Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter brings together an integrated clinical approach for the patient who presents with a functional or dissociative (psychogenic) neurological disorder that is with symptoms that are inconsistent or incongruent with recognized neurological disease. We focus on the most common symptoms presenting to neurologists: blackouts, weakness, sensory disturbance, and movement disorders. We discuss scientific advances in understanding the etiology and mechanisms of these symptoms and how these lead naturally to new approaches to treatment. However, our primary aim is to give practical clinical advice to the neurologist struggling with an often challenging clinical situation.
Terminology in this area is problematic and reflects many different ways of conceptualizing and approaching the problem. There is no perfect solution here. The term to use will depend not only on how the cause of these symptoms is seen but also may depend on how the individual neurologist wishes to communicate the diagnosis to the patient (discussed later).
Conversion disorder (functional neurological symptom disorder) is the term used in in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), the American Psychiatric Association’s classification system for mental disorders. The name still retains the Freudian idea that intolerable psychological conflict leads to the conversion of distress into physical symptoms, but the new criteria are simpler and require only (a) the presence of a motor or sensory symptom, (b) positive evidence of inconsistency or incongruity with disease (such as the Hoover sign), (c) the disorder to not be better explained by a neurological disease (although one may be present), and (d) distress or impairment. Psychological factors are no longer required to be judged as being “associated with the symptom onset” in recognition of the fact that in many patients no identifiable recent stressor is present. The conversion hypothesis is currently just one of many competing hypotheses trying to explain these symptoms and is often an unsatisfactory model in clinical practice ( ). (For the full DSM-5 diagnostic criteria for conversion disorder, see Box 113.1 .)
One or more symptoms of altered voluntary motor or sensory function.
Clinical findings provide evidence of incompatibility between the symptom and recognized neurological or medical conditions.
The symptom or deficit is not better explained by another medical or mental disorder.
The symptom or deficit causes clinically significant distress or impairment in social, occupational, or other important areas of functioning or warrants medical evaluation.
Specify if:
Acute episode: Symptoms present for <6 months.
Persistent: Symptoms occurring for 6 months or more.
Specify if:
With psychological stressor (specify stressor)
Without psychological stressor
Coding note: The ICD-9-CM code for conversion disorder is 300.11, which is assigned regardless of the symptom type. The ICD-10-CM code depends on the symptom type (see below).
Specify symptom type:
(F44.4) With weakness or paralysis
(F44.4) With abnormal movement (e.g., tremor, dystonic movement, myoclonus, gait disorder)
(F44.4) With swallowing symptoms
(F44.4) With speech symptom (e.g., dysphonia, slurred speech)
(F44.5) With attacks or seizures
(F44.6) With anesthesia or sensory loss
(F44.6) With special sensory symptom (e.g., visual, olfactory, or hearing disturbance)
(F44.7) With mixed symptoms
Dissociative seizure/motor disorder (conversion disorder) (International Classification of Diseases, 10th Revision [ICD-10] F44.4–9 and ICD-11 6B60) suggests dissociation as an important mechanism in symptom production. Dissociation encompasses a variety of symptoms in which there is a lack of integration or connection of normal conscious functions. The difficulty is that not all patients with functional symptoms describe dissociative symptoms (see General Advice in History Taking, later).
Somatization disorder (DSM-IV 300.81) was a term applied to a patient with a history of symptoms unexplained by disease, starting before the age of 30. The definition in DSM-IV required at least one neurological symptom, four pain symptoms, two gastrointestinal symptoms, and one sexual symptom. Somatization disorder has essentially been eliminated from DSM-5, although the concept of someone with a lifelong vulnerability to functional disorders remains clinically useful.
Somatic symptom disorder replaced somatization disorder in the DSM-5, with the major distinction that it was irrelevant whether the somatic symptom had a basis in pathophysiological disease. The emphasis instead being on “Excessive thoughts, feelings, and/or behaviors related to these somatic symptoms or associated health concerns.” However, early signs are that this phrase will quickly become synonymous with somatization, despite the intentions of the authors.
Illness anxiety disorder describes excessive and intrusive health anxiety about the possibility of serious disease, which the patient has trouble controlling. Typically, the patient seeks repeated medical reassurance, which only has a short-lived effect. Health anxiety (previously called hypochondriasis) is often present to varying degrees in patients with psychogenic/functional symptoms but may be completely absent.
