Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The tarsal navicular lies in the uppermost portion of the medial longitudinal arch of the foot between the head of the talus and the three cuneiforms. The proximal concave articular surface and convex distal articular surface makes the navicular uniquely shaped as the keystone of the arch by connecting the talus of hindfoot to the cuneiforms of the midfoot and allowing for pronation and supination of the transverse tarsal joint during gait.
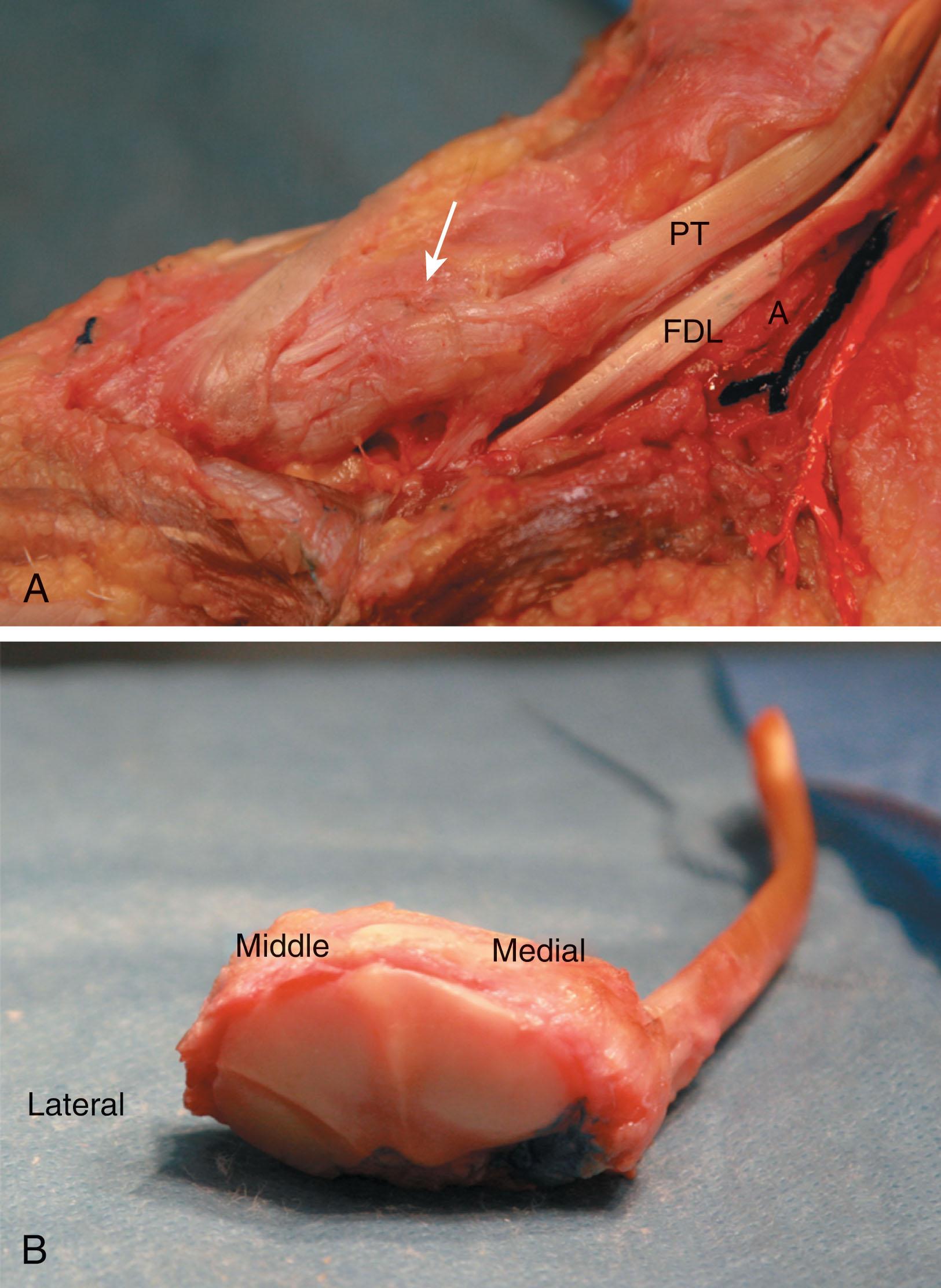
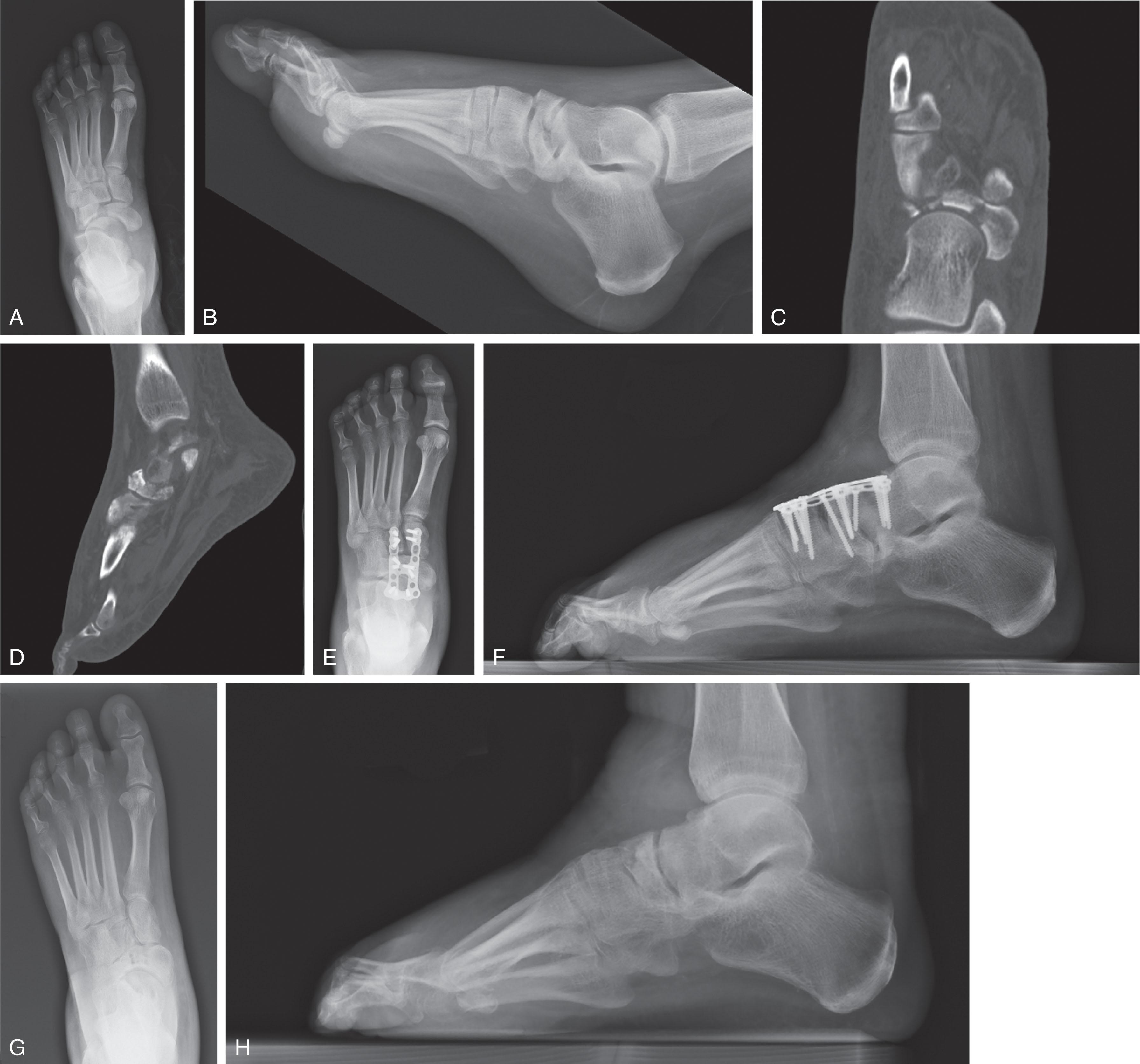
The posterior tibial tendon inserts on the medial tuberosity to invert and supinate the foot. There are multiple ligament attachments, the strongest of which is the confluence of the dorsal talonavicular ligament with the tibionavicular ligament to form the anterior division of the superficial deltoid ligament on the medial side. The spring ligament originates on the sustentaculum tali of the calcaneus, travels under the talar head, and then inserts on the plantar medial navicular. Cuneonavicular ligaments are located plantarly and dorsally and the interosseous cuboideonavicular ligaments arise laterally ( Fig. 47-1 ).
The navicular, via the spring ligament attachment to the anterior process of the calcaneus, cups the talar head to form the acetabulum pedis. The socket originally described by Sarrafian allows the foot to swivel around the head of the talus as the subtalar joint everts during heal strike and the transverse tarsal joints are parallel, allowing flexibility and shock absorption. The subtalar joint inverts during the push-off phase of gait and the talonavicular and calcaneocuboid joints become nonparallel and locked. Motion at the talonavicular joint is critical for normal subtalar function during gait as isolated talonavicular fusion can lead to up to 90% loss of supination.
