal stomach. Adaptive relaxation occurs in a vagally mediated response to activation of mechanoreceptors in the gastric wall and osmo-/chemoreceptors in the stomach and duodenum. Activation of these receptors leads to nitric oxide release and an increase in nonadrenergic, noncholinergic inhibitory input and subsequent relaxation. Sympathetic inputs also contribute to changes in gastric tone. ,
Gastric emptying involves synthesis of a number of inputs and coordination among the fundus, antrum, pylorus, and duodenum. Local sensory nerves, vagal afferent nerves, and hormones provide input based in large part on gastric contents. As shown in Table 28.1 , a number of factors can influence gastric emptying. Gastric emptying will adapt to maintain a steady delivery of 2.5 kcal/min into the proximal duodenum. Coordination is orchestrated by gastrointestinal electrical activity through the interstitial cells of Cajal and neural input through the enteric nervous system and vagal efferent nerves from the central nervous system. Liquids generally empty from the stomach first, primarily as a result of the pressure gradient that develops between increasing gastric pressure and the duodenum. Solid food particles are first ground into smaller particles by rhythmic contractions propagating from the gastric pacemaker region of the gastric body distally through the antrum against a narrowed pylorus. These contractions classically occur at a frequency of three cycles per minute. The pylorus generally remains closed after a meal, allowing only particles 2 mm or smaller to pass into the duodenum. Larger particles are directed retrograde until they have been processed into small enough particles. ,
| Slow Emptying | Accelerated Emptying | |
|---|---|---|
| Gastric contents | Solids | Hot temperature |
| Lipids | ||
| ↑ Osmolar load | ||
| ↑ Caloric density | ||
| ↑ Gastric pH | ||
| Hormones | Glucagon-like peptide-1 (GLP-1) | Motilin |
| Leptin | Ghrelin | |
| Cholecystokinin | ||
| Peptide YY | ||
| Melatonin | ||
| Medications | μ-receptor agonists | Motilin agonists |
| α2-adrenergic agonists | Ghrelin agonists | |
| Anticholinergics | 5-HT 4 agonists | |
| Proton pump inhibitors | Dopamine agonists | |
| H 2 -receptor antagonists | Acetylcholinesterase inhibitors | |
| Miscellaneous | Hyperglycemia | Hypoglycemia |
| Colorectal distention | ||
| Stress | ||
| Exercise |
The gastrointestinal tract is able to interpret a number of luminal inputs, traditionally categorized into mechanosensitive and nutrient sensing pathways. The stomach primarily relies on mechanoreceptors to sense volume of ingested food. Gastric mechanoreceptors activated by the arrival of food then stimulate gastric accommodation and gastric acid secretion through intrinsic and vagovagal reflex pathways. These signals also play an important role in satiation, and several studies have demonstrated that gastric distention induces a satiating effect. However, the stomach also has some chemosensing ability, as the presence of amino acids in the gastric lumen enhances gastrin release from G cells and stimulates gastric acid secretion.
In the child with symptoms suggestive of gastric dysfunction, characterization of gastric motor function and sensation can further our understanding of the child’s symptoms and guide treatment. The clinical presentations of children with these disorders are often similar and the underlying diagnosis can be challenging to determine without further evaluation.
Gastric emptying scintigraphy (GES) is considered the standard method for measurement of gastric emptying, providing physiologic, noninvasive, quantitative measurement of gastric emptying. GES involves ingestion of a radiolabeled meal followed by serial measurement of radioactivity in the stomach, which directly correlates with the volume of meal remaining in the stomach. An example is shown in Fig. 28.2 . Variation in the test protocols used to perform GES is a significant limitation of this technique, and attempts to standardize the methodology of GES in adults have been made. GES is performed after a period of fasting. Medications that can affect gastric emptying, including prokinetic medications and opiates, should be discontinued prior to the test. The duration of discontinuation should be based on the medication’s half-life, but for most medications 48 to 72 hours should suffice. Serotonin receptor antagonists like ondansetron should have little effect on gastric emptying and can be given prior to GES. For children with diabetes, it is important to recognize that hyperglycemia delays gastric emptying.
