Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
“Many handis make light warke ” John Heywood (1497–1580)
Hand surgery is always teamwork between the surgeon, the patient, and the therapist. One cannot get a successful outcome without the cooperation of the other two.
Interestingly there are exceedingly few randomized controlled trials in the management of hand fractures despite this being a common injury. Hand fractures are often considered to be a soft tissue injury with an underlying bone injury.
This chapter deals with the diagnosis and management of fractures of the phalanges and metacarpal bones in adults and children. The majority of these digit injuries can be treated effectively with conservative management and early therapy intervention. This chapter identifies the injuries that may need surgical intervention and the options available.
The differences between pediatric and adult hand fractures lie in the elasticity of children’s bones and the potential disruption of their growth.
Children’s bones have increased water content and plasticity, and tend to fracture incompletely with trauma. Incomplete fractures are seen as bows (bending forces), buckle fractures (one cortex buckles with compression), or green-stick fractures (one cortex ruptures under tension, the other is intact or buckles). The plastic deformation may prevent complete reduction of the fracture when manipulated, but most fractures still do not require open operations, but can be managed with closed or percutaneous techniques, due to the remodeling potential.
The assessment of the fracture is clinical and radiological. The child will have point tenderness in the nondisplaced fracture over the physis, which should increase suspicion of a fracture. If plain X-rays in two, if not three planes, cannot explain pain or deformation, MRI or CT will. The tenodesis test adequately demonstrates any rotational deformity, as the fingers should all be pointing towards the scaphoid tubercle. If in doubt, compare with the other hand. Angular deformities in children may remodel, rotational will not and needs to be corrected.
Any fracture interfering with the growth-plate has a potential for disrupting normal growth. Pediatric fractures involving growth plates are classified according to Salter and Harris. Ogden expanded the classification in 1984 ( Table 56.1 ). ,
| Classification | Clinical | Configuration | Management | Complication |
|---|---|---|---|---|
| I: through physis, showing increased width of physis | Point tenderness only |  |
Conservative | Possible shortening |
| II: through physis and metaphysis | Occurs >10 years old |  |
Manipulation under anesthetic if displaced | Minimal shortening |
| III: through physis and epiphysis | >10 years old |  |
Accurate surgical reposition | Can result in chronic disability as extending into joint |
| IV: metaphysis, physis and epiphysis | Any age, rare in hand |  |
If displaced consider ORIF | Intraarticular so can result in chronic disability and can cause premature focal fusion of the joint |
| V: compression of the epiphyseal plate | Usually from axial loading |  |
Conservative | Growth disturbances |
| VI: open fracture in which part of the physis is missing | Open fracture |  |
Initial fat grafting to prevent physeal bar, later reconstruction with bone graft | Growth disturbances |
| VII: epiphyseal plate only |  |
Requires accurate re-positioning as intraarticular fracture | No impact on growth | |
| VIII: Isolated injury to the metaphysis |  |
Usually can be manipulated under anesthetic or if necessary fixed with K-wire | Potential injury related to endochondral ossification | |
| IX: Injury to the periosteum |  |
May interfere with membranous growth |
The most common fracture pattern encountered in the fingers is a Salter–Harris II, which is satisfyingly corrected with a simple maneuver with a pen, over which the finger is manipulated ( Fig. 56.1 ).
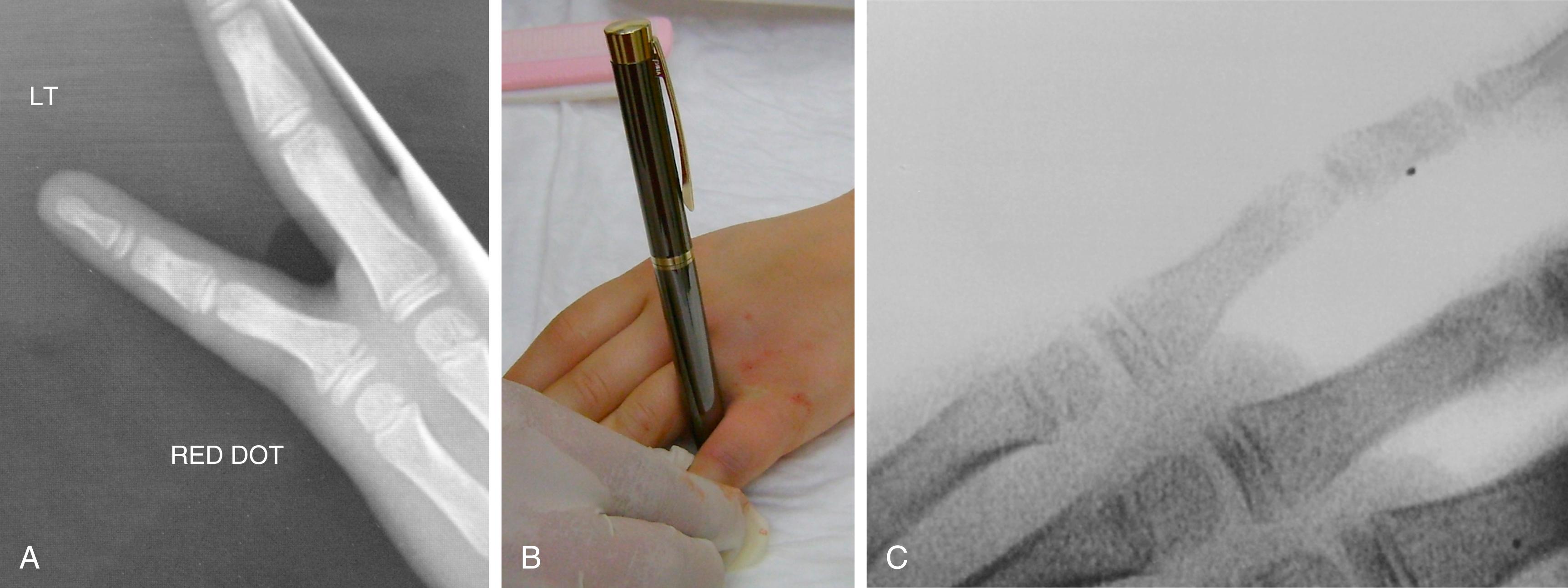
Crush distal phalanx fractures and nailbed injuries are the most common pediatric fracture. These occasionally need a Kirschner-wire (K-wire) or an orange needle to pin a larger distal fragment in place, but often the fragment is too small. A special type of nailbed injury is the Seymour fractures, which are displaced distal phalanx Salter I or II fractures, with avulsion of the proximal edge of the nail from the eponychial fold and the germinal matrix often interposed in the fracture itself ( Fig. 56.2 ). Accurate and timely debridement and repositioning of all tissues is therefore paramount to allow adequate growth of both digit and nail. The clinical presentation can be confused with a mallet finger (because the extensor tendon inserts itself in the epiphysis whilst the flexor tendon inserts itself in the metaphysis), but a true lateral X-ray and a thorough examination under anesthetic should reveal the injury.