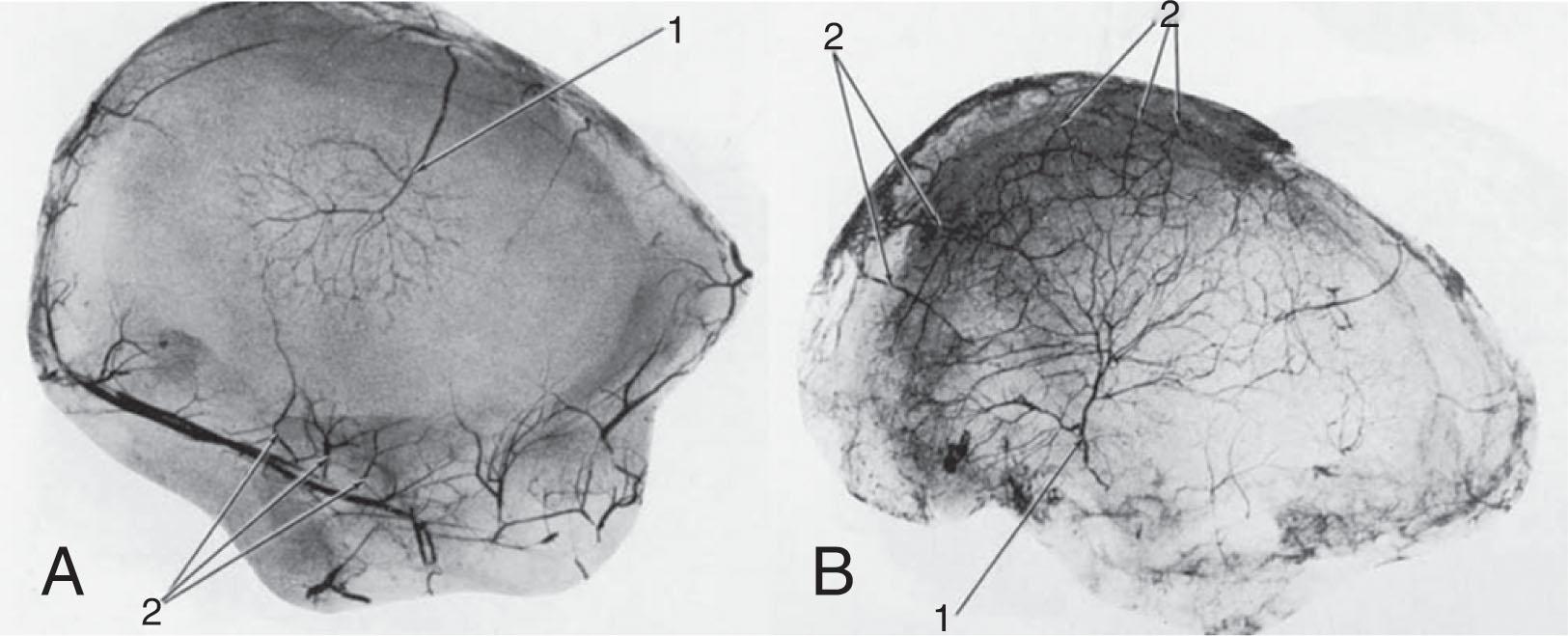
The navicular is covered nearly completely with cartilage, and the blood vessels can enter over a limited number of surfaces; thus the blood supply is crucial to healing potential. Branches from the dorsalis pedis artery contribute dorsally and the posterior tibial artery provides plantar perfusion. A medial confluence of dorsal and plantar vessels serves the tuberosity. A microangiographic study by Torg noted there was an avascular watershed area in the central third. However, findings by McKeon et al suggested that most cadaveric specimens had a robust intraosseous navicular blood supply ( Fig. 47-2 ).
Navicular fractures are often categorized as avulsion fractures, stress fractures, tuberosity fractures, or body fractures. Multiple subclassifications of body fractures have been proposed.
The talonavicular ligament creates a bony avulsion from the navicular as the foot is forcibly plantar flexed and inverted. This low-energy fracture pattern is also called a dorsal lip or “chip” fracture and is the most common, representing 47% of the navicular fractures.
Patients usually report pain, swelling, and difficulty walking and increased pain with plantar flexion. Physical examination reveals dorsal midfoot swelling with ecchymosis and focal tenderness at the talonavicular joint. The lateral radiograph will best demonstrate the displacement of the fracture. When an avulsion fracture is seen, concomitant midfoot and lateral ankle injuries often exist.
Conservative treatment and can lead to good clinical outcomes in the long term. If the size of the fragment is small, a compression dressing may provide relief. If the fragment is large, or if the patient is unable to tolerate compression, a controlled ankle movement (CAM) walker boot or a short-leg walking cast may be considered for additional support. Concomitant injury to the midfoot or lateral ligaments may impact timing of weight-bearing. Typically, patients are immobilized for 2 to 4 weeks followed by activity progression as comfort allows.
Indications include finding an irreducible dislocation or significant midtarsal subluxation secondary to the size of the fracture fragment. A dorsally or medially based incision can be used to visualize the fragment and to perform an open reduction and internal fixation with screws or a plate. In the chronic setting, surgical intervention may be beneficial for a painful nonunion, dorsal prominence, subluxation, or posttraumatic arthritis. Most commonly, the fracture fragment is small and can simply be excised.
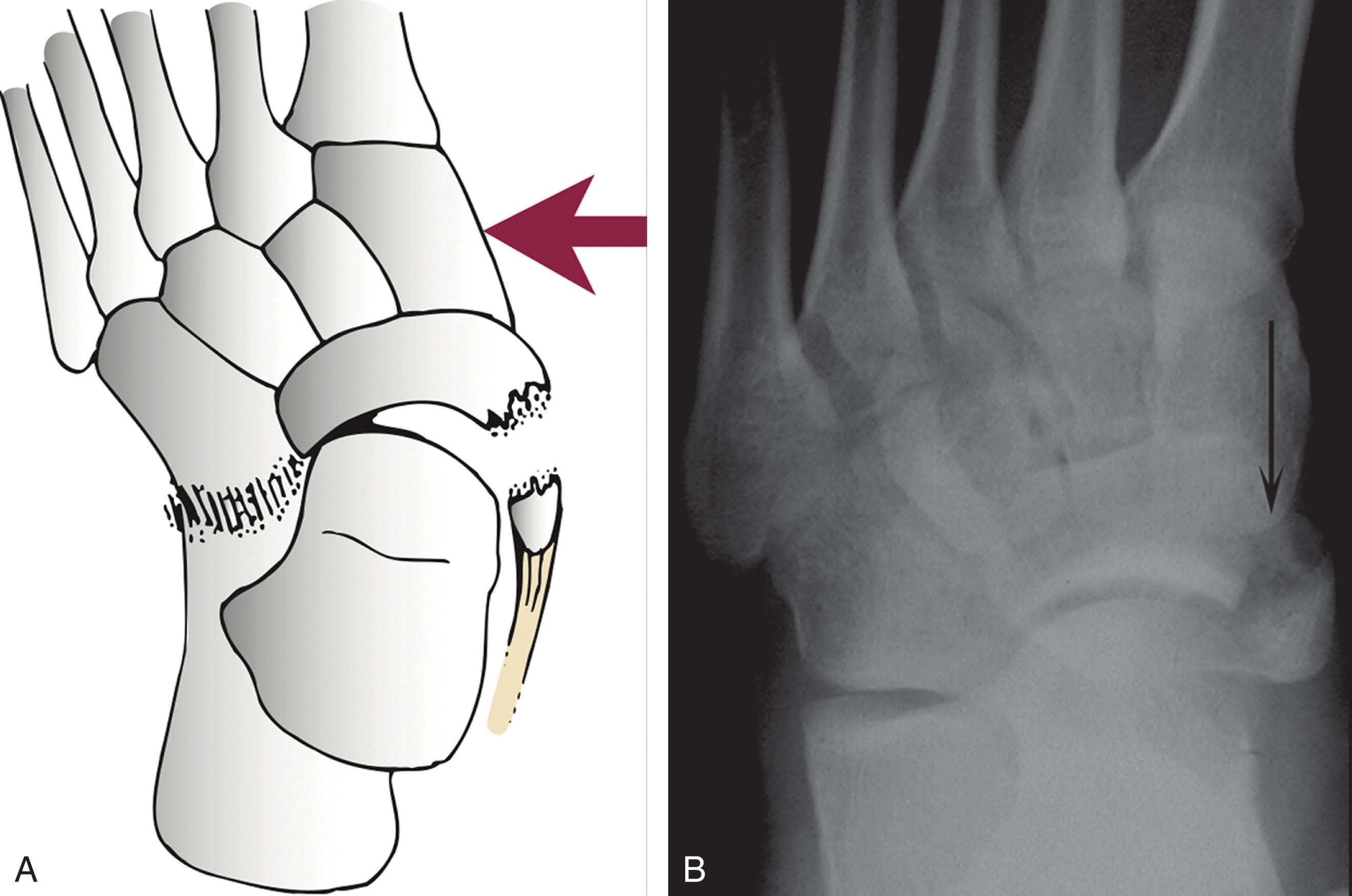
With forced eversion of the foot, the posterior tibial tendon and deltoid ligament can cause the tuberosity to fail in tension ( Fig. 47-3 ). Medial foot pain with weight bearing after a twisting mechanism is common, and pain may be increased with active inversion or passive eversion of the foot.
