Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Gastrointestinal foreign bodies (GIFBs) are composed of food bolus impactions and intentionally and unintentionally ingested or inserted foreign objects. Bezoars are ingested materials (food or other materials) that accumulate in a normal or abnormal stomach. Caustic ingestions present following ingestion of acid or alkaline materials, which may result in acute and/or chronic injury to the esophagus and stomach. These topics are discussed in detail in this chapter.
GIFBs are a common problem encountered by gastroenterologists. Most resolve without serious clinical sequelae. Older studies have suggested that between 1500 and 2750 deaths occurred in the US secondary to GIFBs. More recent studies have suggested the mortality from GIFBs to be significantly lower, with no deaths reported in over 850 adults and only one death in some 2200 children with reported GIFBs. Regardless of imprecise morbidity and mortality rates, serious complications and deaths result from foreign body ingestions. Because of their frequent occurrence and potential for negative consequences, it is important to understand which patients are at risk and know how to diagnose and treat GIFBs and deal with their complications.
GIFBs may result from unintentional or intentional ingestion. The most common patient group that unintentionally ingests foreign bodies is children, particularly those between ages 6 months and 3 years. Children account for 80% of true foreign body ingestions. Children’s natural oral curiosity leads to placing objects in their mouth and occasionally swallowing them. Coins are the most common objects swallowed by children, but other frequently swallowed objects include marbles, small toys, crayons, nails, and pins.
Accidental ingestion due to loss of tactile sensation during swallowing may also occur in adults with dental covers or dentures ; mistakenly ingesting one’s own dentures is not uncommon. Patients with altered mental status or sensorium, including the very old, demented, or intoxicated, are at risk for accidental foreign body ingestions ( Fig. 28.1 ). Accidental coin ingestion has been noted in college-aged adults during a tavern beer drinking game called “Quarters,” in which the coin becomes lodged in the esophagus. Finally, those in certain occupations (e.g., roofers, carpenters, seamstresses, tailors) are at risk of accidental ingestion when nails or pins are held in the mouth during work.

The most common groups that intentionally ingest foreign bodies are psychiatric patients and prisoners, in whom ingestion is often done for secondary gain; they often ingest multiple objects multiple times and often the most complex foreign bodies.
Iatrogenic foreign bodies are increasing in prevalence because of complications from capsule endoscopy, migrated stents (esophageal, enteral, and biliary), and migrated enteral access tubes and bolsters.
Esophageal food impaction is the most common GIFB requiring medical attention in the US, with an incidence of 16/100,000. The vast majority (75% to 100%) of patients with an esophageal food impaction have an underlying predisposing esophageal pathology, most often peptic strictures, Schatzki rings, and increasingly eosinophilic esophagitis (EoE). Esophageal cancer rarely presents with acute food bolus impaction. Other causes that contribute to esophageal food impactions include altered surgical anatomy following esophagectomy, fundoplication, or bariatric surgery and motility disorders such as achalasia and distal esophageal spasm.
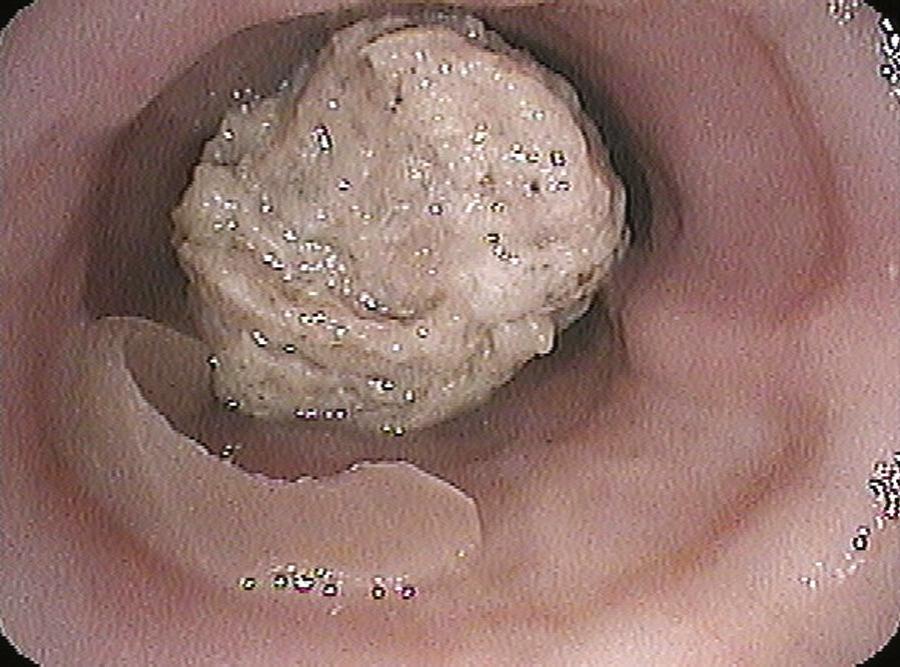
Food impactions most commonly occur in adults in their fourth or fifth decade of life but are becoming more prevalent in young adults because of the rising incidence of eosinophilic esophagitis. Cultural and regional dietary habits influence GIFBs. Fish bone injury is common in Asian countries and the Pacific rim, whereas impactions due to meats (e.g., hot dogs, pork, beef, chicken) are common in the US ( Fig. 28.2 ).