Factitious disorder (DSM-5) describes symptoms that are consciously fabricated for the purpose of medical care or other nonfinancial gain, in distinction to functional disorders which are genuine..
Munchausen syndrome describes someone with factitious disorder who wanders between hospitals, typically changing their name and story. There is a strong association with severe personality disorder.
Malingering is not a psychiatric diagnosis but describes the deliberate fabrication of symptoms for material gain.
Our preferred terms for motor/sensory symptoms and blackouts unexplained by disease are functional and dissociative because (a) they describe a mechanism and not an etiology and (b) they sidestep an illogical debate about whether symptoms are in the mind or the brain ( ; ). The term functional is used in this chapter and is increasingly the term of choice for those in the field ( ).
Functional describes in the broadest possible sense a problem due to a change in function (of the nervous system) rather than structure. It can be criticized for being too broad a term.
Psychogenic , psychosomatic , and somatization all describe an exclusively psychological etiology.
Nonorganic , nonepileptic describes what the problem is not , rather than what it is.
No diagnosis refers to the fact that many neurologists, even when faced with clear evidence of a functional/psychogenic neurological problem, are in the habit of making no diagnosis at all and simply conclude that there is no evidence of neurological disease ( ).
Medically unexplained superficially appears to be a neutral term but is often interpreted by patients and doctors as not knowing what the diagnosis is, rather than not knowing why they have the problem. Furthermore, many neurological diseases have uncertain etiology.
Hysteria , an ancient term originating from the idea of the “wandering womb” causing physical symptoms, is generally viewed as pejorative.
A number of studies of neurological practice have found that approximately one-third of neurological outpatients present with symptoms the neurologist does not think relate to neurological disease. In half of these (approximately one-sixth) the neurologist makes a primary “functional” or “psychogenic” diagnosis. The rest have some neurological disease but symptoms out of proportion to that disease ( ). These figures mirror those in other medical specialties where functional symptoms comprise approximately a third to a half of patients seeing a cardiologist, gastroenterologist, rheumatologist, and other specialty practices. Table 113.1 lists functional symptoms and syndromes according to specialty. Patients with functional neurological symptoms have much higher rates of these other “non-neurological” functional symptoms ( ).
| Specialty | Symptoms |
|---|---|
| Gastroenterology | Irritable bowel syndrome |
| Respiratory | Chronic cough, brittle asthma (some) |
| Rheumatology | Fibromyalgia, chronic back pain (some) |
| Gynecology | Chronic pelvic pain, dysmenorrhea (some) |
| Allergy | Multiple chemical sensitivity syndrome |
| Cardiology | Atypical/noncardiac chest pain, palpitations (some) |
| Infectious diseases | (Postviral) chronic fatigue syndrome, chronic Lyme disease (where physician disagrees that there is ongoing infection) |
| Ear, nose, and throat | Globus sensation, functional dysphonia |
| Neurology | Dissociative (nonepileptic) attacks, functional weakness and sensory symptoms |
| Psychiatry | Depression, anxiety |
Studies of patients with functional neurological symptoms have shown that they report just as much physical disability and have higher rates of anxiety and depression than patients with neurological disease. Most studies show that a minority of patients do not have psychiatric comorbidity. Patients with these symptoms are more likely than the general population to be out of work because of ill health ( ). Findings are similar in other specialties.
Clinical assessment of the patient with a functional disorder requires a somewhat different approach to the standard neurological assessment, especially when there are time constraints. We suggest the following to improve the efficiency of assessment:
Start by making a list of all physical symptoms. Patients with functional disorders typically have multiple physical symptoms. Making a list at the beginning avoids symptoms cropping up later, helps to build rapport, and allows an early appreciation of the main difficulties. Always ask about fatigue, pain, sleep disturbance, memory and concentration symptoms, and dizziness. It may seem counterintuitive to be seeking more symptoms in someone who is already polysymptomatic, but sometimes these symptoms, especially fatigue, are reluctantly volunteered even though they often cause the most limitation.
Dissociative symptoms. Dizziness, if present, may turn out to be dissociative in nature (e.g., feeling “spaced out,” “there, but not there,” or “unreal”). Patients often have trouble describing dissociation, partly because it is hard to describe but also because they fear the symptoms indicate “craziness.” Depersonalization describes feeling disconnected from your own body; derealization is a feeling of being disconnected from your surroundings ( ![]() ).
).
Onset. The onset in patients with weakness and movement disorders is sudden in approximately half of patients. Physical injury, pain, or acute symptoms of dissociation or panic are common in this situation. More gradual-onset symptoms are often associated with fatigue.
