Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
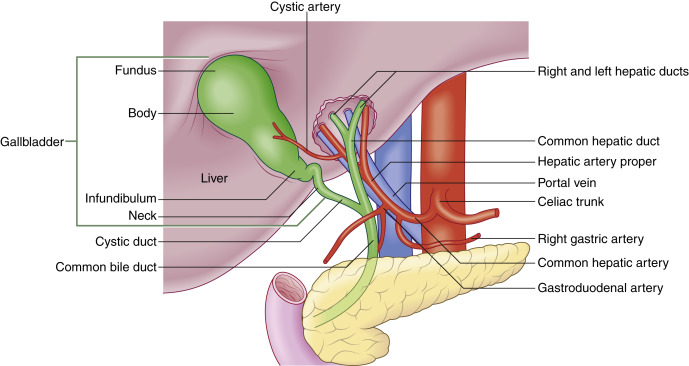
The normal anatomy of the gallbladder, biliary tract, and surrounding organs is presented in Fig. 17.1 . The gallbladder is connected via the cystic duct to the common hepatic duct, forming the common bile duct (CBD) that drains into the duodenum through the head of the pancreas. In most situations, the hepatic artery lies between the CBD and the more posteriorly located portal vein.
Imaging of the gallbladder is performed using a low-frequency transducer, such as a curved array (typically 3–6 MHz frequency). It is best to visualize the gallbladder and CBD in a parasagittal, as well as transverse plane, in real time. Patients are often imaged in a supine position; however, turning the patient in a lateral decubitus or right anterior oblique position may improve visualization. Occasionally, placement of the probe in other positions, such as intercostal or through the right flank, may be helpful for gallbladder visualization. Careful and deliberate interrogation of the entire gallbladder is imperative, as stones may be impacted in the gallbladder neck or pass through the cystic duct into the CBD and cause biliary ductal obstruction. The examiner may find a sonographic Murphy’s sign to be useful. A simple test is performed by placing the probe over the gallbladder to elicit pain. We find that placing the probe in different positions may be best to localize the true site of the pain. Thus probe pressure to the right of the gallbladder, over the gallbladder, and then over the mid-epigastric region may be used to best identify the true site of pain. A sonographic Murphy’s sign is defined as the presence of maximum tenderness elicited by direct probe pressure over the sonographically located gallbladder. If analgesics have been administered, a Murphy’s sign may be more difficult to elicit. On ultrasound we are evaluating the gallbladder primarily for stones, signs of inflammation of the gallbladder, and/or biliary obstruction. If the extrahepatic biliary ductal system appears dilated, then scanning through the liver as well as the head of the pancreas to evaluate the extrahepatic biliary system is important. It is important to document potential etiologies of biliary ductal obstruction such as choledocholithiasis and/or distal mass within the pancreas. When there is biliary ductal obstruction but no identifiable etiology on ultrasound, a computed tomography (CT) scan of the abdomen should be performed. Magnetic resonance imaging (MRI) may be useful to better identify etiologies of biliary obstruction such as choledocholithiasis.
