Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neonatal hypotonia, often referred to as the “floppy infant,” is the main presenting clinical feature of most neuromuscular diseases of early life. However, disorders of the central nervous system may also manifest with hypotonia.
Two types of muscle tone can be assessed clinically: postural and phasic. Postural (antigravity) tone is a sustained, low-intensity muscle contraction in response to gravity. It is mediated by both gamma and alpha motor neuron systems in the spinal cord, and it is assessed clinically by passive manipulation of the limbs. Phasic tone is a brief contraction in response to a high-intensity stretch. It is mediated by the alpha motor neuron system only, and is examined clinically by eliciting the muscle stretch reflexes. Hypotonia is defined as reduction in postural tone, with or without a change in phasic tone. When postural tone is depressed, the trunk and limbs cannot overcome gravity, and the child appears hypotonic or floppy.
After a careful general physical examination, the neurologic assessment needs to include an evaluation of primary neonatal reflexes, a sensory examination, and, most importantly, a motor examination. Muscle tone is assessed by passive manipulation of the infant's limbs.
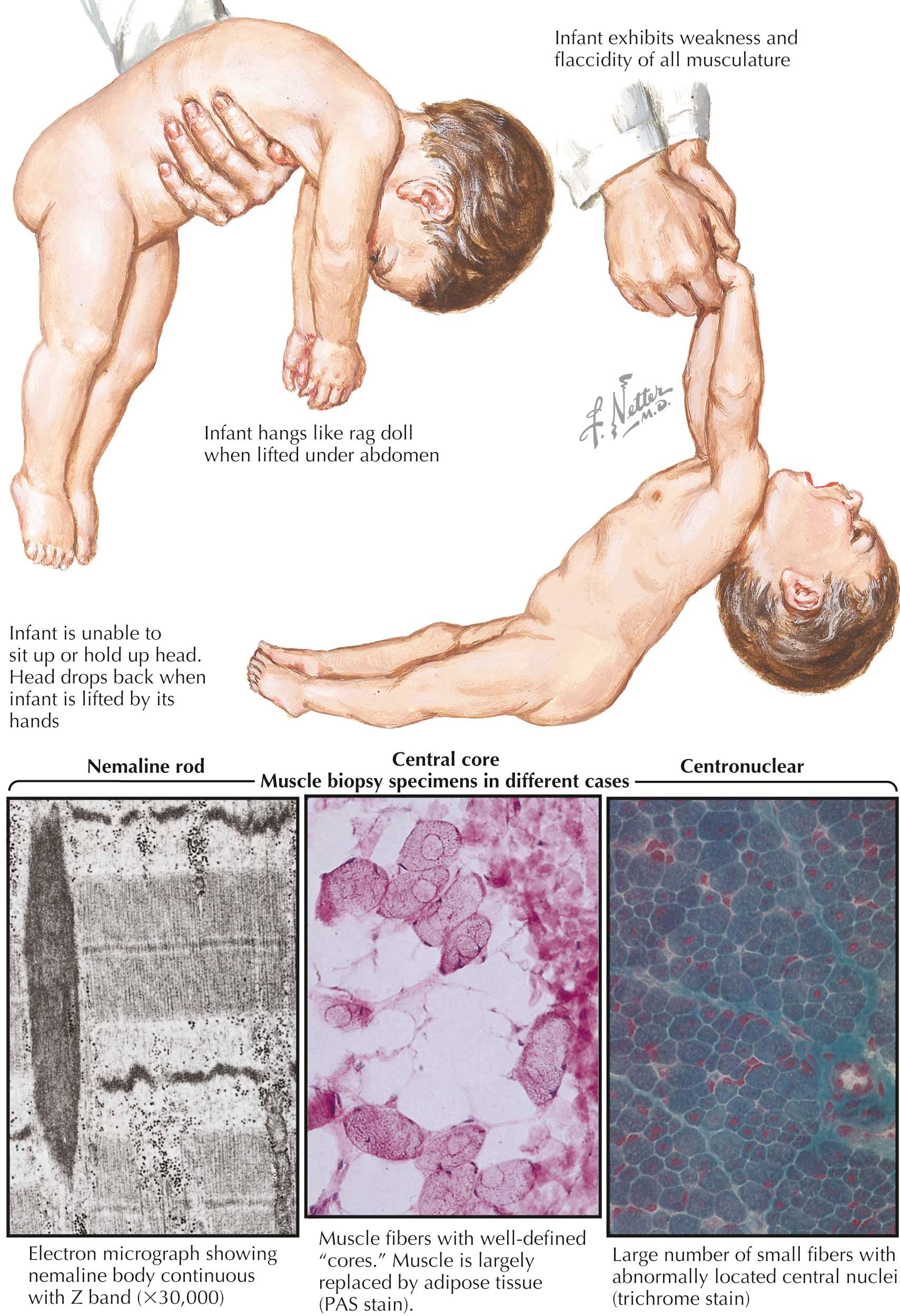
Muscle tone can be evaluated further by performing the traction response, vertical suspension, and horizontal suspension maneuvers. A floppy infant exhibits “head lag,” “slips through” the examiner's hands on vertical suspension, and “drapes over” the examiner's hand on horizontal suspension.