What can the patient do? Patients with functional symptoms have a tendency to report what they can no longer do rather than what they can do. Although it is helpful to hear about previous function, ask what they are able to do—do they enjoy it?
Look for other functional symptoms and syndromes (see Table 113.1 ). The more they have, the more likely it is that the presenting neurological complaint is functional. Some patients rotate between different specialists, with none appreciating their vulnerability to functional symptoms in general.
Ask the patients what they think is wrong and what should be done. If they or their family have been concerned or wondering about a specific neurological disease such as multiple sclerosis, Lyme disease, or “trapped nerves,” this information is important to tailoring an explanation for the diagnosis later on. Do they have health anxiety? Do they think they are irreversibly damaged? Efforts at rehabilitation may be futile unless beliefs about damage can be altered. In one prospective study of outpatients, beliefs about irreversibility predicted outcome more than age, physical disability, and distress ( ). What happened with previous doctors and why has the patient come to see you? Some patients seek diagnosis and treatment; others are simply looking for a label for a problem they do not expect to resolve.
Avoid blunt questions about depression and anxiety. It is not necessary for the purposes of neurological diagnosis to make an accurate assessment of a patient’s psychological state on the first visit. The diagnosis of a functional disorder should be made on the basis of the physical examination, not the presence or absence of psychological comorbidity. It often may be wise to leave questions about emotions for later; only a minority of patients with functional symptoms believe that stress or psychological factors have anything to do with their symptoms, in contrast to patients with disease who commonly attribute their symptoms to stress ( ). Patients with functional disorders do have high rates of depression and anxiety but are often wary of questions about their emotions. They often feel that the doctor is angling to blame their physical symptoms on them personally. Blunt questions like “Are you depressed or anxious?” may not therefore yield accurate answers. Instead try the following:
For depression, ask about activities they can do and whether they get enjoyment from them; if not, they may have anhedonia. If hospitalized, do they look forward to visits from friends and family? Look at the patient—is he or she miserable or avoiding eye contact? Or try framing questions around the physical symptoms: “Does your leg weakness get you down?” Depression is likely when there is persistent anhedonia or low mood most of the time, with four or more of the following: fatigue, sleep disturbance, suicidal ideation, poor memory or concentration, psychomotor retardation/agitation, or feelings of worthlessness/guilt.