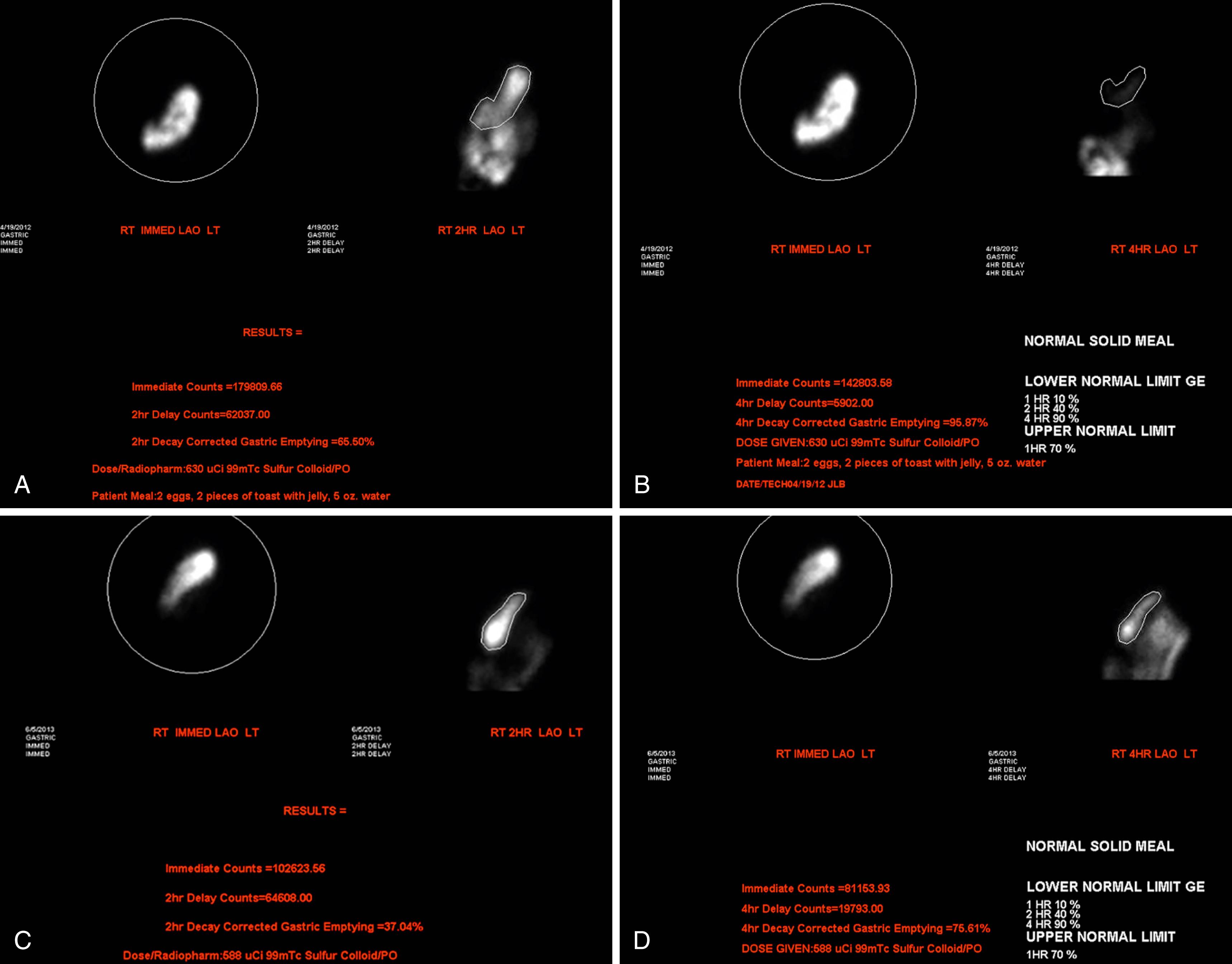
The recommended protocol for GES in adults involves measurement of percent gastric emptying at several time intervals after ingestion of a standard meal. The standard meal consists of the equivalent of two large eggs labeled with Tc-99m sulfur colloid along with two slices of white bread, jam, and 120 mL of water. Imaging is usually performed at 0 hour, 1 hour, 2 hours, and 4 hours. Delayed gastric emptying is defined as having greater than 90% retention at 1 hour, greater than 60% at 2 hours, and greater than 10% at 4 hours. Less than 30% retention at 1 hour is suggestive of rapid gastric emptying. This protocol has also been applied to children and adolescents, and although extending the duration of GES to 4 hours requires increased resource utilization, nearly a quarter of children who were found to have normal emptying at 2 hours had delayed emptying at 4 hours.
However, applying GES in children has its own inherent limitations. Younger and smaller children can have difficulty ingesting the standard meal in a timely manner. In one study, they were also more likely to have slower gastric emptying compared to older and larger children, suggesting that stomach size or other factors may contribute to GES measurements. The standard meal may not be appropriate for all children based on dietary restrictions and cultural preferences, and investigators have proposed meals that are vegetarian and palatable for children of various backgrounds. Interestingly, in a study of adults with upper gastrointestinal symptoms who underwent GES twice in a short time period, 30% had differing results. GES also requires expensive equipment and trained staff, and it involves a limited amount of radiation exposure.
Gastric emptying breath testing (GEBT) has been used as an alternate method of measuring gastric emptying that can be performed in the office setting and does not involve radiation exposure. 13C is a naturally occurring, nonradioactive isotope and can be administered as 13C-octanoic acid (octanoic acid is a medium-chain fatty acid) or 13C-spirulina ( Spirulina platensis is an edible blue-green algae) for the purposes of GEBT. Studies of GEBT using 13C-octanoic acid or 13C-spirulina in children have typically used a meal consisting of radiolabeled eggs, cake, or pancake. , After ingestion, 13C is absorbed in the small intestine, metabolized by the liver, and eliminated in exhaled air as 13CO 2 . The rate-limiting step in this process is gastric emptying, and thus measurements of 13CO 2 in breath samples can be used to calculate gastric emptying. , Because GEBT using 13C is an indirect measurement of gastric emptying dependent on several factors, results may not be accurate in children with malabsorption, hepatic dysfunction, and pulmonary disease. GEBT is not yet widely available for use in children in most clinical settings.