Neonatal hypotonia may be the manifestation of pathology involving the central nervous system (CNS), the peripheral nervous system (i.e., lower motor unit), or both. In infants with cerebral or central hypotonia (nearly two thirds of these cases), the perinatal or prenatal history may suggest a CNS insult. There may also be associated global (rather than an isolated gross-motor) developmental delay, occasionally seizures, microcephaly, dysmorphic features, and/or malformation of the brain and/or other organs. Central hypotonia may be associated with brisk and/or persistent primitive reflexes and normal-brisk muscle stretch reflexes. The degree of weakness noted in these infants is usually less than the degree of hypotonia ( “nonparalytic” hypotonia) .
In lower motor unit hypotonia or peripheral hypotonia , developmental delay is primarily gross-motor and is associated with absent or depressed muscle stretch reflexes and/or muscle atrophy and fasciculations of the tongue. In general, antigravity limb movements are decreased and cannot be elicited via postural reflexes. In these infants, the degree of weakness is proportional or in excess of the degree of hypotonia (“paralytic” hypotonia ). Trauma to the high cervical cord due to traction in breech or cervical presentation may also initially manifest itself as flaccid paralysis, which may be asymmetric, and initially muscle stretch reflexes are absent; later on, however, upper motor neuron signs develop.
Because muscle tone is also determined by the viscoelastic properties of muscle and joints, connective tissue disorders, such as Marfan and Ehlers-Danlos syndromes, osteogenesis imperfecta, and also benign ligamental laxity, can present with hypotonia. In addition, a combined cerebral and lower motor unit hypotonia occurs in infants and older children as a presenting manifestation of congenital myotonic dystrophy, some congenital muscular dystrophies, peroxisomal disorders, mitochondrial encephalomyopathies, neuroaxonal dystrophy, leukodystrophies (e.g., globoid cell leukodystrophy), familial dysautonomia, and asphyxia secondary to motor unit disease. Further, hypotonia without significant weakness may be a feature of systemic diseases, such as sepsis, congenital heart disease, hypothyroidism, rickets, renal tubular acidosis, and others.
Neuromuscular diseases in infancy manifest primarily with hypotonia and weakness ; however, infants with severe hypotonia but only marginal weakness usually do not have a disorder of the lower motor unit (anterior horn cell, peripheral and cranial nerves, neuromuscular junction, and muscle). These infants may have genetic conditions, metabolic disturbances, or as discussed above, systemic disorders (e.g., congenital heart disease, renal failure, etc.).
Spinal muscular atrophy (SMA) is an autosomal recessive hereditary illness. Rarely, variant forms exist, including X-linked and dominant forms. It is one of the two most common causes for a floppy infant secondary to lesions of the peripheral motor unit. The most common form of SMA is the proximal recessive type, which includes a broad range of subtypes, ranging from the severe infantile variant (depicted here) to ambulatory forms with adult onset.