For anxiety, look for three out of the following six symptoms: restlessness/on edge, insomnia, fatigue, irritability, poor concentration, and/or tense muscles combined with a history of worry that is persistent and hard to control. Worry will often be primarily focused on health.
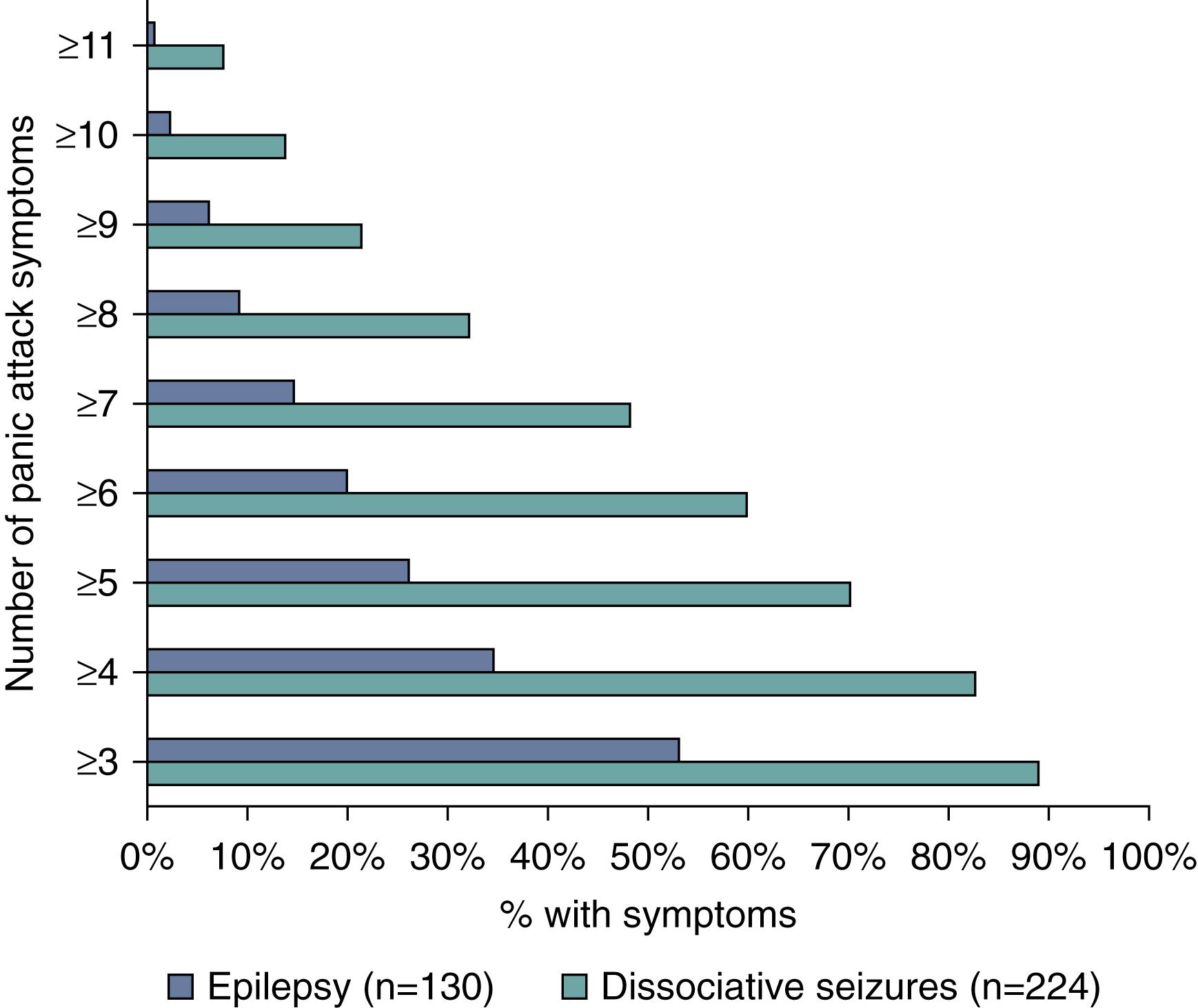
For panic attacks, look for four of the following: palpitations, sweating, trembling/shaking, shortness of breath, choking sensation, chest pain/pressure, nausea/feeling of imminent diarrhea, dizziness, derealization/depersonalization, afraid of going crazy/losing control, afraid of dying, tingling, or flushes/chills. Panic is a very common problem in patients with functional symptoms, especially nonepileptic attacks. Typically, they are not reported as panic attacks at all, but rather attacks where the patient unexpectedly had multiple symptoms all at once. The emotional component of the panic attack is experienced but erroneously attributed by the patient as being an understandable fear about the physical “attack” that is occurring.
Do not always expect psychological comorbidity or life events. Depression and anxiety are common, but approximately one-third of patients will have neither. Likewise, although some patients have a history of a recent life event or stress, this is only a risk factor in some patients and in others it is not present ( ). Sometimes the panic attack or physical injury that triggered the symptom is the most stressful life event, and the presence of the symptom then serves to perpetuate the anxiety. Avoiding a diagnosis of functional symptoms in someone because they are psychologically “normal” is as great an error as making the diagnosis simply because the patient has a lot of obvious psychological comorbidity.
Patient Describing Dissociation at Onset of Functional Left Hemiparesis and Functional Left Facial Spasm. Patient describing dissociation—facial spasm.
The diagnosis of functional symptoms should always be made on the basis of either:
Clinical features typical of a functional neurological disorder (e.g., a typical thrashing dissociative [nonepileptic] attack with side-to-side head movements and eyes closed for 5 minutes); or
Physical signs demonstrating internal inconsistency (e.g., Hoover sign for functional weakness, entrainment in functional tremor—see later discussion).
Mistakes are more likely when (1) too much weight is placed on the presence of a psychiatric history; (2) the diagnosis is made just because the problem is bizarre or unfamiliar; (3) there is failure to consider the possibility of a comorbid neurological disease (e.g., dissociative attacks and epilepsy in the same patient); or (4) when the assessing clinician is unfamiliar with a wide range of unusual neurological disorders ( ).
La belle indifference (smiling indifference to disability) has no diagnostic value because it is just as commonly present in neurological disease ( ). When it is present, it often reflects a conscious desire on the patient’s behalf to appear happy in a situation where he or she is concerned that someone will make a psychiatric diagnosis, or alternatively may indicate factitious disorder.