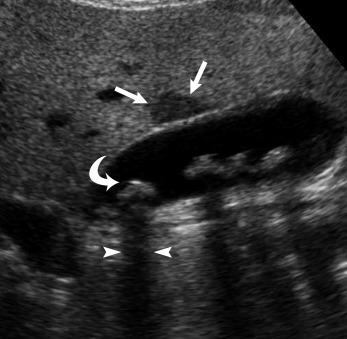
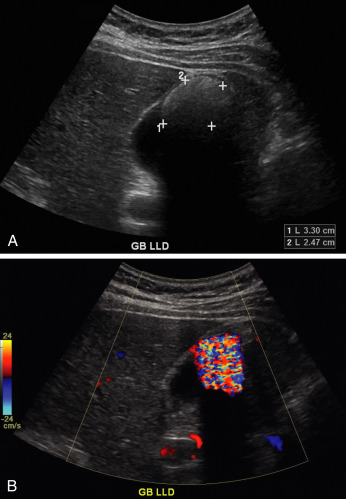
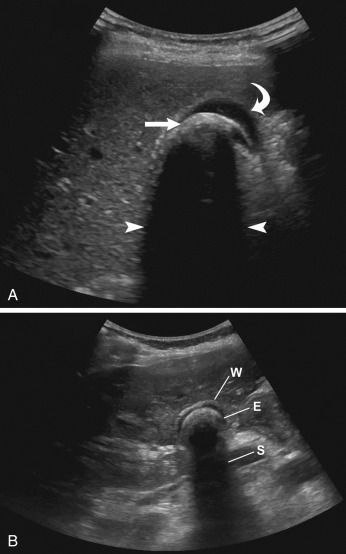
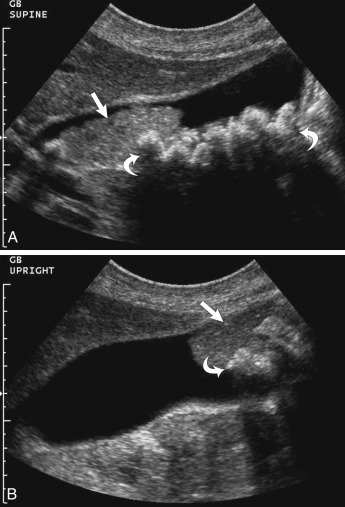
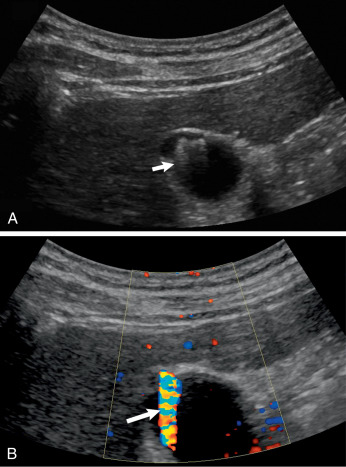
The principal imaging features that distinguish gallstones are mobility, echogenic focus, and acoustic shadowing ( Fig. 17.2 , ![]()
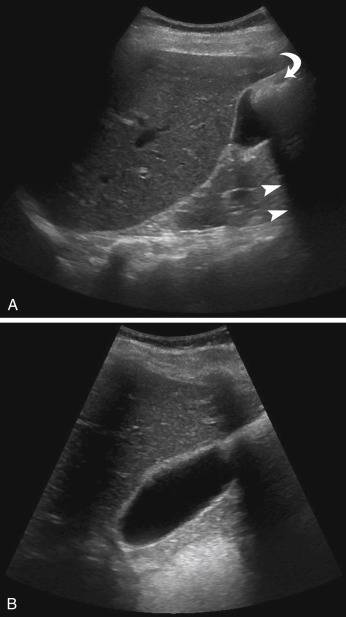
![]() ). Multiple studies have shown sensitivities of ultrasound of approximately 95%, with even higher positive and negative predictive values. Gallstones may also demonstrate a “twinkle” artifact on color Doppler imaging ( Fig. 17.3 ). When an echogenic focus is identified in the gallbladder, first shadowing should be confirmed. This is followed by repositioning the patient to demonstrate stone mobility. This can include having the patient upright or standing. Stones lodged in the cystic duct may not move. Careful attention to surrounding structures is important, so as not to confuse an echogenic bowel (which can create a “dirty shadow”) with gallstones ( Fig. 17.4 ). This artifact can be differentiated from stones by scanning the patient in different positions and noting that the bowel is not within the gallbladder fossa, as well as noting peristalsis within the bowel (
). Multiple studies have shown sensitivities of ultrasound of approximately 95%, with even higher positive and negative predictive values. Gallstones may also demonstrate a “twinkle” artifact on color Doppler imaging ( Fig. 17.3 ). When an echogenic focus is identified in the gallbladder, first shadowing should be confirmed. This is followed by repositioning the patient to demonstrate stone mobility. This can include having the patient upright or standing. Stones lodged in the cystic duct may not move. Careful attention to surrounding structures is important, so as not to confuse an echogenic bowel (which can create a “dirty shadow”) with gallstones ( Fig. 17.4 ). This artifact can be differentiated from stones by scanning the patient in different positions and noting that the bowel is not within the gallbladder fossa, as well as noting peristalsis within the bowel ( ![]() ). Scanning in different planes or obliquely may be necessary to separate adjacent bowel from the gallbladder (see Fig. 17.4 ). A Refraction artifact, which is a mildly echogenic area in the region of the neck of the gallbladder that produces acoustic shadowing, can also be confused for gallstones. This edge artifact is due to refraction or from the multiple small valves of Heister within the cystic duct. Other nonmobile echogenicities within the gallbladder, which may be confused with cholelithiasis, are listed in Table 17.1 .