Nonoperative management is generally recommended because most fractures are minimally displaced and if the fracture progresses to a nonunion, the sequelae of late operative intervention are minor. Patients can be immobilized in a walker boot for 4 to 6 weeks. An arch support may remove tension from the posterior tibial tendon. The tendon’s broad plantar insertion may allow retention of tendon function even with this fracture.
Surgical treatment is recommended for large fragments or significantly retracted fragments in which osseous union is unlikely, or prominence would be symptomatic. Direct visualization can be obtained from a medial incision and lag screws can be placed. Postoperatively, the patient is placed in a splint for 2 weeks and then converted to a short-leg walking cast or a walker boot.
For patients with a symptomatic nonunion, excision of the nonunion fragment and advancement of the posterior tibial tendon with bone anchors or suture tunnels may be beneficial.
The most common mechanism is a direct axial load after a fall from height and landing on the foot. Other proposed mechanisms include forced plantar flexion with abduction of the midtarsal joints. This mechanism would lead to a vertical talar body fracture and dorsal dislocation of a portion of the navicular. Main and Jowett suggested that the mechanism of these injuries was based on “swivel” of the foot about the axis of the talocalcaneal ligament combined with longitudinal load.
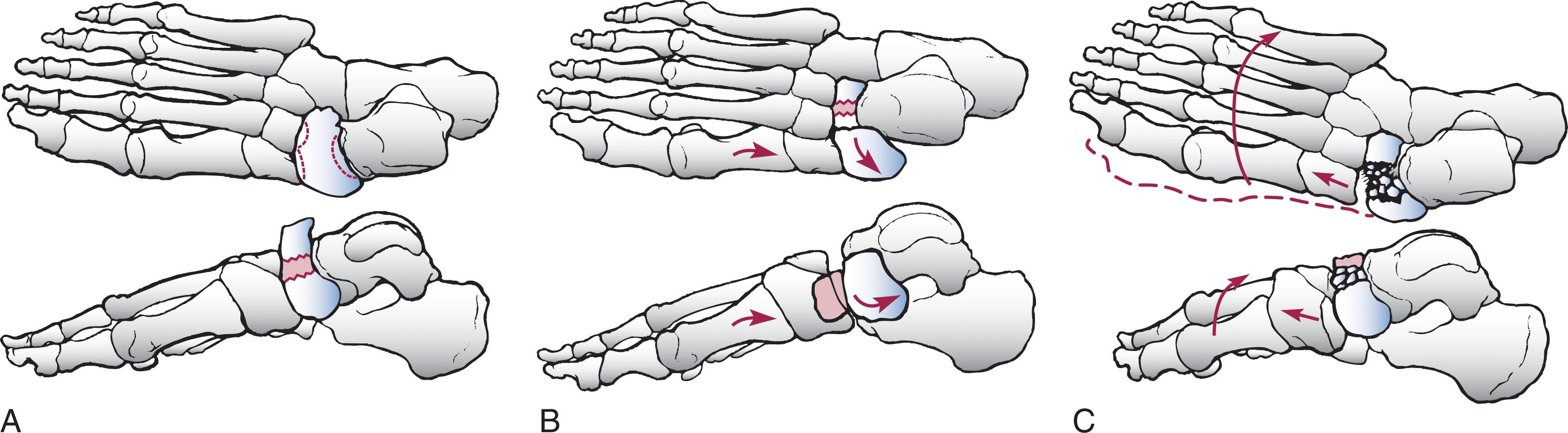
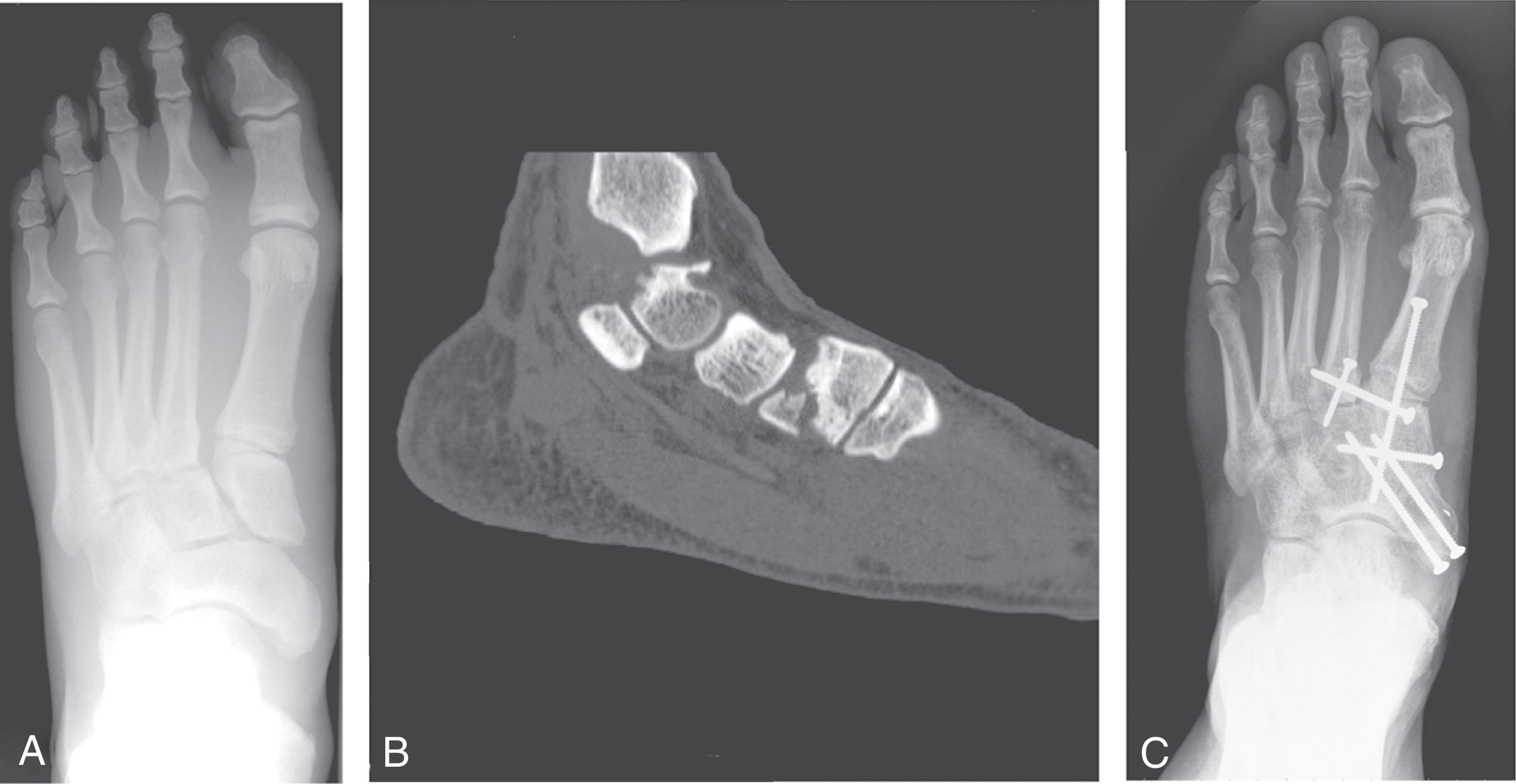
Sangeorzan et al described three types of navicular body fractures ( Table 47-1 ). Type 2 and 3 fractures have displacement secondary to the rotation of the foot on a flattened lateral navicular leading to apparent hindfoot varus ( Fig. 47-4 ). Schmid et al questioned the clinical predictability of the Sangeorzan classification and subsequently developed an updated classification system of navicular body fractures reflecting talonavicular joint damage, which they felt better correlated with prognosis (see Table 47-1 ). At average follow-up of 6 years, surgical fixation of 24 patients led to good outcomes but was closely related to fracture severity based on their system.
| Type | Sangeorzan 1989 | Schmid 2016 |
|---|---|---|
| 1 | Transverse in the coronal plane with a resultant dorsal fragment that is less than 50% of the navicular body. On the AP radiograph, the medial border of the foot must not be disrupted. | Two part fracture. |
| 2 | The most common type have a transverse fracture line from dorsolateral to plantar-medial. There may be a large dorsomedial fragment with plantar-lateral comminution. The calcaneonavicular joint is intact. | Multifragment fracture. |
| 3 | Central or lateral comminution. The medial fragment is subluxated or dislocated at the naviculocuneiform joint medially. Subluxation of the calcaneocuboid joint may occur as well. | Fracture with associated dislocation of the talonavicular joint or fracture of the talar head. |
Patients must be evaluated for any additional associated orthopedic injuries based on a high-energy injury mechanism such as motor vehicle collision or fall from height. Gross malalignment of the foot and severe swelling, ecchymosis, or tenderness at the midfoot may be present. Closed reduction and splinting in a padded splint with elevation and strict non–weight bearing is mainstay at acute presentation. Conservative treatment is reserved for patients with truly nondisplaced fractures of the navicular body, severe soft tissues injuries, those who will not ambulate, or those with medical comorbidities precluding surgery. Treatment is most predictable with complete non–weight bearing and immobilization until radiographic signs of union are seen.