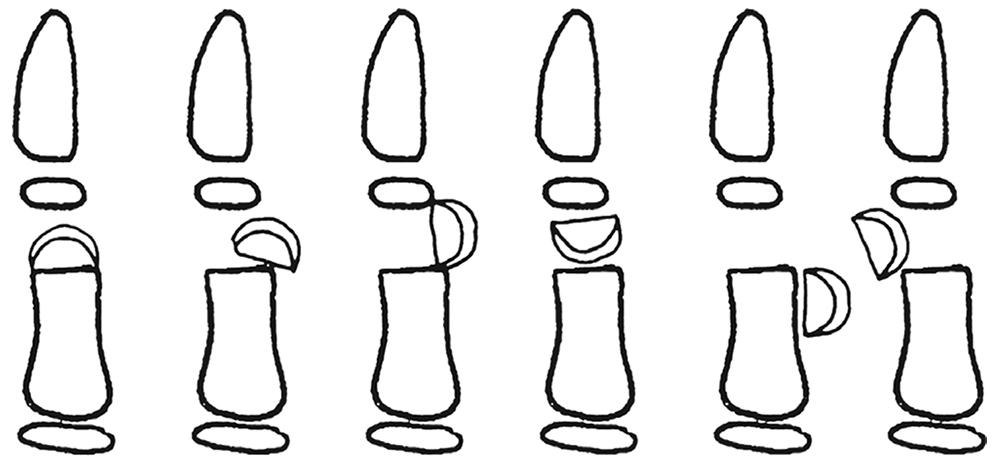
Fractures through the neck of the phalanges are usually only found in children and mostly involve some unfortunate interface between fingers and doors. Al-Qattan divided them into three categories, which determined prognosis and treatment: type I fractures are undisplaced, type II fractures are displaced, but maintain some bone-to-bone contact, whilst type III fractures have no bone-to-bone contact. Type III is furthermore subdivided according to the location of the distal fragment, type IIID especially being associated with an avascular fingertip ( Fig. 56.3 ). Since the smallest displacement is poorly tolerated, all types apart from type I require open reduction and K-wiring, but have progressively worse prognoses.
Hand therapy intervention for these patients is minimum as younger children rarely become stiff at the DIP joint and instinctively start functional use once the bulky bandage or splint has been removed. Older children may require a volar splint of the affected digit until pain has settled alongside edema control work.
It is worth remembering that there is no gain in changing the dressings in nailbed injuries before 10 days, unless you are worried about infections, which of course is a different matter.
Hand fractures account for ∼17% of all fractures in adults, with 59% of hand fractures occurring in the phalanges, 33% in the metacarpals, and 8% in the carpal bones.
It is the authors’ practice always to speak to patients about bone grafts and obtain consent for this option before the operation, even though it is rarely needed.
Metacarpal fractures can be divided into their anatomical location or configuration, but most commonly occur in the little or ring fingers and the thumb.
Neck fractures of the fourth and fifth metacarpal are usually treated conservatively and many surgeons now state they will never treat these surgically, whatever the angulation of the fracture is. They can be manipulated and the digit neighbor-strapped, accepting that the patient will lose the knuckle and may have some extensor lag. If there is rotation of the digit this should be corrected surgically.
Neck fractures where the head is completely off the metacarpal and involves the index or little fingers may be fixed with minicondylar plates. In other fingers, H-plates or T-plates (the two-hole fixation on each side of the fracture can be transverse remember) can be used or perhaps even better, intramedullary K-wiring.
Intraarticular metacarpal head fractures are best seen on Brewerton’s views and can be fixed with countersunk screws, if the fragments are large enough. The fragment must be three times the size of the screw head to hold it. If this is not possible a primary joint replacement or a free joint from the second toe may be considered at a later date if function is compromised. Very rarely does this joint get considered for fusion in the fingers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here