Dissociative (nonepileptic) attacks, also commonly called psychogenic nonepileptic seizures, are the most common type of symptom unexplained by disease seen in neurological practice ( ). Studies have estimated that up to one in seven patients in a “first fit” clinic, 50% of patients brought in by ambulance in apparent status epilepticus, and approximately 20%–50% of patients admitted for videotelemetry have this diagnosis. Mean age of onset is in the mid-20s, but peak is late teens; females predominate 3:1. Later-onset patients in their 40s and 50s have a 1:1 gender ratio and typically have health anxiety and a history of recent “organic” health problems ( ).
Dissociative attacks most frequently involve shaking movements of the limbs with impaired awareness for the attack. The movement seen is usually a tremor rather than a jerk. Approximately 20% of attacks resemble syncope more than epilepsy and consist of the patient falling down and lying still with their eyes shut for more than 2 minutes ( ); very few other conditions lead to this clinical scenario. Occasionally, attacks similar to complex partial seizures may be seen. Drop attack semiology without loss of awareness can also be seen in patients who are recovering from or subsequently develop dissociative attacks, suggesting a continuity of these phenotypes in some patients.
The diagnosis is usually made on the basis of the observable features of an attack, preferably recorded using video electroencephalography (EEG) ( Table 113.2 ; ). No one feature should be used on its own to make a diagnosis, but some are more reliable than others ( ). Data on the reliability of these signs have largely been taken from studies of videotelemetry; these signs are less reliable when based on witness descriptions.
| Dissociative Attacks | Epileptic Seizures | |
|---|---|---|
| Helpful | ||
| Duration over 2 min ∗ | Common | Rare |
| Fluctuating course ∗ | Common | Rare |
| Eyes and mouth closed ∗ | Common | Rare |
| Resisting eye opening | Common | Very rare |
| Side-to-side head or body movement ∗ | Common | Rare |
| Opisthotonus, arc de cercle | Occasional | Very rare |
| Visible large bite mark on side of tongue/cheek/lip | Very rare | Occasional |
| Dislocated shoulder | Very rare | Occasional |
| Fast respiration during attack | Common | Ceases |
| Grunting/guttural ictal cry sound | Rare | Common |
| Weeping/upset after a seizure ∗ | Occasional | Very rare ‡ |
| Recall for period of unresponsiveness ∗ | Common | Very rare |
| Thrashing, violent movements | Common | Rare |
| Postictal stertorous breathing ∗ | Rare | Common |
| Pelvic thrusting ∗ , † | Occasional | Rare § |
| Asynchronous movements ∗ , † | Common | Rare |
| Attacks in medical situations | Common | Rare |
| Not So Helpful | ||
| Stereotyped attacks | Common | Common |
| Attack arising from sleep | Occasional | Common |
| Aura | Common | Common |
| Incontinence of urine or feces ∗ | Occasional | Common |
| Injury ∗ | Common ¶ | Common |
| Report of tongue biting ∗ | Common | Common |
∗ Endorsed by a systematic review ( ).
† These signs unhelpful in distinguishing nonepileptic attacks from frontal lobe seizures.
§ Frontal lobe epilepsy. Dissociative attacks do sometimes appear to arise from sleep, but video electroencephalogram (EEG) usually shows this not to be true sleep. Attacks arising from EEG-documented sleep are suggestive of epilepsy.
Attention has shifted in recent years to diagnosis using subjective experience of the attack. Patients with dissociative attacks typically do not volunteer a prodrome. Indeed, studies analyzing dialogue between neurologists and patients have shown that the lack of any attempt to describe a prodrome may be of diagnostic value in itself because patients with epilepsy usually do attempt to describe their prodrome when present, compared with patients with dissociative attacks who describe the disability associated with the attack ( ). However, if questioned, many patients with nonepileptic attacks will admit to a brief prodrome with features of panic ( ; Fig. 113.1 ). If obtained, this is useful information that gives the clinician windows into understanding both the nature of the attacks (a mechanism related to panic attacks in which the patient dissociates) and possible treatment (teaching the patient distraction techniques to use during this warning phase to avert the attack and following treatment principles for panic disorder). As some patients recover, they may experience awareness during the attack itself.
Video EEG may be supplemented by an open suggestion protocol to help record an attack ( ). Deceptive placebo induction with saline or a tuning fork is more controversial. Postictal prolactin measurement (to detect high prolactin after a generalized seizure) has fallen out of favor owing to problems with the reliability and timing of the test. Common diagnostic pitfalls include coexistent epilepsy (present in 5%–20% of patients), frontal lobe seizures, sleep-related movement disorders, and paroxysmal movement disorders.