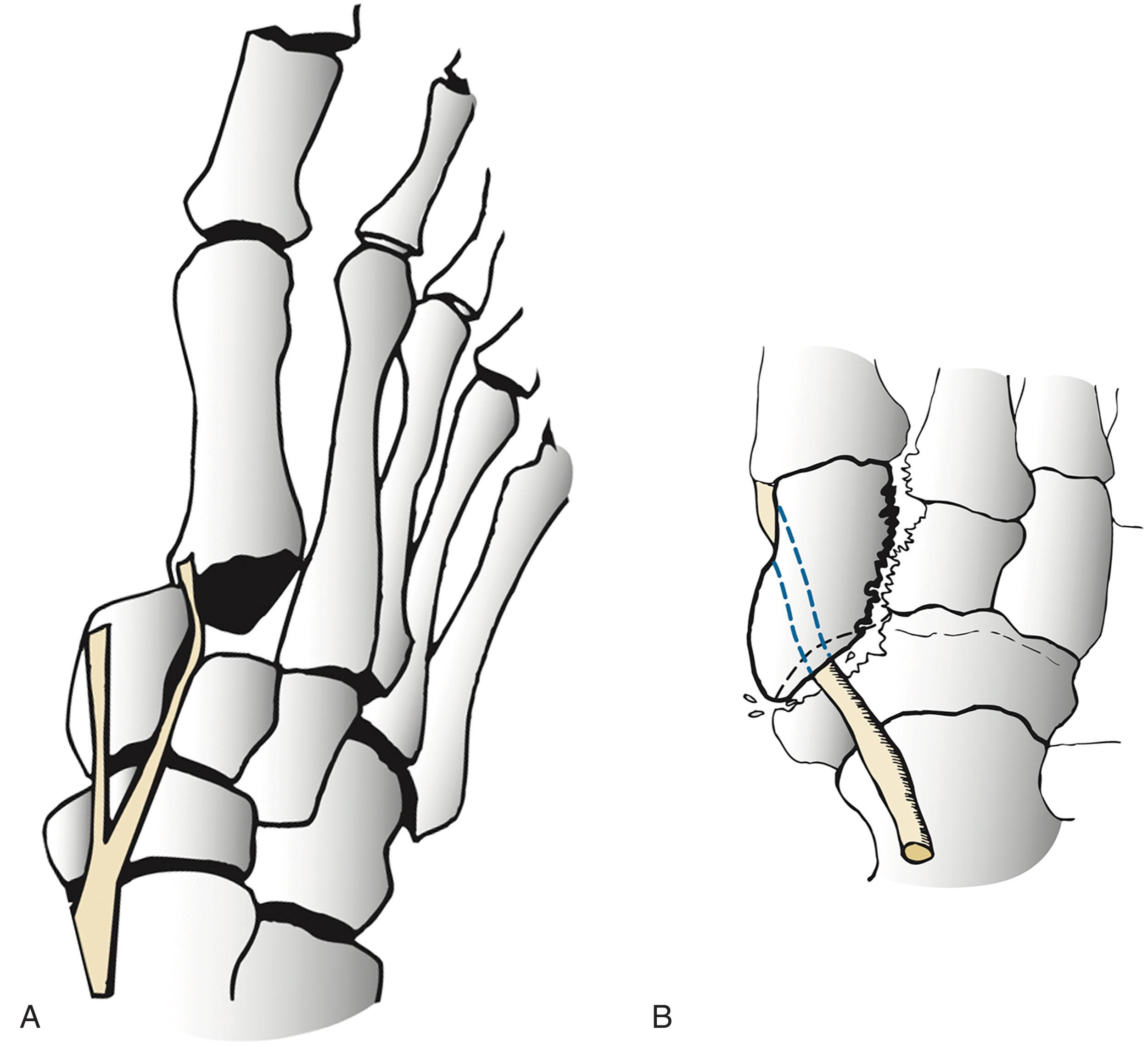
Multiple authors noted that with nonsurgical treatment, late deformities resulted in poor outcomes that led to osteoarthritis, medial column collapse, adduction, and a cavovarus foot. Most patients undergo closed reduction and splinting in the emergency department. Patients who have irreducible dislocations, open fractures, neurovascular compromise, or soft tissues that are at risk may necessitate urgent surgical intervention to obtain improved alignment and to decrease the amount of soft tissue swelling. Percutaneous pinning is useful in the acute setting to stabilize the fracture and/or dislocation and to decrease pressure on the soft tissues. This technique can also be used for definitive fixation if an acceptable reduction can be obtained closed. External fixation allows for further stability of the unstable dislocation. This technique is useful for patients with severe soft tissue injuries, grossly unstable comminuted fractures, or to supplement internal fixation ( Fig. 47-5 ).

Definitive management can be delayed based on swelling. Ideally, an anatomic reduction of the fracture and restoration of the talonavicular (TN) and navuculocuneiform (NC) joints is performed through an incision between the tibialis anterior and tibialis posterior tendons. Individual fragments can be manipulated with K-wires, pointed reduction forceps, or a dental pick, and a joint distractor can aid in visualization. The articular surface is inspected to determine whether it is salvageable or if a primary arthrodesis should be performed. Fracture fixation includes screw placement and compression when possible. For small fracture fragments, mini-fragment screws or bioabsorbable pins can be used for fixation of intraarticular fragments. Severely comminuted fractures are often treated with bridge plating. The goal of this treatment should be to restore column length and foot alignment even if these patients may eventually benefit from delayed arthrodesis ( Fig. 47-6 ). Patients are non–weight bearing for at least 8 to 12 weeks depending on radiographic signs of union ( Fig. 47-7 ).

Arthrodesis is generally reserved in the acute setting for only the most severely comminuted fractures that cannot be bridged because of instability. Eichenholtz and Levine as well as Main and Jowett recommended containing the fusion to the TN and NC joints. Garcia and Parks recommended that the degree of articular cartilage damage should guide the surgeon in the decision of whether and where to fuse. Hansen described “ankylosis” as an alternative in which the fracture fragments are fixed with screws, and when there is inadequate bone, the screws can be placed across the nonessential naviculocuneiform joints. The joints are not formally prepared for arthrodesis, and the lag screws are removed when the fracture has healed.
Delayed arthrodesis is useful for patients with posttraumatic arthritis, residual deformity after fracture union, or painful nonunion of the fracture.
The largest series was published by Richter et al and included 155 patients with fractures of the midfoot; however, only 50 of these patients had navicular fractures. At an average of 9 years' follow-up, patients with an isolated navicular fracture fixation had significantly ( P < 0.05) better function and better American Orthopaedic Foot and Ankle Society (AOFAS) scores than patients with Lisfranc or Chopart fracture dislocations.
Main and Jowett reported on 29 fractures of the navicular body. Eighteen of 24 displaced fractures had fair or poor results. Displacement seemed predictive of outcome because all five nondisplaced fractures had good or excellent results. Sangeorzan et al confirmed this in his report on 21 navicular body fractures. Of the 15 patients with satisfactory reduction, 14 had a good result. Patients who did not have a satisfactory reduction had worse clinical outcomes. These authors concluded that the type of fracture pattern and the quality of the reduction affect the patient's outcome.
Complications include avascular necrosis (AVN), collapse of the navicular, nonunion, medial column collapse, and posttraumatic arthritis. The goals of treatment are to restore a plantigrade and painless foot for the patient. Many patients require arthrodesis because of chondrolysis, posttraumatic arthrosis, or residual deformity ( Fig. 47-8 ). When possible, the arthrodesis should be limited to the joints with pain and deformity, and plantigrade alignment should be restored.
