Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The goals of fluid administration are to optimize tissue oxygenation by augmenting intravascular volume, improving left ventricular preload, and increasing cardiac output. This chapter reviews the timing and considerations for choice of therapy in volume repletion and the effects of fluid volume overload in the postresuscitation period.
Studies from the early 2000s suggested that earlier recognition and treatment of septic shock correlated with improved outcomes. In a report by Rivers and colleagues, the Early Goal-Directed Therapy Collaborative Group randomized subjects to receive either intensive treatment for septic shock within the initial 6 hours of therapy or standard therapy provided in the emergency department. Standard and early goal-directed therapy (EGDT) groups received antibiotics, vasoactive medications, and intravenous (IV) fluid for volume resuscitation. Goals for fluid administration included infusion of crystalloid in 500-mL boluses every 30 minutes with a target central venous pressure of 8–12 mm Hg as a marker of effective repletion of intravascular volume and response to fluids. Although the total volume of fluid administered by 72 hours was equivalent, the EGDT group received substantially more IV fluid in the first 6 hours of treatment. Compared with the standard therapy group, significant improvements related to in-hospital mortality were observed in the group assigned to earlier administration of volume-based resuscitation in conjunction with other therapies, including the optimization of central venous oxygen saturation with red blood cell transfusions and use of inotropes, if necessary. In-hospital mortality was 30.5% in the EGDT group, compared with 46.5% in the standard therapy group ( P = 0.009). Replication of results in other studies prompted guidelines for the treatment of sepsis to include early volume repletion as part of protocol-based, quantitative resuscitation to reverse tissue hypoperfusion. , In the Surviving Sepsis Campaign, initial resuscitation recommendations for the first 6 hours included treatment aimed at maintaining a central venous pressure of 8–12 mm Hg, a mean arterial pressure more than or equal to 65 mm Hg, urine output more than or equal to 0.5 mL kg/hr, and mixed venous oxygen saturation greater than 65%. In 2018 the Surviving Sepsis guidelines were further revised to accelerate this protocol-driven timeline and include recommendations for initiating fluid resuscitation within 1 hour for hypotension or lactatemia.
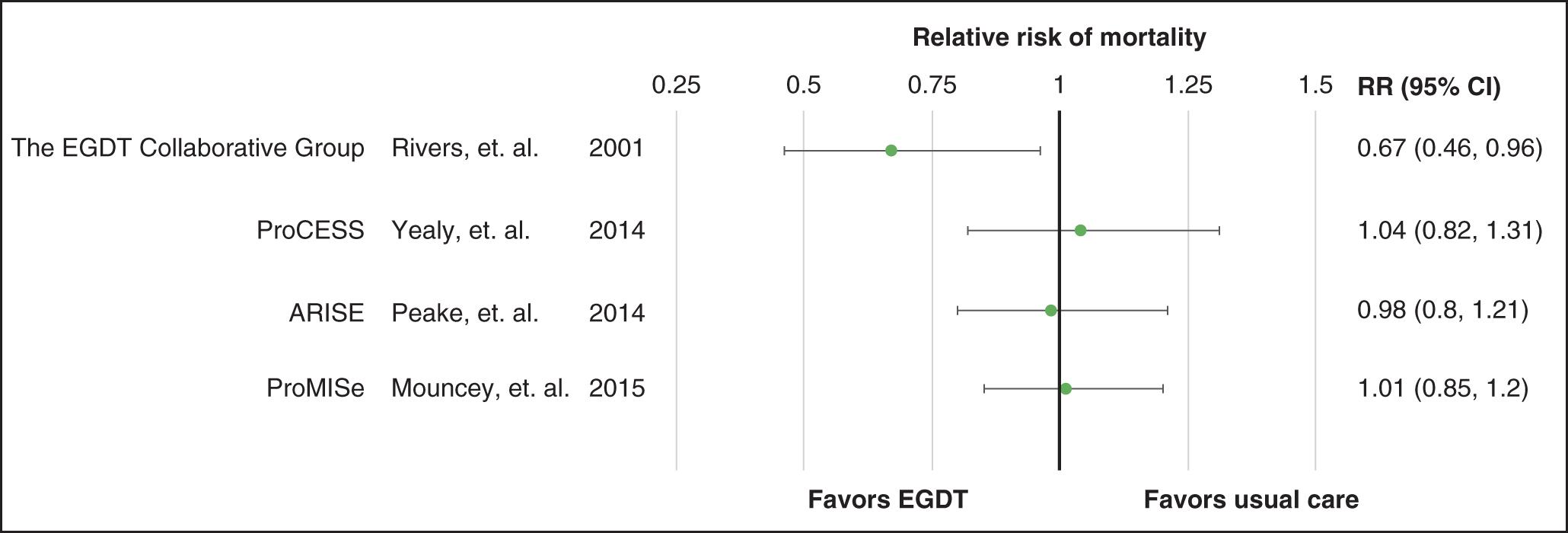
Meeting hemodynamic stabilization endpoints in such a manner with goal-directed therapy and other supportive measures remains desirable in most cases, especially in patients who prove to be fluid responsive. However, other multicenter studies that have re-examined this topic have not replicated survival benefits, and the advantages of aggressive EGDT have been questioned. The Australasian Resuscitation in Sepsis Evaluation (ARISE) study examined EGDT resuscitation in patients with septic shock. Sixteen hundred patients were randomized to EGDT or usual care. On average, patients in the EGDT group were treated with more IV fluid in the initial 6 hours of therapy compared with those randomized to usual care. Those in the EGDT group were also more likely to receive red blood cell transfusions. At 90 days, no significant differences were observed in patient survival. In-hospital mortality, the duration of organ support, and the length of hospital stay were also similar. The Protocol-based Care for Early Septic Shock (ProCESS) investigative group showed comparable results, with no benefits found with EGDT. ProCESS was a prospective multicenter trial that randomized 1341 emergency department patients with septic shock to receive 6 hours of protocol-based EGDT, protocol-based standard therapy, or usual care. The investigators did not require placement of central venous catheters, administration of inotropes, or blood transfusions in the protocol-based standard therapy group, as compared