Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endoscopic sinus and skull base surgery has become an effective part of the management of chronic rhinosinusitis (CRS) and tumors of the sinuses and anterior skull base. Technologic advances have been critical in advancing endoscopic surgical procedures, with the introduction of improved optics and lighting, advanced instrumentation, and image-guided surgical navigation. Hemostatic materials and devices have similarly evolved to assist in the management of the surgical field and postoperative cavity.
The vast majority of inflammatory frontal disease can be treated with a well-performed Draf I or Draf IIa dissection. Common causes of continued disease after a complete Draf IIa dissection include membranous stenosis, middle turbinate lateralization, osteitis, neo-osteogenesis, and prominence of the nasofrontal beak.
Extended endoscopic approaches offer improved exposure of the frontal sinus and may be preferred over external approaches in some cases. Table 10.1 describes the advantages of such endoscopic approaches. Extended frontal sinus approaches are also useful for the resection of benign and malignant tumors of the frontal sinus. The procedure has helped to expand endoscopic techniques to include recalcitrant frontal sinus disease, frontal sinus mucoceles, cerebrospinal fluid (CSF) leaks, frontoethmoid fractures, frontal sinus tumors, and endoscopic skull base surgery. The procedure also improves the postoperative delivery of topical irrigation and tumor surveillance.
|
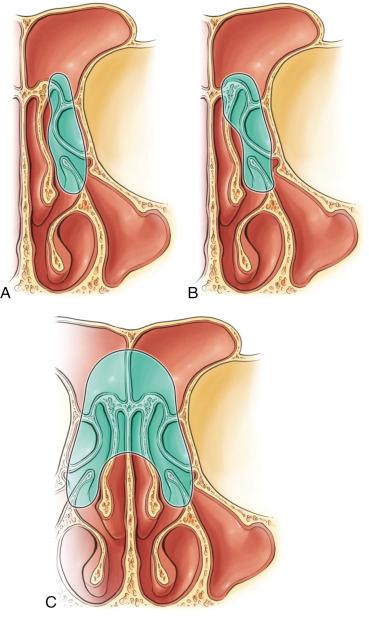
The Draf IIb procedure is an extension of the Draf IIa dissection in the medial direction, with partial removal of the anterior-superior middle turbinate and frontal sinus floor. As in basic frontal sinus surgery, it is critical to preserve mucosa and avoid exposed bone wherever possible. Ideally, complete Draf IIa dissection is performed before progressing to Draf IIb dissection.
Patients undergoing extended frontal approach procedures often have challenging anatomy; the use of image guidance is preferred in these cases. The progression to Draf IIb dissection commits both the patient and the surgeon to more meticulous and prolonged postoperative care.
The reader is referred to Chapter 9 for discussion and illustration of the anatomy of the frontal recess, anterior ethmoid region, and accessory frontal cells. Given the high degree of variability in pneumatization of the sinus, certain basic relationships are important to understand. The frontal sinus is a pyramidal, funnel-shaped structure. It is divided in the midline by an intersinus septum and may contain an intersinus cell. The intersinus septum separates the paired sinuses and is a surgical target for maximal expansion of outflow.
Extended frontal sinus approaches seek to remove the floor of the frontal sinus for maximal enlargement of the outflow pathway. Fig. 10.1 shows the dissection boundaries for the Draf classification of extended frontal sinus approaches. The nasofrontal beak is the variably thick bony projection at the junction of the nasal and frontal bones. If this structure is prominent, it may narrow frontal sinus outflow. The anterior limit of dissection is the periosteal layer of the superficial glabellar cutaneous tissue. Lateral boundaries of the frontal sinus floor consist of the medial orbital wall and orbital roof. These structures are generally left undisturbed during extended frontal sinus approaches.
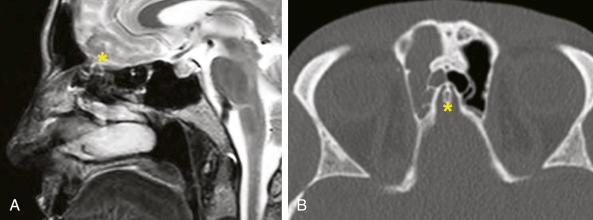
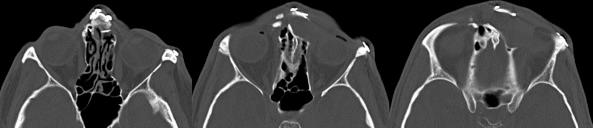
The olfactory fossa is the lowest point in the floor of the anterior cranial base. The skull base slopes downward in a lateral to medial direction in the coronal plane and in an anterior to posterior direction in the sagittal plane. The degree of slope is highly variable and should be studied on preoperative images. The olfactory fossa contains an anterior projection into the frontal sinus that is most easily seen in axial view ( Fig. 10.2 ). The distance from this projection to the anterior table of the frontal sinus is referred to as the anterior-posterior (A-P) diameter.
The cribriform plate of the ethmoid bone may vary in depth and slope and is often asymmetric.