Wireless motility capsule (WMC) testing involves ingestion of a nondigestible capsule that measures pH, pressure, and temperature as the capsule travels aborally through the gastrointestinal tract. Gastric emptying can be measured based on the time from ingestion until a sharp rise in pH signifying the exit of the capsule from the acidic environment of the stomach to the alkaline duodenum. In adults, the gastric emptying time shown by the WMC correlates with the percentage of meal retained at 4 hours during GES, suggesting that the gastric emptying time represents the time near the end of emptying of a solid meal. In a study of children with upper gastrointestinal symptoms, prolonged gastric emptying time shown by the WMC was very sensitive (100% sensitivity) but only marginally specific (50% specificity) in identifying gastroparesis as determined by GES. WMC testing is also not yet widely available in pediatric settings.
Several other testing modalities have been used to evaluate gastric emptying, with limited clinical application. Serial MRI images have been used to measure emptying, whether by labeling a meal with gadolinium or by calculating gastric volume. Although MRI is noninvasive and does not require radiation exposure, it is also time-consuming and expensive. , , Abdominal ultrasonography has also been used to estimate gastric emptying after ingestion of a liquid or solid test meal based on either two-dimensional measurements (i.e., antral diameter) or three-dimensional computer-assisted reconstruction. Emptying is estimated based on measurements of gastric size and volume. Use of ultrasonography to estimate gastric emptying is time-consuming and not yet standardized.
Gastric barostat testing involves measurement of gastric compliance and distensibility through gradual inflation of an intragastric balloon by a computer-controlled pump. Measurement of volume changes in response to applied pressure allows assessment for gastric relaxation and accommodation. Concurrent recording of clinical symptoms is used to measure gastric sensation as well. Gastric barostat testing is the best validated measure of gastric accommodation and sensation, but it is invasive and challenging to perform in children. Gastric barostat testing has been mostly used in children for research studies.
Abdominal ultrasonography can be used for two-dimensional measurements of diameter or cross-sectional area of various parts of the stomach or for three-dimensional measurement through computer-assisted reconstruction of the stomach. While its utility may be limited in the evaluation of gastric emptying, abdominal ultrasonography is perhaps better suited for evaluation of gastric accommodation through serial measurement of gastric area or volume after ingestion of a liquid test meal. ,
The satiety drinking test (also called the nutrient drink test) has been used to indirectly assess gastric accommodation and involves measurement of the volume of a nutrient drink ingested until maximum satiety after an overnight fast. Patients are asked to drink the nutrient drink at a constant rate while rating their satiety every few minutes. In adults, the amount of calories ingested at maximum satiety correlates with gastric accommodation measured by gastric barostat. Normal values have been determined for children and adolescents. Investigators have recently proposed using a manometry catheter to measure intragastric pressure during ingestion of a nutrient drink.
Electrogastrography (EGG) involves noninvasive recording of gastric myoelectrical waveforms using electrodes placed on the surface of the upper abdomen. EGG measures gastric slow wave frequency and amplitude. Sinusoidal waveform frequency is normally 3 cycles per minute with an increase in amplitude after meals. Increased frequency suggests tachygastria and decreased frequency suggests bradygastria. EGG has traditionally been limited by the presence of artifacts during recordings and poor sensitivity and specificity. , EGG abnormalities are found in a fraction of patients with functional dyspepsia. The clinical utility of EGG testing remains controversial.
Antroduodenal manometry (ADM) measures antral and duodenal contractile activity by sequential pressure sensors along an intraluminal catheter. ADM requires placement of a water-perfused or solid-state catheter either nasally or via gastrostomy, with advancement until recording sites span the distal stomach and the proximal duodenum. Catheter placement is generally performed with fluoroscopic guidance or endoscopic assistance. Contractile activity and clinical symptoms are then recorded for several hours during the fasting, prandial, and postprandial phases. Prokinetic medications can be administered to characterize response. ADM is the only clinically available test that allows direct evaluation of gastric contraction patterns. However, the test is invasive and time-consuming, and its clinical use in children is generally limited to gastrointestinal motility centers.
Gastroparesis is defined as a delay in gastric emptying in the absence of mechanical obstruction accompanied by corresponding symptoms, including nausea, vomiting, early satiety, and abdominal pain. , In adults, the prevalence of gastroparesis has been estimated at 1.8%. Although the exact prevalence in children remains unclear, there is evidence that the number of hospitalizations for children with gastroparesis (and the associated cost of care) has been rising dramatically over the past decade.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here