Weakness as a functional symptom is more common in females and typically presents in the mid-30s but like all functional symptoms can occur in children and the elderly. Estimates of incidence are approximately 5/100,000, comparable with multiple sclerosis. Comorbidity with other functional symptoms, especially fatigue and pain, is almost invariable. The most common presentation is unilateral weakness, followed by monoparesis and paraparesis. There is no good evidence for left-sided or nondominant preponderance. Complete paralysis is less common clinically than weakness ( ).
The onset is sudden in approximately 50% of patients. In the acute presentation, there are often symptoms of a panic attack, dissociative seizure, or an immediate trigger such as a physical injury, acute pain, migraine, a general anesthetic, or an episode of sleep paralysis ( ). When the onset is more gradual, there is typically a history of fatigue, pain, or immobility on which the weakness becomes superimposed gradually over time. The weakness seen in complex regional pain syndrome type 1 (CRPS-1) ( ) has the same clinical features as functional weakness .
Subjectively, patients with functional weakness often report that the affected limb “doesn’t feel as if it belongs” to them or, in extreme situations, as if it is “not there” or is “someone else’s” limb ( ![]() ). They commonly report that the leg gives away or that they keep dropping things unexpectedly. The diagnosis depends on demonstrating internal inconsistency and incongruence with disease:
). They commonly report that the leg gives away or that they keep dropping things unexpectedly. The diagnosis depends on demonstrating internal inconsistency and incongruence with disease:
Pattern of weakness. In functional weakness, the limb is usually globally weak or often demonstrates the inverse of pyramidal weakness, with the flexors weaker in the arms and the extensors weaker in the legs.
Inconsistency during examination. This may be obvious—for example, a patient who can walk to the examination table but cannot raise the leg against gravity on examination. More commonly there is weakness of ankle movements, but the patient can stand on tiptoes or on their heels. Arm weakness may be incompatible with performance, such as removing shoes or carrying a bag.
Hoover sign. Hip extension must be weak for this test to work. The presence of hip extension weakness itself in an ambulant patient is a positive sign of functional weakness. If hip extension returns to normal during contralateral hip flexion against resistance, this demonstrates structural integrity of the motor pathways ( Fig. 113.2 ; ![]() ). The test is easiest to do with the patient in the sitting position. We find it useful to demonstrate this sign to the patient and relatives to indicate that the diagnosis is being made on the basis of positive criteria. This test may be false positive when there is cortical neglect.