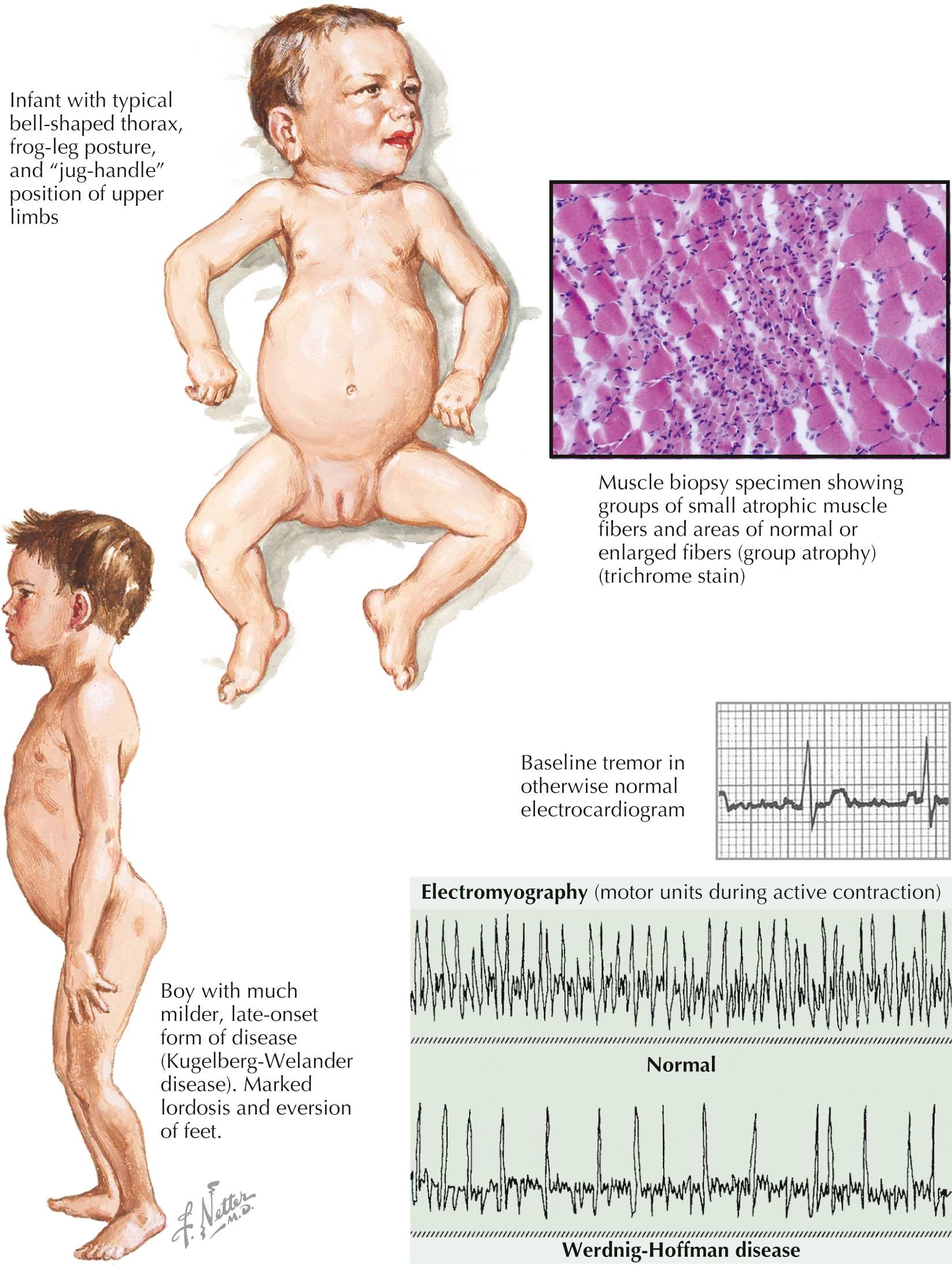
In the healthy newborn infant, purposeless extremity movements have a well-defined muscular tone, despite the lack of coordinated motor function. Concomitantly, full-term newborns have well-developed suck and swallow function. At birth, many SMA type I infants appear normal; however, within a few weeks to months, generalized hypotonia and neuromuscular weakness develop. A classic hypotonic posture characterized by abducted hips, internal rotation of the forearms, and frog-legged and jug-handle habitus is typical. Their respiratory pattern is characterized by paradoxic chest and abdomen movement resulting from selective intercostal muscle weakness with preserved diaphragm function. Without supportive treatment, such infants subsequently develop characteristic bell-shaped deformities of the thorax. Progressive bulbar and respiratory insufficiency results in a vulnerability to both aspiration and infectious pneumonias.