with the use of these therapies in the EGDT group. Overall, the total volume of fluid administered during the 6-hour study period was reported as being significantly different between the groups. Again, no differences in survival were observed at 90 days. There was also no significant impact on 1-year mortality, the duration of time spent on mechanical ventilation, or the duration of time on renal replacement therapy. ProMISe was a pragmatic randomized trial that examined mortality and other critical illness outcomes in patients with septic shock across 56 hospitals in England. Participants were randomized to either EGDT or usual care. A total of 1260 patients were enrolled, and there were no statistically significant between-group differences in mortality or the other secondary outcomes, including adverse events and quality of life. Additionally, EGDT increased the cost of care for these critically ill patients. Fig. 99.1 shows the relative risk of mortality in EGDT versus usual care in these four major randomized controlled trials.
When deciding on IV fluid therapy, the choices can be broadly classified into three major categories. Crystalloid fluids have long been considered the mainstay of volume replacement in the hospital setting and include normal saline (NS), lactated Ringer’s (LR) solution, Hartmann’s solution, and other balanced salt solutions such as Plasma-Lyte. A second broad category includes colloid preparations such as albumin, hydroxyethyl starch (HES), dextran, and gelatin. Finally, blood products, including packed red blood cells, can be used for volume repletion in the treatment of hypoperfusion caused by inadequate circulating volumes. Table 99.1 compares the osmolality and composition of human plasma and common isotonic crystalloid fluid preparations.
| Plasma | 0.9% Normal Saline (NS) a | Lactated Ringer’s (LR) b | Plasma-Lyte-LYTE A (PL) c | Sterile Water With 150 mEq/L Sodium Bicarbonate d | |
|---|---|---|---|---|---|
| Osmolality (mOsmol/L) | 280–310 | 308 (calc) | 273 (calc) | 294 (calc) | 300 (calc) |
| Sodium (mEq/L) | 135–145 | 154 | 130 | 140 | 150 |
| Potassium (mEq/L) | 4.0–5.0 | – | 4.0 | 5.0 | – |
| Chloride (mEq/L) | 95–110 | 154 | 109 | 98 | – |
| Calcium (mEq/L) | 2.2–2.6 | – | 2.7 | – | – |
| Magnesium (mEq/L) | 1.0–2.0 | – | – | 3.0 | – |
| Lactate (mEq/L) | 0.8–1.8 | – | 28 | – | – |
| Acetate (mEq/L) | – | – | – | 27 | – |
| Gluconate (mEq/L) | – | – | – | 23 | – |
| Bicarbonate (mEq/L) | 24–31 | – | – | – | 150 |
a Baxter Healthcare Corp. Sodium Chloride Injection, USP. Package Insert.
b Baxter Healthcare Corp. Lactated Ringer’s Injection, USP. Package Insert.
c Baxter Healthcare Corp. Plasma-Lyte A Injection pH 7.4, USP. Package Insert.
d Hospira, Inc. Sodium Bicarbonate Injection, USP. Package Insert.
The choice between crystalloids and colloids as therapeutic fluids in the intensive care unit (ICU) has long been a topic of debate and investigation. In an analysis of multiple population studies, Goldwasser and Feldman observed that mortality was inversely associated with serum albumin levels. With each 2.5 g/L lower serum albumin concentration, a correlative 24%–56% increase in risk of death was detected. This relationship held true in healthy populations and in those who suffered from acute and chronic illnesses. Several mechanisms for the protective effects of the albumin molecule have been explored. Among these, infused albumin reportedly has free radical scavenging antioxidant properties that may have clinical importance. Moreover, the proposed advantages for prescribing colloid over crystalloid fluid in resuscitation strategies for critically ill patients include concepts based on hemodynamic Starling’s principles and the role of plasma oncotic pressure. Theoretically, large colloid molecules that persist in the circulation enhance water reabsorption from the interstitial space and maintain the volume within the vasculature for longer periods. Ideally, this characteristic would reduce the large fluid volumes that are often required for resuscitation and improve clinical outcomes.