). The test is easiest to do with the patient in the sitting position. We find it useful to demonstrate this sign to the patient and relatives to indicate that the diagnosis is being made on the basis of positive criteria. This test may be false positive when there is cortical neglect.
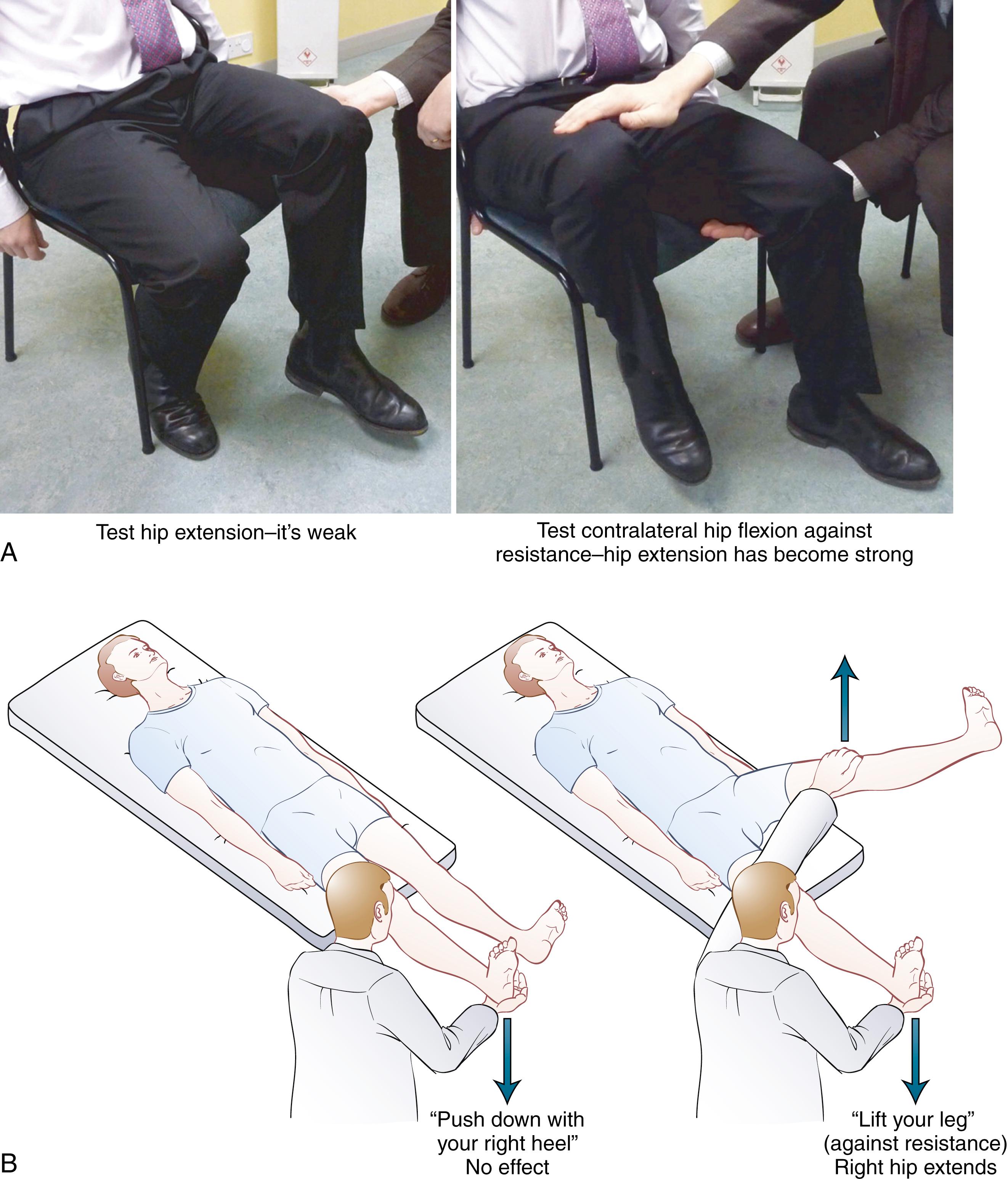
Hip abductor sign. A similar test involves demonstrating weakness of hip abduction, which returns to normal with contralateral hip abduction against resistance.
Dragging gait. If there is moderate or severe unilateral leg weakness, the patient may walk with a dragging gait in which the foot does not leave the ground. Often the hip is externally or internally rotated ( Fig. 113.3 ).

“Give-way” weakness. This is a pattern of weakness in which the patient transiently has normal power but then the limb gives way, sometimes just before it is touched. If the arm is very weak, it may hover for a second before collapsing. Normal power can be produced by saying to the patient, “At the count of 3, push—1 … 2 … 3 … push. ” This is a less reliable sign and occurs more commonly in painful limbs or occasionally in myasthenia gravis.
Drift without pronator sign. Sometimes patients with functional arm weakness will demonstrate a downward drift of the arm without the pronation seen in conditions such as stroke ( ).
Facial spasm (looking like weakness) ( ![]() ). It is not uncommon to see patients who apparently have weakness of their face, usually ipsilateral to a functional hemiparesis ( ). In fact, the appearance is nearly always due to unilateral overactivity of the platysma muscle which pulls the side of the lip downwards. There may be jaw deviation and sometimes an upward deviation of the mouth instead. Contraction of the orbicularis oculi muscle can lead to an appearance with a depressed eyebrow ( Fig. 113.4 ), which may be interpreted incorrectly as ptosis, although true functional ptosis does occur more rarely. These features can sometimes be enhanced on examination by sustained voluntary contraction of facial or periocular muscles.
). It is not uncommon to see patients who apparently have weakness of their face, usually ipsilateral to a functional hemiparesis ( ). In fact, the appearance is nearly always due to unilateral overactivity of the platysma muscle which pulls the side of the lip downwards. There may be jaw deviation and sometimes an upward deviation of the mouth instead. Contraction of the orbicularis oculi muscle can lead to an appearance with a depressed eyebrow ( Fig. 113.4 ), which may be interpreted incorrectly as ptosis, although true functional ptosis does occur more rarely. These features can sometimes be enhanced on examination by sustained voluntary contraction of facial or periocular muscles.