). Scanning in different planes or obliquely may be necessary to separate adjacent bowel from the gallbladder (see Fig. 17.4 ). A Refraction artifact, which is a mildly echogenic area in the region of the neck of the gallbladder that produces acoustic shadowing, can also be confused for gallstones. This edge artifact is due to refraction or from the multiple small valves of Heister within the cystic duct. Other nonmobile echogenicities within the gallbladder, which may be confused with cholelithiasis, are listed in Table 17.1 .
|
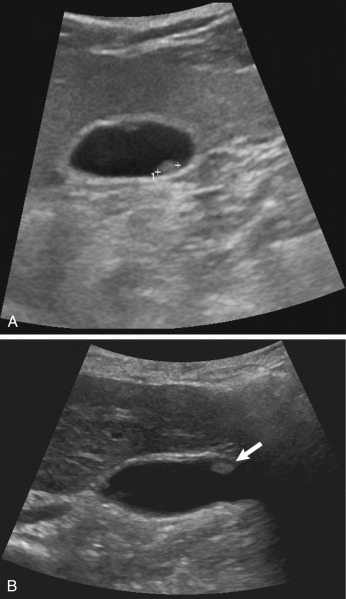
The gallbladder is best examined when the patient is fasting. In emergent situations, the patient may not always be adequately prepped. Thus when the patient is not fasting, the gallbladder may be contracted. Even in these situations, gallstones may be identified. Also, the gallbladder may be in a permanent state of contraction in cases of chronic cholecystitis. In these situations the wall, echo, and shadow, or “WES,” triad is observed. This corresponds to a visualization of the anterior gallbladder wall, with echogenicity representing the echogenic gallstones and posterior acoustic shadowing ( Fig. 17.5 , ![]() ). Again, this WES triad is fairly specific for chronic cholecystitis and cholelithiasis, but in patients with gallstones who are not fasting, their gallbladder may have a similar appearance. “Twinkle” artifact can also be seen in this entity (see
). Again, this WES triad is fairly specific for chronic cholecystitis and cholelithiasis, but in patients with gallstones who are not fasting, their gallbladder may have a similar appearance. “Twinkle” artifact can also be seen in this entity (see ![]() ). Patients with porcelain gallbladders will have an echogenic gallbladder wall with some shadowing. A porcelain gallbladder may predispose a patient to gallbladder cancer.
). Patients with porcelain gallbladders will have an echogenic gallbladder wall with some shadowing. A porcelain gallbladder may predispose a patient to gallbladder cancer.
Tumefactive sludge is often an incidental finding when there is examination of the gallbladder in a patient with right upper quadrant pain. Tumefactive biliary sludge may mimic gallstones or a mass. However, sludge will not shadow. Often this sludge may be mobile ( Fig. 17.6 ). Thus with repositioning of the patient, sludge may move. Additionally, adding color or power Doppler to the evaluation should demonstrate lack of vascularity in the sludge. There can be an exception to the rule of no acoustic shadowing with sludge. If gallstones are surrounded by sludge, they may produce the “twinkle” artifact or shadowing. Other causes of gallbladder masses and mimics of cholelithiasis are listed in Table 17.2 .