Symptomatic rectal foreign bodies are more often the result of insertion through the anus rather than oral ingestion and transit. This is reported most commonly in young adult males. Rectal foreign bodies that come to medical attention are most commonly inserted with the intention of autoeroticism but may present following consensual sexual acts or sexual assault. Less common but still prevalent causes of rectal foreign bodies include concealment of illegal drugs during smuggling efforts, loss of objects during attempts by the patient to relieve constipation, and even reports of falling on objects.
The majority (≈ 80% to 90%) of GIFBs pass through the GI tract without any clinical sequelae and cause no harm to the patient. The remaining 10% to 20% of GIFBs will require endoscopic intervention, and 1% of GIFBs may require operative therapy. Recent data suggest that in the setting of intentional ingestions, the need for endoscopic and surgical intervention is higher with endoscopy being performed in two thirds of cases and surgery needed in greater than 10% of patients. True foreign bodies and food impactions can cause significant morbidity, with the most serious complications being bowel perforation or obstruction and rarely ensuing death. To help stratify therapeutic interventions, it is important to understand the conditions, patients, and anatomic locations in which complications associated with GIFBs are apt to occur.
Perforation and obstruction from GIFBs can occur in any part of the digestive tract, but they are more apt to occur in areas of narrowing, angulation, anatomic sphincters, or previous surgery ( Fig. 28.3 ). The pharynx is the first area where foreign bodies may become entrapped and cause complications. In the hypopharynx, short sharp objects like fish bones and toothpicks may lacerate the mucosa or become lodged.

Once in the esophagus, there are 4 areas of narrowing where food boluses and foreign bodies become lodged: upper esophageal sphincter, level of the aortic arch, level of the mainstem bronchus, and esophagogastric junction. These areas all have luminal narrowing to 23 mm or less. However, food and foreign bodies more commonly lodge in the esophagus at areas of pathology, including rings, webs, or strictures. Multiple esophageal rings associated with eosinophilic esophagitis (see Chapter 30 ) contribute to esophageal food impaction at an increasing prevalence in young adults. Similarly, esophageal motor abnormalities (see Chapter 44 ) such as distal esophageal spasm or achalasia may lead to food or foreign body impaction in the esophagus. Foreign body and food impaction in the esophagus have the highest incidence of overall adverse events, with the complication rate directly proportional to how long the object is lodged in the esophagus. Esophageal foreign bodies in children have a significantly lower spontaneous passage rate, as low as 12% compared with other GIFBs. Serious complications of esophageal foreign bodies include perforation, abscess, mediastinitis, pneumothorax, fistula formation, and cardiac tamponade.
If a GIFB passes through the esophagus, the vast majority will pass through the entire GI tract without further difficulty or complication. Exceptions are sharp, long, and large objects. Sharp or pointed objects may have a perforation rate as high as 35%. Large objects (>2.5 cm [1 inch] in diameter) may not be able to pass through the pylorus. Long objects (>5 cm [2 inches]) such as pens, pencils, and eating utensils may not negotiate around the duodenal sweep or through the pylorus.