Although first described in the 1970s, it was in 1981 that Torg conducted a multicenter study that included 21 cases of navicular stress fracture. A 1994 report by Khan et al reported their high rate of occurrence in running and jumping athletes. They are often seen in men in their mid-twenties with a mechanism of overuse injury, and patients with an inflexible or cavovarus foot may be at increased risk. Patients usually give a history of insidious onset of a “cramping” or “soreness” in the dorsal or medial midfoot or anterior ankle that is poorly defined. Hunter reported increased pain when patients stood on their toes and exerted a downward pressure. Patients may have the most tenderness with pressure over the proximal dorsal navicular. Several authors have emphasized the importance in timely diagnosis in athletes because failure of diagnosis may result in fracture displacement. Controversy exists regarding the significance of a central watershed area of decreased vascularization, first reported by Waugh in 1958 while evaluating Kohler disease. McKeon suggested that factors other than vascularity contribute to stress fractures, as only 6 of 54 specimens in his cadaveric study had the classic pattern of previously described avascularity.
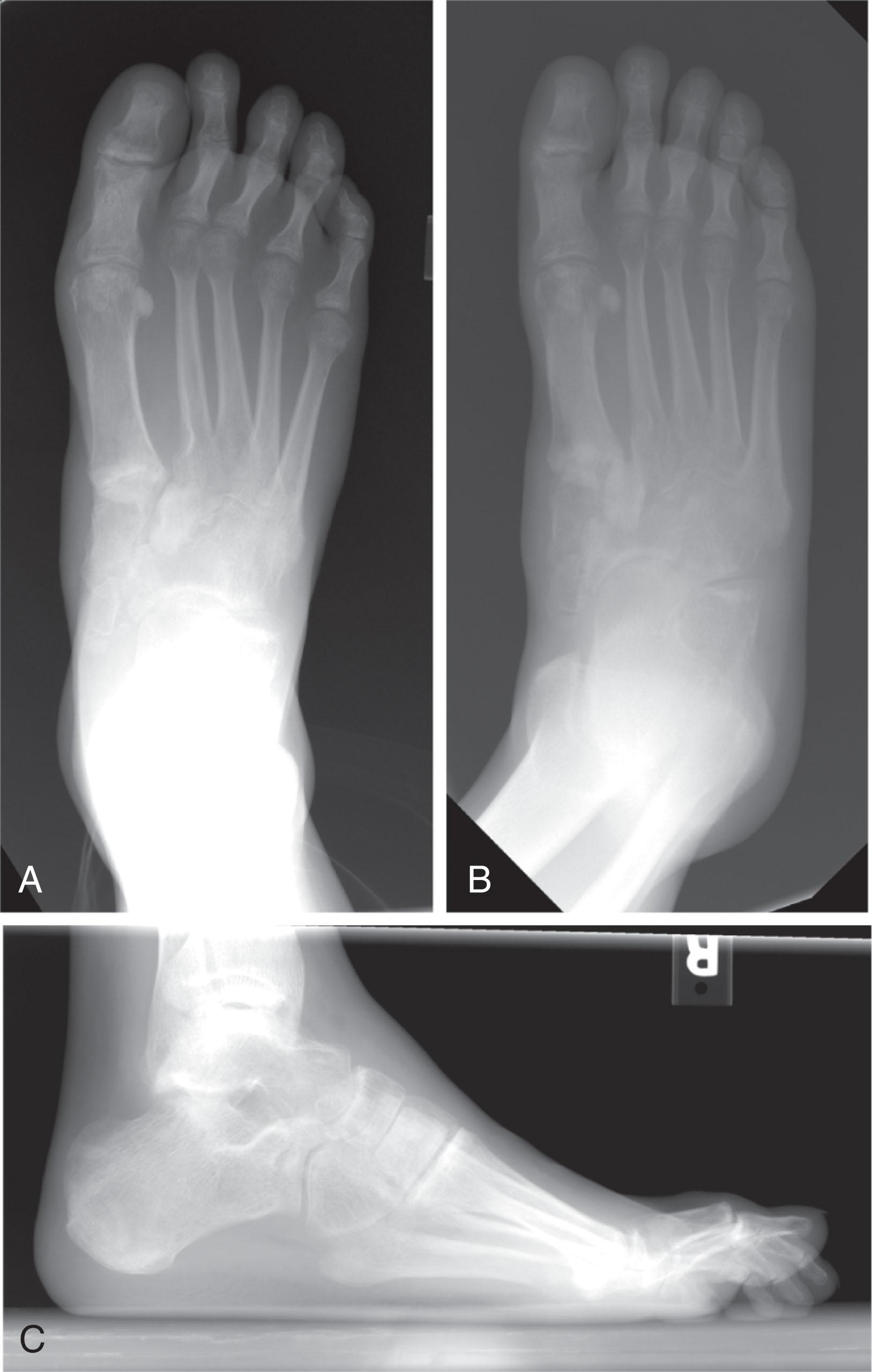
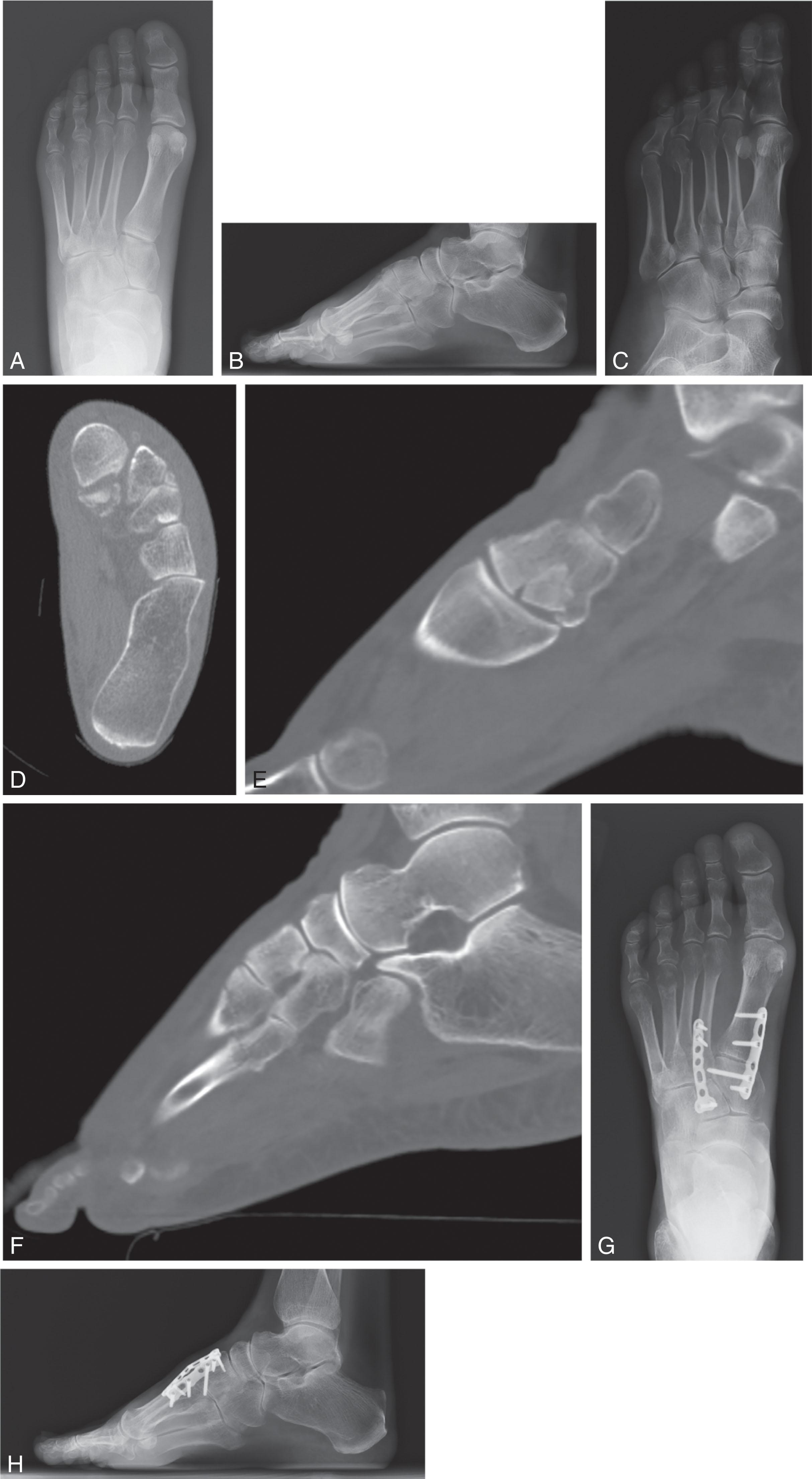
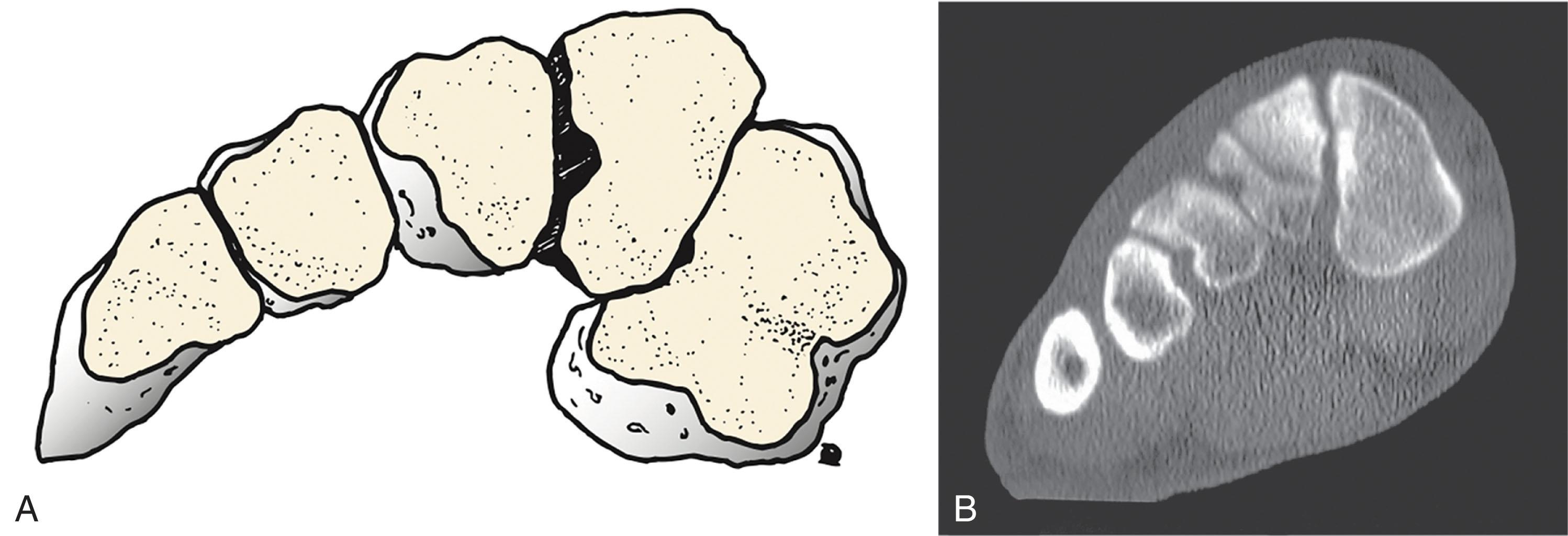
Initial evaluation of the patient with a suspected navicular stress fracture should include weight-bearing anteroposterior (AP), lateral, and lateral column oblique radiographs. A coned-down AP view of the navicular may also be helpful because greater penetration of the beam may lead to higher sensitivity of plain radiographs. It can be very difficult to differentiate between a bipartite navicular and a navicular stress fracture. A bipartite navicular is comma shaped and bent, with a cleft from proximal plantar to distal dorsal, which creates a triangular wedge of bone dorsal to the navicular body ( Fig. 47-9 ). In contrast, a stress fracture occurs in the sagittal plane and most commonly in the central third of the bone (see Fig. 47-10 ).

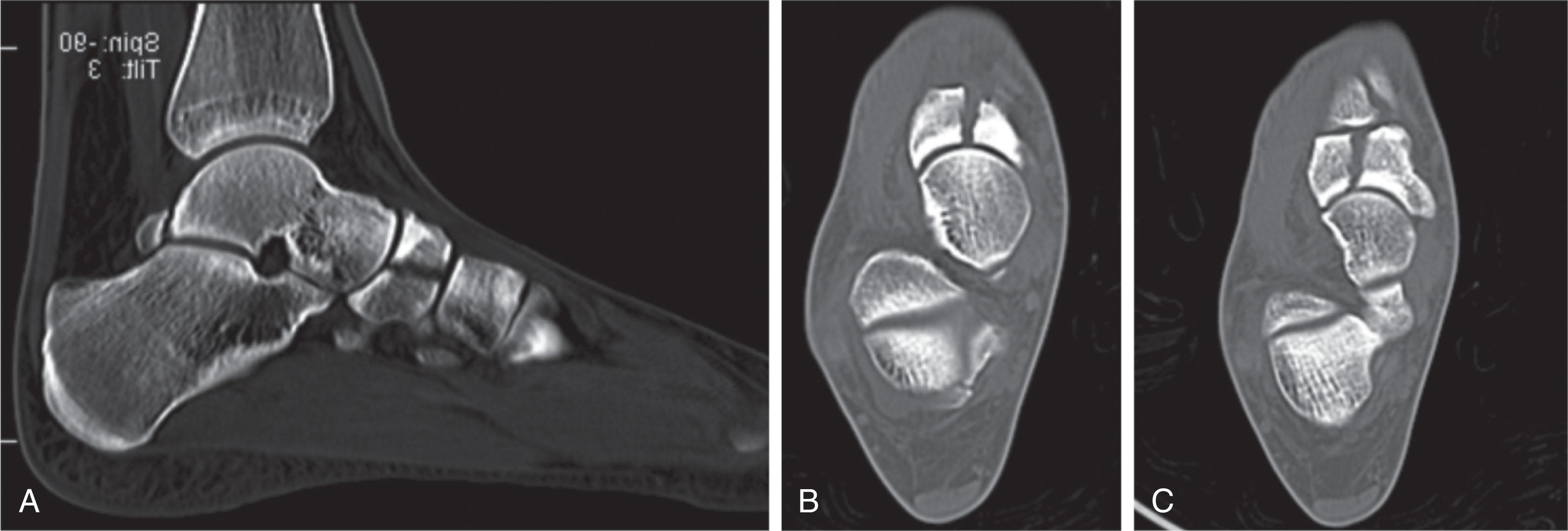
Bone scans are very sensitive for detecting stress fractures but are not as commonly used as CT scans or MRIs. CT scans are more accurate in evaluating fracture lines, displacement, coalitions, and cystic changes, but MRI is more sensitive in earlier diagnosis and treatment of stress reactions. If plain radiographs, MRI, and CT are negative, a bone scan can confirm a diagnosis if suspicion remains. Complete fractures are most commonly in the sagittal plane in the central third of the navicular body while incomplete fractures most commonly involve the dorsal cortex of the proximal articular surface ( Fig. 47-11 ).