Prospective randomized trials examining the potential benefits of albumin and colloids in lieu of crystalloid solutions for volume repletion have yielded variable results. For example, there are investigations that demonstrated benefit with albumin administration and support its clinical safety. In one such study, a group of 100 patients with hypoalbuminemia in the ICU were randomized to receive (versus not receive) albumin as part of their treatment regimen. The groups were well matched and had similar baseline serum albumin concentrations and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores. Significant improvements in Sequential Organ Failure Assessment (SOFA) scores were observed in the albumin-treated group. Interestingly, significant decreases in fluid gains were also seen in the albumin-treated group. These results led the investigators to suggest that treatment with albumin may lead to better outcomes in critically ill patients with hypoalbuminemia. Similarly, the Saline versus Albumin Fluid Evaluation (SAFE) study was a large trial that included nearly 7000 ICU patients with trauma, acute respiratory distress syndrome (ARDS), and severe sepsis. The participants were randomized to receive either 4% albumin or NS for intravascular fluid resuscitation. In a subgroup analysis of patients with severe sepsis, those in the albumin-treated group had a significantly lower heart rate and a significantly higher central venous pressure on days 1–3. No between-group differences were detected in the total SOFA score, and similar numbers of patients required renal replacement therapy in the saline- and albumin-treated groups. Multivariate logistic regression analysis revealed that the adjusted odds ratio (OR) for death in the albumin-treated versus saline-treated group was 0.71 (85% confidence interval [CI]: 0.52–0.97; P = 0.03), suggesting that albumin treatment may decrease the risk of death in severe sepsis. Furthermore, data from a meta-analysis suggested that albumin administration is safe. In 55 trials that evaluated many different types of patients, including those with trauma, burns, hypoalbuminemia, and ascites, albumin administration did not adversely affect mortality.
In contrast to studies suggesting benefit with albumin therapy in sepsis, other large prospective randomized trials failed to support a clear benefit of infusing albumin over crystalloid solutions in patients in the ICU setting. In the larger and more diverse group of original SAFE study participants discussed earlier, investigators found no between-group differences in death or new episodes of single- or multiorgan system failure between those treated with albumin versus saline. There was also no significant difference in the number of days spent in the ICU, length of hospital stay, or days of renal replacement therapy in the subgroup analyses. Similarly, the Colloids Versus Crystalloids for the Resuscitation of the Critically Ill (CRISTAL) trial examined outcomes for ICU patients with shock from sepsis, trauma, or hypovolemia who were randomized to treatment with colloid solutions compared with crystalloids. In addition to 4% and 20% albumin, the colloid arm of CRISTAL included gelatins, dextrans, and HES. At 28 days after study enrollment, even though colloid resuscitation was associated with fewer days of mechanical ventilation and more days without vasopressor therapy, no significant differences in mortality were observed between the patients who received colloids and those who received crystalloids. Patients with severe sepsis have also been randomized to receive crystalloid plus albumin therapy compared with crystalloids alone. In the more than 1800 randomized patients in the Albumin Italian Outcome Sepsis (ALBIOS) study, significantly higher mean arterial pressures and lower net fluid gains were observed in the albumin plus crystalloid therapy group. However, the investigators also noted that the total daily amount of fluids administered did not differ between the groups and, more importantly, there were no significant differences in patient survival at 28 or 90 days between the groups. The Cochrane analysis of pooled data on this topic also found no evidence that colloids reduced the risk of death compared with crystalloids in the treatment of critically ill patients. Overall, there remains a paucity of data to suggest that clear benefits exist for administering albumin or other colloid solutions instead of crystalloids in critically ill patients requiring volume repletion. The lack of resounding benefit is compounded by the high cost of albumin, which also makes it less attractive for routine use.
There is also evidence suggesting that colloid solutions such as albumin may be associated with harmful effects. Though they tended to have higher critical illness severity scores, patients in the Sepsis Occurrence in Acutely ill Patients (SOAP) study who received albumin at any time during their ICU stay had a higher risk of death. A systematic review of 37 randomized trials comparing crystalloid with colloid administration also hinted at safety concerns. The investigators found that colloid resuscitation was associated with a 4% increase in the absolute risk of mortality (95% CI, 1.00–1.08) and concluded that the difference in the effect of the colloids was not related to the types of inciting injuries.
The harm associated with colloid infusion may be more pronounced with respect to specific organ systems or types of colloids. In a post hoc analysis of the SAFE study, albumin administration in patients with traumatic brain injury was associated with higher mortality compared with those who received crystalloids.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here