Objects may become impacted in the small intestine at the ligament of Treitz or ileocecal valve. Adhesions, postinflammatory strictures, and surgical anastomoses within the small intestine may also be sites where foreign bodies lodge and obstruct. However, most objects, even sharp ones, rarely cause damage once in the small intestine and colon, because the bowel naturally protects itself through peristalsis and axial flow. These factors tend to keep the foreign body concentrated in the center of fecal residue, with the blunt end leading and the sharp end trailing.
Inserted rectal objects are often tenaciously retained because of anal sphincter spasm and edema, making spontaneous passage of the object difficult. The angulation and valves of Houston may also impede passage of objects through the rectum.
The history from children or noncommunicative adults is often unreliable. Most gastric and up to 20% to 30% of esophageal foreign bodies in children are asymptomatic. Most of these present after having been witnessed or suspected by a parent, caregiver, or older sibling, but in up to 40% of cases, there is no history of a witnessed ingestion. Thus, symptoms are often subtle in children, presenting as drooling, not wanting to eat, and failure to thrive.
For communicative adults, history of the timing and type of ingestion is usually reliable. Patients are able to relate exactly what they ingested, when they ingested it, and symptoms of pain and/or obstruction. Patients with esophageal food bolus impactions are symptomatic with complete or intermittent obstruction. They are unable to drink liquids or retain their own oral secretions. Sialorrhea is common. Ingestion of an unappreciated small, sharp object, including obscured fish or animal bones, may cause odynophagia or a persistent foreign body sensation because of mucosal laceration. The type of symptoms can aid in determining whether an esophageal foreign object is still present. If the patient presents with dysphagia, odynophagia, or dysphonia, there is an 80% likelihood a foreign body is present, causing at least partial obstruction. Symptoms of drooling and inability to handle secretions are indicative of a near-total esophageal obstruction. If symptoms are restricted to retrosternal chest pain or pharyngeal discomfort, less than 50% of patients will still have a foreign body present. Patient localization of where an ingested foreign object is lodged is not accurate, with only a 30% to 40% correct localization in the esophagus and essentially a 0% accuracy for foreign bodies in the stomach. Once the object reaches the stomach, small intestine, or colon, the patient will not report symptoms unless a complication occurs (e.g., obstruction, perforation, bleeding).
Patients with rectal foreign bodies are frequently asymptomatic, but embarrassment may interfere with obtaining an accurate history. Presentation is often after the patient or another person has made multiple attempts to remove the object. Symptoms may include anorectal pain, bleeding, and pruritus, with a small number of patients presenting with more serious complications, including obstruction, perforation, and peritonitis.
Past medical history is useful to identify previous foreign body ingestion; repeat offenders are likely to ingest multiple and more complex foreign objects. A history of dysphagia in a person with a food impaction or esophageal foreign body suggests a high likelihood of underlying esophageal pathology. Previous food impaction or need for esophageal dilation makes recurrent episodes more likely. A history of allergies (e.g., asthma, allergic rhinitis, food allergy) may be a clue that a patient may have eosinophilic esophagitis.
Physical examination does little to secure the diagnosis or location of a retained foreign body, but it is crucial to identifying already developed complications related to foreign body ingestion. Assessment of the patient’s airway, ventilatory status, and risk for aspiration are crucial prior to initiating therapy to remove a GIFB. A neck and chest examination looking for crepitus, erythema, and swelling can suggest a proximal perforation. Lung examination should be performed to detect the presence of aspiration or wheezing. An abdominal examination should be performed to evaluate for signs of perforation or obstruction.
Plain films of the chest and abdomen are recommended for patients presenting with suspected foreign body ingestion to determine the presence, type, number, and location of foreign objects present. Radiologic evaluation is not routinely needed for patients with non-bony food impactions who have no complications. Both anteroposterior and lateral chest films are needed because lateral films will aid in determining if a foreign body is in the esophagus or the trachea and may detail foreign bodies obscured by the overlying spine in an anteroposterior film. Biplanar neck films are recommended if there is a suspected object or complication in the hypopharynx or cervical esophagus. Plain films are also useful in identifying complications like free air, aspirations, or subcutaneous emphysema ( Fig. 28.4 ).