The literature on navicular stress fractures is limited to small series. McCormick et al reported that in 10 surgically treated fatigue fractures at 3-year follow-up, eight had gone onto radiographic union confirmed by CT scan. They reported that completely displaced navicular stress fractures have a higher incidence of nonunion. Many other authors have recognized the importance of preventing displacement of a navicular stress fracture. Hunter, Torg et al, and Khan et al recommended removing patients from athletic activities and to maintain the fracture nondisplaced, strict non–weight bearing in a cast for 6 to 8 weeks. Torg et al performed a meta-analysis to establish an evidence-based treatment algorithm. Their results favored non–weight-bearing casting or surgery over weight-bearing casting ( P < 0.0003). They reported no statistical difference between non–weight-bearing casts and surgical management and recommended conservative treatment with non–weight-bearing casting as the standard of care for nondisplaced navicular stress fractures. Most authors agree that in nonathletes a trial of strict non–weight bearing and immobilization is warranted. In athletes, and certainly in patients with displaced fractures, operative reduction and internal fixation is generally recommended.
When surgery is performed, a dorsal approach to the navicular is popular with open reduction and lag screw placement from the smaller lateral fragment to the larger medial fragment. Some authors recommend percutaneous screw placement from medial to lateral to avoid further vascular disruption. Internal fixation is commonly performed with 4.0 mm partially threaded cannulated screws. In fractures with diastasis, autologous graft or aspirate may be added. The patient is then kept non–weight bearing for 6 to 8 weeks and often casted followed by progression in a weight-bearing boot and then transition into a graphite plate insole around 3 months postoperatively. Athletes generally initiate return to sports activity at least 4 to 6 months postoperatively, depending on documentation of healing best seen on CT scan obtained at least 3 months after surgery.
The primary complication is delayed union or nonunion in both conservatively and operatively treated patients. Patients who have progression to nonunion will remain symptomatic with pain. Radiographs may demonstrate diastasis or medullary cysts. An untreated nonunion can lead to further displacement and deformity, similar to a comminuted navicular body fracture, with a progressive flatfoot deformity and medial column collapse. Nonunions are primarily treated with Open Reduction Interal Fixation (ORIF) and bone grafting, and vascularized pedicle bone grafting has been reported with success. If arthritic changes exist, adjacent joint fusion is most predictable.
High-energy force is required to produce this rare injury and it probably represents a variant of the midtarsal dislocation with ligamentous injuries extending to the adjacent tarsal joints. The mechanism consists initially of foot plantar flexion causing plantar dislocation of the naviculocuneiform joint, followed by recoil of the foot against the plantar surface of the navicular, causing dorsal extrusion. Only a few have been reported and all were complicated by either AVN or planovalgus collapse.