| Cause | Finding |
|---|---|
| Multiple stones | Echogenic layer with acoustic shadowing. |
| Sludge/sludgeball | Usually dependent, no color. Often mobile. |
| Stones and sludge | Stones surrounded by sludge (as above). |
| Blood | Dependent in gallbladder /or fills entire gallbladder. No shadowing. |
| Pus | Similar to blood, but with finding of acute cholecystitis. |
| Pseudo-sludge | A curvilinear echogenicity whose borders may project beyond the gallbladder and may disappear with different transducer orientations. |
| Parasites | Only in endemic areas or in patients from these areas. |
| Gallbladder polyps | Small masses with or without color flow. |
| Gallbladder cancer | Gallbladder mass with color flow and wall thickening, and often gallstones. |
Both benign and malignant gallbladder masses may be encountered when examining the gallbladder in the acute setting. This includes gallbladder polyps, cancer, or, rarely, metastasis ( Fig. 17.7 , ![]() ). Most polyps are small and may resolve spontaneously. However, adenomatous polyps may be precancerous.
). Most polyps are small and may resolve spontaneously. However, adenomatous polyps may be precancerous.
Gallbladder cancer may be missed on routine ultrasound. This is probably due to the fact that gallstones are often present in patients with gallbladder cancer, and any mass within the gallbladder may be obscured by the gallstones. Gallbladder carcinoma can be echogenic, isoechoic, or hypoechoic, and usually does have color Doppler flow. Gallbladder cancer may cause either diffuse or focal thickening of the gallbladder wall ( Fig. 17.8 ). Primary gallbladder cancer may invade the adjacent liver. Various cancers, including melanoma and gastrointestinal (GI) cancers, may metastasize to the gallbladder and appear as a vascular gallbladder mass.

Adenomyomatosis is characterized by epithelial proliferation and mucosal diverticula called Rokitansky–Aschoff sinuses. The most common form creates localized and confined wall thickening at the fundus of the gallbladder. This thickening can be so great, it appears as a mass and may be hard to distinguish from gallbladder cancer. There are other rare forms of segmental or diffuse adenomyomatosis. The pathognomonic finding of adenomyomatosis is the presence of hyperechoic foci, most commonly noted in the anterior wall of the gallbladder, which produces a comet tail artifact that decreases in width and amplitude more posteriorly ( Fig. 17.9 , ![]()
![]() ). This is thought to be secondary to cholesterol crystals within the Rokitansky–Aschoff sinuses in the gallbladder wall. Color Doppler will show a “twinkle artifact” in this entity (see Fig. 17.9 ), which is similar to the “twinkle” artifact seen with gallstones.
). This is thought to be secondary to cholesterol crystals within the Rokitansky–Aschoff sinuses in the gallbladder wall. Color Doppler will show a “twinkle artifact” in this entity (see Fig. 17.9 ), which is similar to the “twinkle” artifact seen with gallstones.
The American College of Radiology has imaging criteria for patients with right upper quadrant pain who have fever, leukocytosis, and a clinical positive Murphy’s sign, and recommends ultrasound as the first-line test in these situations ( Table 17.3 ). Patients may present with acute or chronic pain in the right upper quadrant of the abdomen. The level and acuity of pain are secondary to the etiology of the pain. For instance, chronic pain may be secondary to chronic cholecystitis and cholelithiasis, whereas more acute pain may be secondary to acute cholecystitis, gallbladder perforation, or acute biliary obstruction. Abnormalities of the liver, biliary tract, pancreas, or kidney should be considered in the differential as listed in Table 17.4 . In some situations, the etiology of the pain may not be discovered or may be secondary to etiologies that may require other imaging, such as CT.
| Radiologic Procedure | Rating | Comments | Relative Radiation Level |
|---|---|---|---|
| Ultrasound abdomen | 9 | ||
| MRI abdomen without and with contrast | 6 | Based on ultrasound findings, this generally should follow an ultrasound of the right upper quadrant. | |
| Cholescintigraphy | 6 | ☢ ☢ | |
| CT abdomen with contrast | 6 | ☢ ☢ ☢ | |
| MRI abdomen without contrast | 4 | ||
| CT abdomen without contrast | 4 | ☢ ☢ ☢ | |
| CT abdomen without and with contrast | 3 | ☢ ☢ ☢ ☢ |
|
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here