Unfortunately, radiography cannot image nonradiopaque objects (e.g., plastic, glass, wood) and may miss small bones or metal objects. The false-negative rate for plain film investigation of foreign bodies is as high as 47%, with false-positive rates up to 20%. False-negative rates for food impactions have been reported as high as 87%. If continued clinical suspicion or symptoms warrant, the individual should undergo further clinical investigation.
Use of plain films in children is more controversial because of the inability of the child to give a history and the associated radiation exposure. Some have suggested mouth-to-anus screening films to detect the presence of foreign bodies in children. Bedside US has been effective in identifying esophageal foreign bodies in children without the need of radiation. Also to limit radiation, hand-held metal detectors have been used, with a sensitivity ranging from 89% to 95% for detection and localization of metallic foreign bodies.
Barium studies are generally not recommended for evaluating GIFBs. Aspiration of hypertonic contrast agents in patients with complete or near-complete esophageal obstruction may lead to aspiration pneumonitis. Barium may also delay or impair the performance of a therapeutic endoscopic intervention by interfering with endoscopic visualization. Even if a barium study is considered normal, an endoscopy is still recommended if symptoms persist or suspicion of a foreign body is high.
CT or MRI are rarely necessary for the diagnosis of GIFBs. However, CT has been found to detect foreign bodies missed by other modalities and may aid in detecting complications of foreign body ingestion, such as perforation or abscess, prior to the use of endoscopy. CT of the cervical esophagus or hypopharynx prior to endoscopic investigation may benefit diagnosis.
Endoscopy provides the most precise means to diagnose suspected foreign bodies or food impactions. This ensures an almost 100% diagnostic accuracy for objects within the reach of the endoscope, including nonradiopaque objects and objects obscured by overlying bony structures that are not visualized by radiography.
Endoscopy allows the most accurate diagnosis of the underlying pathology, such as esophageal strictures, which may have led to a food impaction or impacted esophageal foreign body. Endoscopy also allows visualization of mucosal defects, abrasions, or ulcerations that may have resulted from the foreign body. Diagnostic endoscopy is also linked to the most efficacious therapy for GIFBs, the use of therapeutic endoscopy to remove or treat the object.
Diagnostic upper endoscopy for foreign bodies is relatively contraindicated when there are clinical or radiographic signs of perforation. Once an ingested foreign object has passed the ligament of Treitz, endoscopy is generally not indicated, because these objects will typically pass unimpeded with notable exceptions (see later). Similarly, most small (<2.5 cm) blunt objects in an adult patient’s stomach do not require endoscopic retrieval; most will pass without complication.
Treatment of GIFBs should always be planned with the knowledge that 80% to 90% of GIFBs will spontaneously pass through the GI tract without complication. This has led some investigators to suggest that all foreign bodies can be managed with conservative observation. Although conservative management is effective in most cases of GIFB, it is more appropriate to perform selective endoscopy for treatment based on the location, size, and type of foreign body ingested.
Several medical therapies have been considered as primary treatment of esophageal foreign bodies and food impactions. The smooth muscle relaxant glucagon is the most widely used and studied drug for the treatment of esophageal food and foreign object impactions. Glucagon, given in intravenous doses of 0.5 to 2 mg, can produce relaxation of the lower esophageal sphincter by as much as 60%, with the potential to permit passage of the impacted food or foreign body. Success with glucagon ranges from 12% to 58% in treating food impactions. A multicenter study showed glucagon to be effective in only 14% of cases, not statistically different from patients who did not receive glucagon. A small randomized study showed no benefit of glucagon administration over placebo. Glucagon may cause nausea, vomiting, and abdominal distention and has little effect when a fixed obstruction is present, preventing passage of the foreign body. Nifedipine and nitroglycerin are not recommended because of hypotension-related side effects and questionable efficacy.
Gas-forming agents like carbonated beverages or preparations consisting of sodium bicarbonate and citric acid have been described for treating esophageal impactions. They are purported to release carbon dioxide gas to distend the lumen and act as a piston to push the object from the esophagus into the stomach. However, the effectiveness of this method is doubtful, and perforations have been reported associated with use of gas-forming objects. Similarly, the meat tenderizer papain is not recommended for treatment of esophageal meat impactions; its lack of efficacy and risk of complications (e.g., perforation, mediastinitis) have been described.