Fractures that are isolated to the cuboid are generally uncommon as they are generally a component of more complex injury. This is due to the protected anatomic position and buttressed location of the cuboid as well as its robust pyramidal shape with the base medially and the apex laterally. The cuboid has six distinct surfaces, three of which articulate with surrounding bones. Dorsally and laterally the cuboid is exposed, while plantarly the long plantar ligaments attach at the peroneal sulcus that runs obliquely distally and medially with the peroneus longus tendon. Distally, the fourth and fifth metatarsal facets make the largest contribution to dorsiflexion and plantarflexion of the midfoot and also contribute to pronation and supination. The proximal surface facet articulation with the calcaneus further contributes to pronation and supination, and the medial surface articulates with the lateral cuneiform and occasionally navicular. The bony architecture of the cuboid provides an essential contribution to overall static and dynamic foot function. Consequently, loss of lateral column length results in forefoot abduction with planus and compensatory eversion of the hindfoot. The predominant fracture types seen in cuboid fractures are avulsion and compression fractures to the body or direct crush injury, which can be highly variable. Insufficiency fractures comprise a less common fracture category. Fenton et al, in the largest series to date, attempted to further classify traumatic cuboid fractures into five categories ( Table 47-2 ; Fig. 47-12 )
| Type | Description |
|---|---|
| I | Avulsions–bifurcate ligament avulsions occur with forefoot adduction and inversion of the hindfoot. |
| II | Extraarticular fractures–mildly displaced body fractures that do not extend into the calcaneocuboid or tarsometatarsal joints, these occur with axial load to the fourth and fifth metatarsals or abduction of the forefoot. |
| III | Intraarticular fractures–mildly displaced body fractures that extend into the calcaneocuboid or tarsometatarsal joints, these occur with axial load (see Fig. 47-12 ). |
| IV | Associated tarsometatarsal injury–dislocation of the fourth and fifth metatarsals may cause shearing and shortening of the articular surface distally; these result from indirect rotational injury or direct crush injury. |
| V | Associated crush or midtarsal injury–seen with lateral column injury and possible multifragmentary shortening from cuboid compression during forceful eversion of the forefoot on the hindfoot. |

The most common cuboid fracture is a lateral avulsion of the calcaneocuboid ligament, which is best detected on AP or oblique foot radiographs. These fractures are often misdiagnosed as a simple ankle “ sprain” as they may be associated with twisting or inversion. Ecchymosis and swelling are variable, but careful examination for the location of tenderness on the lateral foot can help distinguish cuboid fracture from lateral ankle sprain ( Fig. 47-13 ).
The majority of avulsion fractures can be treated nonoperatively because they are minimally displaced. Multiple authors have recommended boot immobilization for up to 6 weeks.
With larger fragments, varus stress radiographs revealing a calcaneocuboid angle greater than 10 degrees may also be indication for operative intervention. However, surgery is often reserved for the patient with a painful nonunion of an avulsion fragment that has been adequately treated with immobilization and footwear modifications. Surgical excision and soft tissue repair typically relieves pain resulting from a symptomatic nonunion.
The second most common cuboid fracture pattern is a compression fracture. This high-energy fracture pattern, seen in automobile accidents or high falls, is commonly caused by axial loading a plantar-flexed foot, with either inversion or eversion of the forefoot. It has been described as a “nutcracker fracture of the cuboid” between the calcaneus and the abducting lateral metatarsals, which compress the cuboid.
In the series of 155 patients with midfoot fractures, published by Richter et al, 58 patients had fractures of the cuboid. Seventy-six percent had cuboid fractures associated with Lisfranc or Chopart injuries, whereas only 14 (24%) patients had isolated cuboid fractures. These authors found that isolated cuboid fractures had better long-term functional outcomes.
Patients should also be stressed with a passive abduction, adduction, inversion, or eversion maneuver and evaluated for associated injuries of the Chopart or Lisfranc joints. Any patient with a high-energy mechanism of injury that results in a cuboid fracture should have a complete radiographic series of the entire foot, and likely a CT scan should be performed.
Patients with minimally displaced extraarticular and intraarticular fractures can be treated with immobilization and activity restrictions as long as lateral column length integrity and articular congruence is maintained. Cast immobilization may be best, followed by a walking boot with progression as tolerated.
The amount of displacement that necessitates operative treatment of cuboid fractures is controversial although it is widely accepted that the cuboid serves as an important stabilizer of the lateral column, and a failure to restore length will result in pain and deformity. Surgical interventions should focus on restoration of length, rotation, and alignment.
Weber and Locher presented a series of 12 patients with compression fractures of the cuboid that were treated with open reduction and internal fixation without arthrodesis. Four patients required screw fixation only, whereas eight patients required a plate-and-screw construct to reconstruct the cuboid. Seven patients (58%) in their series required bone grafting to restore length. Sangeorzan and Swiontkowski also noted the frequent need for bone grafting. They recommended distraction, maintained with bone grafting, along with internal fixation. In severely comminuted fractures, fusion constructs or spanning bridge-plate fixation may be the only options to restore and maintain column length. In fractures with a severe soft tissue injury, spanning external fixation can be used with the focus on maintaining lateral column length regardless of timing and type of definitive fixation technique.
Stress fractures usually present with an insidious onset of pain on the lateral side of the foot exacerbated by activity. Advanced imaging is frequently necessary to diagnosis these injuries. Beaman et al reported two cases of tarsal cuboid stress fracture in collegiate athletes that mimicked peroneal tendon disorders and both patients were able to return to their prior level of activity after a period of rest and immobilization. Cuboid insufficiency fractures have also been associated with plantar fascia disruption. Yu and Solmen reported on two such patients. The first patient had a prior surgical release of the plantar fascia and healed the cuboid fracture conservatively, while the second patient had a spontaneous plantar fascia rupture before the stress fracture and eventually necessitated a calcaneocuboid arthrodesis.
Patients can generally be conservatively treated with immobilization and activity restriction up to 6 weeks. If they are unable to bear weight because of pain, a short-leg cast and complete non–weight bearing may be preferred.
Rarely, for those patients with persistent pain despite aggressive conservative treatment for at least 12 weeks, compression screw placement with an option for bone grafting can be considered. Salvage arthrodesis of the calcaneocuboid joint can be performed as a last resort.
Fractures isolated to the cuneiform bones are rare and there are two types, avulsion fractures and crush injuries resulting from direct trauma.
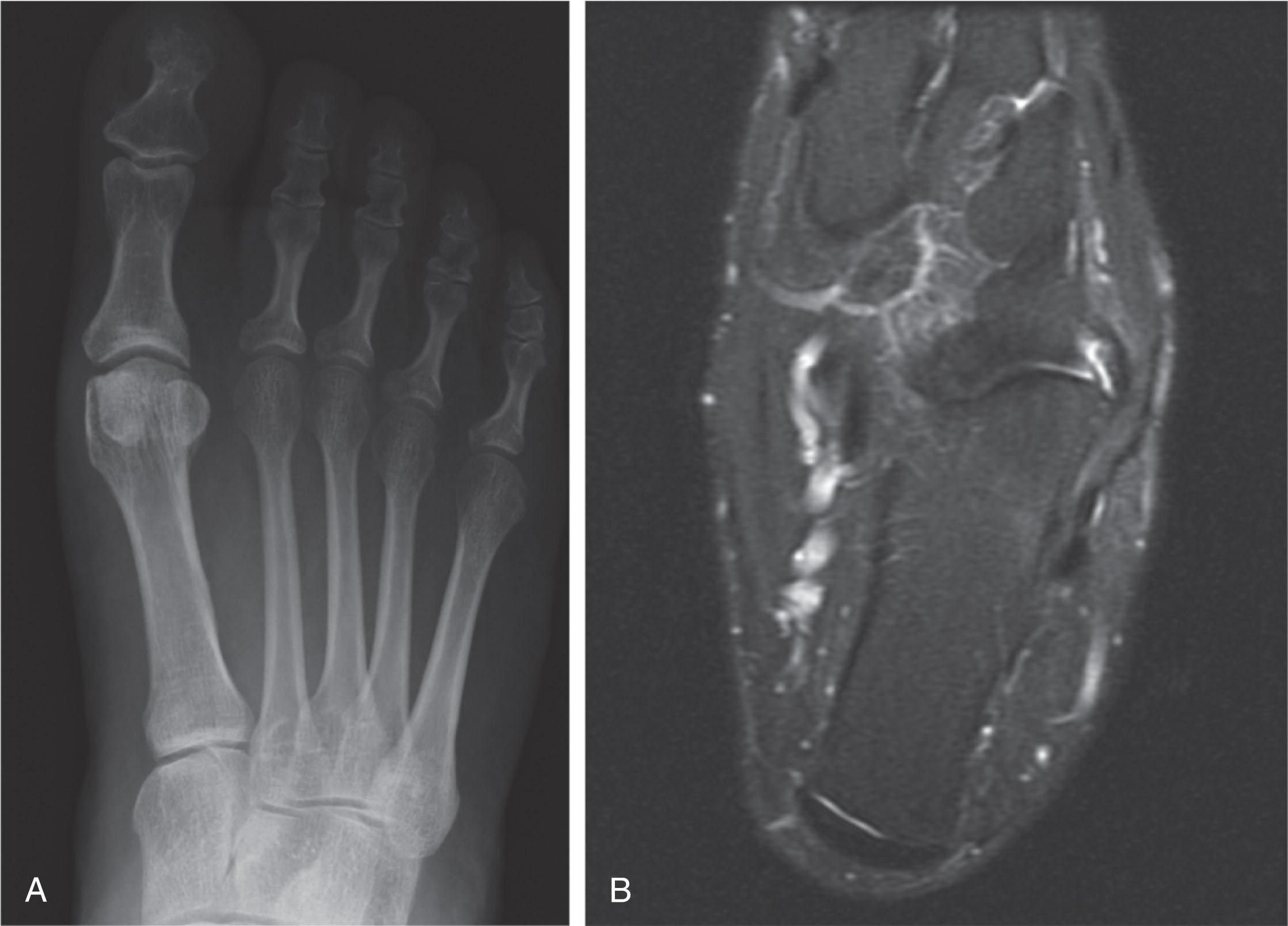
Usually minimally displaced because of the intertarsal ligaments, these fractures are caused by a twisting mechanism. Patients will present with variable swelling, ecchymosis, and tenderness in the midfoot, and weight-bearing radiographs may be important to rule out concomitant injuries. The irregular edges of an acute fracture differentiate it from the smooth surface edges of a bipartite cuneiform.