Extraocular and facial movements are preserved; these infants typically have a bright, attentive countenance. Careful evaluation of the tongue reveals tongue fasciculations. In contrast to adult motor neuron disorders, fasciculations in limbs are difficult to appreciate due to excessive subcutaneous infantile fat. Abnormal motor milestones with poor head control, inability to roll and to achieve independent sitting, as expected during the first few months, leads to investigation and eventual diagnosis of SMA type I. In a most severe subset, reduced fetal movements occurs prenatally; these infants are born with generalized hypotonia, weakness, respiratory insufficiency, bulbar dysfunction, and proximal joint contractures.
Spinal muscular atrophy with respiratory distress (SMARD) is distinguished by early respiratory failure due to diaphragm involvement, especially in association with more distal presentation of limb weakness. X-linked SMA manifests as a severe infantile SMA variant predominantly affecting males.
SMA II infants initially can sit but never become able to walk and are diagnosed at ages 6 to 24 months. Kugelberg-Welander disease, SMA III, typically occurs between ages 2 and 14 years with symptoms of proximal weakness. These children may have mild elevations of creatinine kinase (CK, <1000 IU/L).
More than 95% of SMA I infants have a homozygous deletion/mutation of exon 7 of the survival motor neuron 1 gene ( SMN1 gene) on chromosome 5q11-13. Infants who do not have this deletion identified may have a non–chromosome 5 SMA or a mutation(s) in the survival motor neuron gene not detectable with the currently used polymerase chain reaction (PCR)-based methods. Both SMA II and SMA III have exactly the same genetic defects as those with type I. When a child with proximal muscle weakness, shown by electromyography (EMG), demonstrates neurogenic changes, deoxyribonucleic acid (DNA) testing for SMN1 gene is the diagnostic tool of choice.
Electromyography is a very sensitive primary diagnostic tool; however, it has been largely supplanted by DNA analysis. However, when DNA testing is normal and significant weakness is manifest, the EMG findings are distinct in type I SMA, demonstrating diffuse fibrillations in virtually all muscles in association with markedly reduced recruitment of small motor units in the absence of the typical large complex motor units characteristic of reinnervation in milder, more chronic forms of the disorder. Muscle biopsy demonstrates findings typical of neurogenic atrophy, although the reduced reinnervation capacity in SMA type I often results in a predominance of small rounded fibers within entirely denervated fascicles.
Other lesions in the motor unit can mimic Werdnig-Hoffmann disease (WHD), but, as a rule, can be differentiated by clinical and electromyographic findings and examination of muscle biopsy specimens if genetic and/or neurophysiologic testing are not definitive. Differential diagnosis includes the very rare recessive inherited peripheral neuropathy variants, such as congenital hypomyelinating neuropathy that may clinically mimic WHD, even to the point of tongue fasciculations. More distally within the motor unit, neuromuscular junction disorders, including transient neonatal myasthenia gravis and infantile botulism, as well as the various congenital myopathies and dystrophies, may present as a floppy baby.
Treatment for Werdnig-Hoffmann disease remains largely supportive. The prognosis is generally poor, with onset is in the neonatal period. Many of these infants do not survive until their first birthday. However, even in the absence of extensive supportive care, historically, up to 30% of infants with SMA type I survive beyond 2 years of age, some into adolescence or beyond.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here