Radiologic methods to treat esophageal foreign bodies are often successful. Under fluoroscopic guidance, Foley catheters, suction catheters, wire baskets, and magnets have been used to retract objects. The most commonly described extraction device is the Foley catheter; its tip is passed beyond the object, the balloon inflated, then the object is withdrawn into the oropharynx. Success with this method under fluoroscopy has been described as better than 90%. However, all radiographic methods suffer from lack of control of the object, particularly at the level of the upper esophageal sphincter and hypopharynx. Complications include nosebleeds, laryngospasm, aspiration, perforation, and even death. Radiographic methods are generally recommended only if flexible endoscopy is unavailable.
Flexible endoscopy has become the treatment of choice for GI food impactions and foreign bodies because it is safe and highly efficacious. Multiple large series have reported the success rate for endoscopic treatment of GIFBs to be more than 95%, with complication rates of less than 5%. The risk for complications is increased when sharp or multiple objects are ingested and when ingestion is intentional as opposed to accidental.
Because most GIFBs pass spontaneously without causing symptoms, it is important to understand the indications and timing for endoscopic intervention. Generally, all foreign bodies lodged in the esophagus require urgent intervention. The risk for an adverse outcome from an esophageal foreign body or food impaction is directly related to how long the object or food dwells in the esophagus. Ideally, no object should be left in the esophagus longer than 24 hours.
Once in the stomach, most ingested objects will pass spontaneously, and the risk of complications is much lower, making observation acceptable. There are notable exceptions. Sharp and pointed objects are associated with perforation rates as high as 15% to 35%. Objects longer than 5 cm and round objects wider than 2.5 cm also may not be passed and should be removed from the stomach with an endoscope at presentation or if they have not progressed in 3 to 5 days. If a more complex or sharp object has progressed beyond the stomach and cannot be retrieved, periodic radiographs should be obtained to document progression through the GI tract. The patient should then be followed for any symptoms suggestive of obstruction or perforation (e.g., fever, tachycardia, abdominal pain, distention). Alternatively, with the increasing use of double and single balloon enteroscopy, case reports have detailed the use of these scopes to safely and effectively retrieve foreign bodies from the small bowel. Given that most foreign bodies pass without sequelae upon reaching the small intestine, use of balloon-assisted enteroscopy should take into consideration the type of object and the patient who ingested it. Accessories including baskets, hoods, and forceps have been designed for balloon enteroscopes to enable foreign body retrieval.
Sedation to facilitate endoscopy for the management of food impactions and ingested foreign objects should be individualized. Conscious sedation is adequate for treating most food impactions and simple foreign bodies in the adult population, but anesthesia assistance may be required for uncooperative patients or patients who have swallowed multiple complex objects (see Chapter 42 ). Endoscopy for treatment of foreign bodies in the pediatric population is usually performed with the aid of anesthesia and endotracheal intubation.
For management of impactions and ingestions below the level of the laryngopharynx, flexible endoscopy is preferred. Rigid esophagoscopy and flexible nasoendoscopes can be used but provide no additional benefit and are often available to only a few endoscopists. A comparison of rigid versus flexible endoscopes to treat esophageal foreign bodies found significantly fewer perforations with flexible endoscopes. Laryngoscopes with the aid of a Kelly or McGill forceps can be useful for proximal foreign bodies and small sharp objects in the hypopharynx.
Availability of and familiarity with multiple endoscopic retrieval devices for removal of foreign bodies and food impactions is critical ( Box 28.1 ). An endoscopy suite and/or travel cart should be equipped with at least rat tooth or alligator grasping forceps, polypectomy snare, Dormia basket, and retrieval net. Overtubes of 45 and 60 cm in length should be available to the endoscopist. An overtube allows protection of the airway, multiple exchanges of the endoscope, and mucosal protection from sharp objects. The longer 60-cm overtube enables retrieval of sharp and complex objects from the stomach and encompasses the lower esophageal sphincter. An alternative adjunct for extraction of sharp objects is a latex protection hood that fits onto the tip of the endoscope (discussed later).
Flexible endoscope
Rigid endoscope
Laryngoscope
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here