Patients can generally be conservatively treated with a walking boot and activity restriction until they can weight bear without pain.
Surgery can be considered when there is significant displacement of the avulsion fracture or if the patient fails conservative treatment. Small fractures can be excised while larger fragments may necessitate bone grafting and internal fixation followed by a period of non–weight bearing. Functional limitations are rare in these fractures because there is not a significant amount of native motion at the cuneiform joints ( Fig. 47-14 ).
Direct blow to the midfoot is the most common mechanism for isolated fractures to the cuneiform. These fractures are usually higher energy than avulsion fractures. Careful review of a complete radiographic series must be performed to exclude concomitant injuries. A CT scan can characterize the amount of fracture displacement, intraarticular extension, and any associated dislocations.
If the fracture is minimally displaced, patients can be immobilized in a boot with pain serving as the guide for progression into standard footwear.
Patients with large fragments displaced, subluxated, or intraarticular step-off should be considered operative with open reduction and internal fixation. For severe crush injuries with fragments too small for screw fixation, a temporary bridge plate may be used to maintain length while the fracture heals ( Fig. 47-15 ). Intercuneiform arthrodesis can be considered based on degree of articular injury ( Fig. 47-16 ).


Isolated dislocation of the midfoot bones is uncommon and usually involves the more mobile medial column at the navicular. Most of these so-called “isolated” injuries likely occur in association with radiographically undetectable ligamentous injuries. High-energy trauma is generally the cause of cuneiform or cuboid dislocations. Staged management may be best if the soft tissues are not amenable to initial definitive treatment as evidenced by fracture blisters and loss of skin wrinkles.
Cuneiform dislocation occurs most often with a Lisfranc fracture-dislocation, but isolated cuneiform dislocations have also been reported. The cuneiforms most easily dislocate dorsally with “indirect” plantar-flexion and axial loading forces. The medial cuneiform follows the path of least resistance, dislocating dorsally or medially. The first metatarsal may follow with the entire medial column dislocated proximally and dorsally associated with disruption of the intercuneiform and naviculocuneiform ligamentous attachments. Isolated dislocations of the middle cuneiform have also been reported associated with pure plantar-flexion injuries at the second ray. The Roman arch bony configuration of the midfoot and the strong plantar ligaments impart strong resistance to plantar dislocation. However, a high-energy direct blow to the dorsal foot may cause plantar dislocation, which is likely to be associated with compartment syndrome or open injuries. Clinical evaluation may reveal midfoot ecchymosis with tenderness and deformity can sometimes be detected depending on the degree of swelling. Prompt diagnosis is essential to prevent collapse of the midfoot, AVN, or arthritis. Radiographically, the tarsometatarsal alignment should be examined carefully and the complex radiographic anatomy of the midfoot may warrant a CT scan as a diagnostic aid.
At presentation, closed reduction may reduce deformity and relieve skin tension. With some cuneiform dislocations, applying pressure over the prominent dislocated bone while longitudinal traction is applied through finger traps may be beneficial. When the medial cuneiform is dislocated dorsally, the lateral slip of the anterior tibialis may block reduction and open reduction may be necessary ( Fig. 47-17 ). Open reduction is most commonly performed through a dorsal longitudinal incision with restoration of tarsal alignment followed internal fixation. Screws or plates placed across relatively immobile joints, such as the intercuneiform and naviculocuneiform articulations, are often left permanently. Primary fusion can be performed for severely damage joint surfaces ( Fig. 47-18 ).
The rigid framework of the lateral column of the foot and the multiple ligamentous attachments of the cuboid bone across its articulation with the calcaneus, lateral cuneiform, fourth and fifth metatarsals, and occasionally the navicular render isolated cuboid dislocation highly unusual. Reports indicate that the cuboid displaces plantarmedial, and various mechanisms have been proposed including crush injury, opposite rotational moments about the hindfoot and forefoot, and abduction and dorsiflexion of the forefoot expelling the cuboid.
Clinically, the patient may have pain or a defect based laterally accompanied by ecchymosis and swelling. Careful radiographic evaluation demonstrates medial and plantar displacement of the cuboid with loss of the normal anatomic relationships. Coexistent rotatory subluxation of the talonavicular joint with temporary subtalar subluxation may be associated, and osteochondral fractures of the surrounding bones and the subtalar complex may coexist.
Although closed reduction may be obtained by supination and adduction of the forefoot with dorsally directed pressure over the plantar cuboid, finger traps can also help, but the reduction may be impeded by the peroneus longus. It may be necessary to expose and stabilize the cuboid with multiple Kirschner wires via a dorsolateral approach. Immobilization non–weight bearing for 6 to 8 weeks, followed by removal of hardware, may provide a functional foot. Delayed reconstruction of ligamentous stabilizers or fusion may be necessary for chronically painful symptoms.
Lisfranc was a Napoleonic-era field surgeon credited with describing amputations through the tarsometatarsal joints. Lisfranc joint injuries, as defined today, represent an extremely heterogeneous group of injuries about the midfoot-forefoot junction. This includes high-energy injuries with severe dislocations and significant soft tissue injury, as well as subtle sprains with millimeter subluxations easily evading detection. Increased awareness of the potential for long-term disability resulting from subtle injuries has heightened the index of suspicion in identifying these injuries.
In 1909, Quenu and Kuss provided the original descriptive treatment algorithm forming the foundation for current classifications. Gissane's report, in 1951, described three forefoot amputations resulting from vascular compromise associated with delayed joint reduction. In the 1950s, Del Sel and then Collett et al introduced the importance of anatomic reduction in maximizing functional outcome. This concept was not universally accepted, and restoration of joint congruity was not considered a necessary standard, as late salvage by arthrodesis was reportedly successfully performed in those presumed few patients with a poor functional result. The importance of anatomic reduction was again emphasized by multiple studies in the 1970s and 1980s, which demonstrated that prognosis depended greatly on achieving and maintaining an anatomic reduction. These early reports included closed reduction with splinting, percutaneous Kirschner wire fixation, open Kirschner wire fixation, and open treatment with screws.
The Lisfranc joint complex includes the tarsometatarsal joints, intermetatarsal joints, and anterior intertarsal articulations. It is an elaborate biomechanical construct stabilized by its unique bone structure, strong capsuloligamentous attachments, and plantar soft tissue restraints. Sagittal motion is characterized as 10 to 20 degrees at the fifth tarsometatarsal joint, with progressively less mobility from lateral to medial rays, with the exception of substantial sagittal and coronal plane motion at the first tarsometatarsal articulation.
The first through the third metatarsal bases and their corresponding cuneiforms are dorsally based trapezoids in coronal cross section. The result is a Roman arch configuration that imparts inherent osseous stability to the convex-dorsal transverse arch by preventing plantar displacement of the metatarsal bases. In the axial plane, the second metatarsal base is recessed and dovetailed between the medial and lateral cuneiforms, limiting frontal plane translation ( Fig. 47-19 ). The recessed position of the second metatarsal at the apex of the Roman arch make this particular articulation the keystone of the Lisfranc complex, thus explaining the rarity of injury without second metatarsal base fracture and the reason a shallower mortise places patients at greater risk for injury.
The tarsometatarsal joints are formed by the proximal articular surface of the five metatarsals and the distal articular surface of the corresponding three cuneiforms and cuboid. The first, second, and third tarsometatarsal joints are characterized by a slightly concave metatarsal articular surface correspondingly to a convex surface of the respective cuneiform, and the first tarsometatarsal joint is slightly medially oriented. The fourth metatarsal has a flatter surface that articulates with the medial cuboid facet, and occasionally it also articulates with the lateral cuneiform. The fifth metatarsal articulates with the lateral facet of the cuboid, which is separated from the medial cuboid facet by a vertical crest, and more laterally oriented.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here