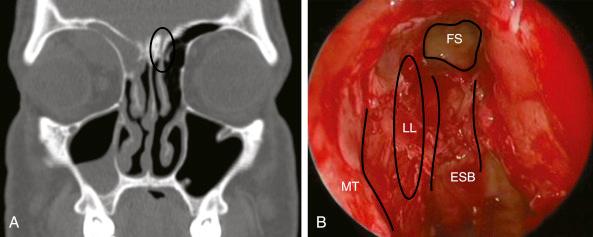
The middle turbinate is expected to insert into the lateral lamella of the cribriform plate. In many patients, the most anterior aspect of the middle turbinate lies anterior to the cribriform plate and may insert into the floor of the frontal sinus.
The anterior aspect of the middle turbinate offers a reliable landmark to identify the locations of the frontal sinus and olfactory fossa ( Fig. 10.3 ).
Indications for extended frontal sinus surgery include
failed prior frontal surgery, often associated with neo-osteogenesis or lateralized middle turbinate remnant ( Fig. 10.4 )
mucocele ( Fig. 10.5 )
frontal sinus unobliteration
need for surgical access (treatment of type 3 or type 4 frontal cell, intersinus septal cell)
benign or malignant tumor
repair of CSF leak or encephalocele
select trauma cases
Relative contraindications for extended frontal sinus surgery include
extremely narrow A-P diameter
severe bilateral neo-osteogenesis
lesions requiring access to the lateral aspect of a well-pneumatized frontal sinus
medical comorbidities precluding general anesthesia
The disease process, radiologic findings, and goals of surgery should be reviewed thoroughly before making the decision as to which approach is most favorable.
The risks of surgery, including CSF leak, orbital injury, hemorrhage, smell dysfunction, and possible recurrence of disease, should be discussed fully with the patient well in advance of surgery.
The possible need for adjunctive open approaches should be entertained and discussed.
Postoperative care expectations should be agreed upon, including follow-up, débridement, and medication regimens.
Preoperative medical treatment with agents such as antibiotics and systemic corticosteroids may be necessary to optimize intraoperative hemostasis and visualization.
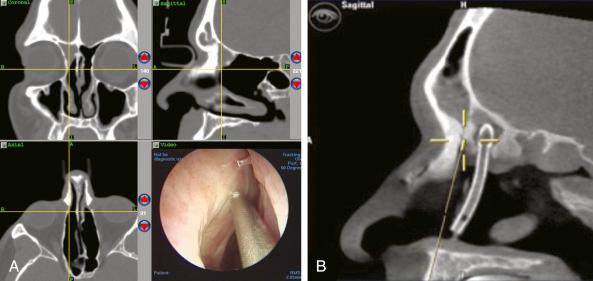
Thoroughly review fine-cut computed tomographic (CT) scans in the coronal, axial, and sagittal planes. Actively scrolling through the scans on a computer workstation is helpful to create a three-dimensional understanding of the anatomy.
Examine the A-P dimension in both axial and sagittal planes. Smaller dimensions indicate a more technically challenging surgery and ultimately a smaller sinusotomy, which may yield a worse long-term prognosis.
It is often quoted that a minimum A-P dimension of 10 mm is required, but in reality there need only be enough room for the drill to fit comfortably without the back end of the bur violating the cribriform plate or posterior table of the sinus ( Fig. 10.6 ).
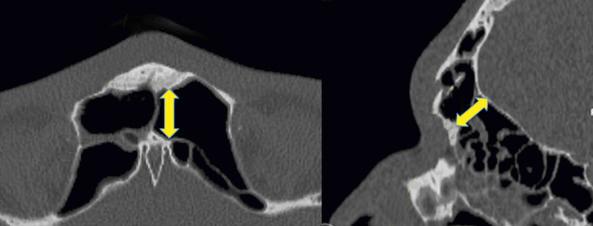
Assess the thickness of the nasofrontal beak because this can be drilled out to increase the A-P dimension.
Identify the middle turbinate or middle turbinate remnant. This will serve as a surgical landmark. Its anterior insertion is helpful to note preoperatively, as is the presence of lateralization, osteitis, or neo-osteogenesis.
Establish the location of the anterior ethmoid artery and note its presence within the skull base or hanging in a mesentery. If the anterior ethmoid artery is in a mesentery, bipolar cautery may be used early in the procedure to prevent risk of inadvertent injury.
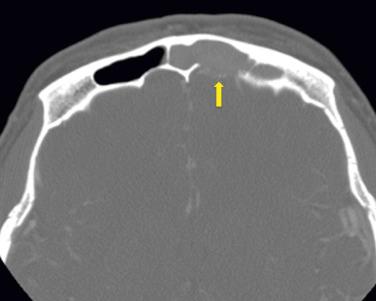
Look for the presence of a skull base defect. It is not uncommon for a mucocele or postobstructive tumor secretions to demineralize the anterior and/or posterior table of the frontal sinus. Posterior table dehiscence warrants more careful introduction of instruments ( Fig. 10.7 ).
In the case of a tumor or CSF leak or encephalocele, determine the presence, location, and size of the potential skull base defect to decide on the optimal surgical approach. Magnetic resonance imaging (MRI) aids in the diagnosis of mucocele, tumor, and CSF leak or encephalocele. It may also be helpful in postoperative examination of patients who have previously undergone fat obliteration, although findings are highly variable in this population. MRI is helpful to distinguish tumor from inspissated secretions and to identify the location and size of a skull base defect.
If far lateral dissection is expected, an adjunctive open approach, such as a trephine or osteoplastic flap, may be anticipated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here