“Altered” reflexes. Occasionally, patients with functional weakness may have what appears to be ankle clonus, which on closer inspection has features of functional tremor. There may also appear to be reflex asymmetry if the patient is co-contracting agonist and antagonist muscles on one side of their body. Finally, in our experience it is not that unusual for the plantar response to be relatively mute on the affected side if there is marked sensory disturbance.
Long-standing Functional Left Arm and Leg Weakness and Sensory Disturbance. Functional hemiparesis including patient’s description of arm and leg, dragging gait with inverted ankle, and altered perception of ankle position.
Right-Sided Functional Leg Weakness With a Positive Hoover Sign. Hoover sign with right leg weakness.
Functional Facial Spasm Showing Contraction of Platysma on the Right With Jaw Deviation to the Right. Functional facial spasm.
Functional movement disorders have been increasingly recognized by movement disorder specialists, especially over the past decade ( ). In specialist clinics, these symptoms account for up to 10% of new referrals ( ). Like weakness, the onset of functional movement disorders is often sudden or may be accompanied by pain ( ). The course may be unusual, with sudden remissions or relapses in different limbs. General clues to a functional movement disorder include improvement with distraction (many so-called organic movement disorders get worse during distraction) and worsening with attention. Many organic movement disorders, especially gait disorders, can look bizarre, but if a clinician is careful to make the diagnosis only on positive grounds, it should not be as intimidating a diagnosis as it first appears. Gupta and Lang proposed a revised classification in which clinically definite cases included cases documented through resolution with placebo or psychotherapy and cases clinically established with clear positive evidence on examination and laboratory supported with electrophysiology ( ). Caution is warranted insofar as organic movement disorders can also improve temporarily with placebo and because functional and organic movement disorders commonly exist together.
Tremor is the most commonly encountered functional/psychogenic movement disorder ( ; ). There are a number of positive clinical features, none of which are 100% reliable, that should enable a positive diagnosis to be made:
Variable frequency, which may include starting and stopping of the tremor, is more useful than variable amplitude, which can be found in organic tremor.
The entrainment test is carried out by asking the patient, with the unaffected limb, to copy a rhythmical tapping movement provided by the examiner, preferably using thumb and forefinger. The movement should be altered in frequency while the patient is trying to copy it, to bring out the features described as follows. If the tremor is in the legs, ask the patient to copy foot tapping movements. If it is in the trunk, then tongue or neck movements may be used. Mental distraction tasks such as mental arithmetic tend to be less effective distractors in functional tremor. In functional tremor, one of three things happens: (1) the patient is unable to copy the simple tapping movement and cannot explain why; (2) the tremor in the affected limb stops; or (3) the tremor in the affected hand entrains to the same rhythm as the examiner. False positives in this test appear to be rare, although, as with any positive functional sign, they do not exclude the possibility of an additional underlying “organic” movement disorder. In contrast, false negatives are more common, particularly if the tremor is long-standing or if the tremor relies on mechanics. For example, a heel-tapping leg tremor in someone sitting with their foot plantar-flexed on the ground is characteristic of a functional tremor ( ). Tremor recording, if available, can be helpful in recording the response to this test.
Ballistic movements. Ask the patient to make sudden ballistic movements with the good hand by touching the rapidly moving finger of the examiner. Functional tremor will often stop briefly during the movement.
Attempted immobilization. Attempting to immobilize the affected limb often makes a functional tremor worse. Likewise, loading the limb with weights tends to make the tremor worse, whereas organic tremor tends to improve with this maneuver.
Coactivation sign. Most functional tremor is similar to voluntary tremor. Sometimes the mechanism of the tremor is different and relates to coactivation of agonist and antagonist muscles (like shivering).
Coherence analysis. If functional tremor is present in more than one limb, it usually has the same frequency. In contrast, organic tremor usually has slightly different frequencies in different body parts. Therefore demonstrating coherence of the tremor between different body parts can provide supportive evidence of a functional tremor.
The addition of slowness and postural instability to a patient with functional tremor can give the appearance of Parkinson disease, especially if the patient is also depressed and has diminished facial expression. The slowness is distractible and without the normal decrement seen in parkinsonism ( ). There may be stiffness but with a quality of active resistance to it. Fluorodopa positron emission tomography (PET) scanning or dopamine transporter single-photon emission computed tomography (SPECT) scanning should be normal in functional movement disorder patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here