Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The underlying mechanism for most defects related to problems associated with failed first-trimester obstetric procedures is vascular disruption.
With chorionic villus sampling, removal of villi may result in embryonic hypotension, hypoxia, endothelial damage, hemorrhage, and necrosis with tissue loss involving distal structures in the upper body (hands and tongue), with middle digital rays more affected than medial or lateral rays.
Failed dilatation and uterine curettage in early pregnancy has also been associated with fetal oromandibular limb hypogenesis syndrome, which is consistent with the role of hypoxic trauma in inducing fetal structural defects in early pregnancy.
Maternal hyperthermia during the late first trimester, resulting in fever greater than 39°C for more than 2 days, can cause severe congenital limb disruption with hypoglossia, hypodactylia, terminal transverse hemimelia, and Möbius sequence.
Infants who survive attempted termination of pregnancy (both surgical and medical) are at increased risk to be born with arthrogryposis and intellectual disability as well as terminal transverse hemimelia and Möbius sequence.
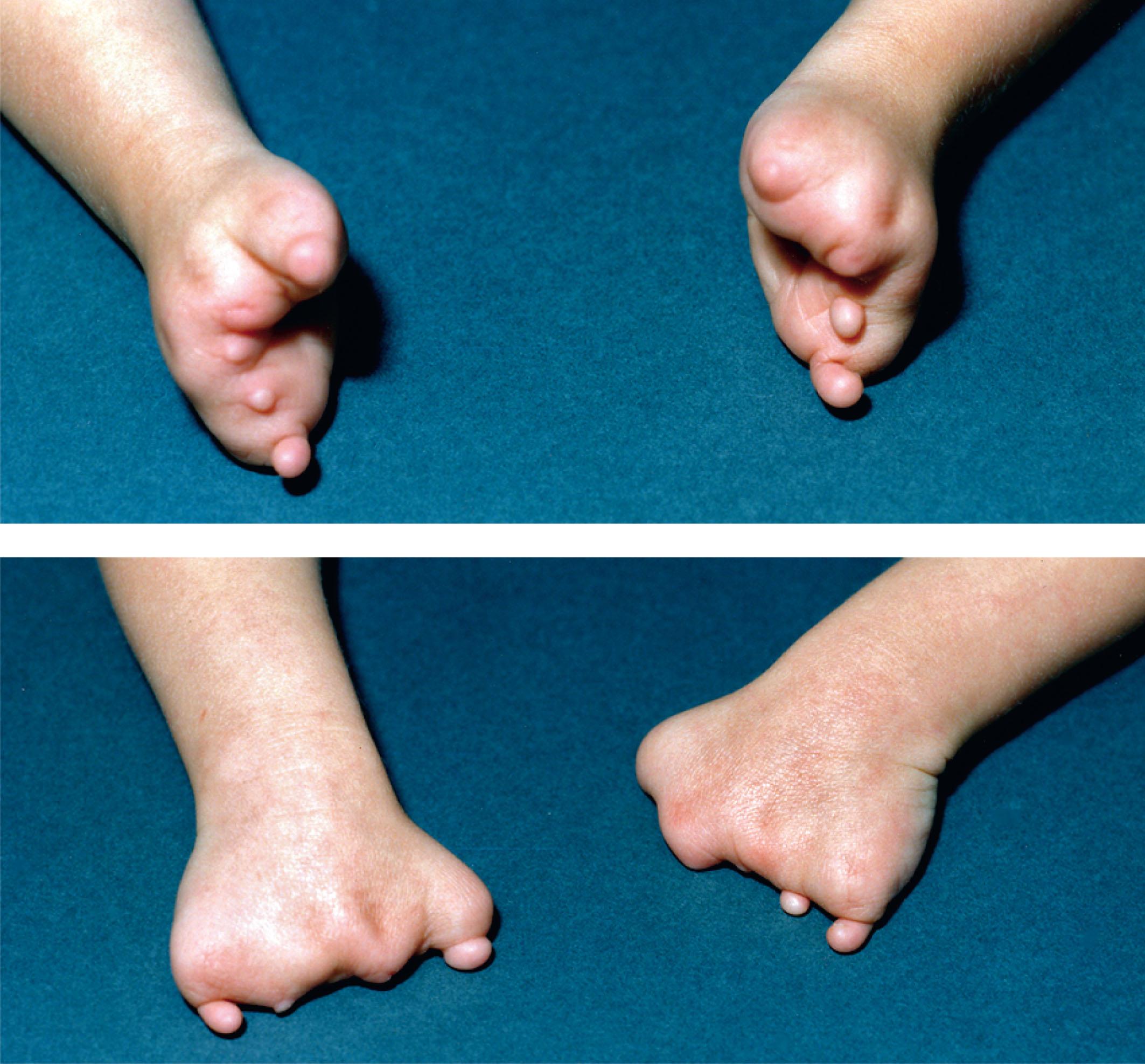
The underlying mechanism for most defects related to problems associated with failed obstetric procedures is vascular disruption. With chorionic villus sampling (CVS), removal of villi may result in embryonic hypotension, hypoxia, endothelial damage, hemorrhage, and necrosis with tissue loss. Defects are more likely to involve distal structures in the upper body (hands and tongue) than proximal structures or the lower body, with middle digital rays more affected than medial or lateral rays ( Fig. 50.1 ). Absence of the distal portion of the third finger, with tapering and stiff joints, appears to be a distinctive effect of exposure to CVS.
Following blunt trauma to the placenta, Quintaro et al. noted numerous ecchymoses that might be related to the increased frequency of hemangiomas in CVS-exposed infants.
Limb defects caused by vascular disruption have a birth prevalence of 0.22 per 1000, accounting for 34% of all limb-reduction defects (which occur with a prevalence rate of 0.69 per 1000). The frequency of terminal transverse limb-reduction defects is significantly higher after CVS than in nonexposed pregnancies, with earlier procedures resulting in more severe types of defects and a higher frequency of procedure-related defects. The estimated risk for terminal transverse defects after early CVS is estimated to be between 1:1000 and 1:3000. Therefore it is recommended that CVS only be performed after 10 weeks of gestation. Most experienced operators try to insert the CVS catheter into the chorion frondosum because if the catheter enters the decidua, it can cause hemorrhages. Loss rates after CVS increase with the number of insertions, and inexperienced operators usually require more insertions to obtain adequate samples.
The embryo is normally in a state of partial hypoxia, and because of this state of partial hypoxia, disturbances in the embryo’s oxygen supply can more easily lead to a damaging degree of hypoxia. In an experimental setting, mammalian embryos show a surprising degree of resilience to hypoxia, with many organogenic-stage embryos able to survive 30 to 60 minutes of anoxia, but in some embryos this degree of hypoxia causes abnormal development, particularly transverse limb reduction defects. These abnormalities are preceded by hemorrhage, edema, and tissue necrosis. Other parts of the embryo are also susceptible to such hypoxia-induced damage, and these include the genital tubercle, the developing nose, the tail, and the central nervous system. Animal models of hypoxia during early stages of organ development result in patterns of limb defects with more severe destruction of the feet compared with the hands and hypoplasia of digits two through four, particularly the third digit. In human fetuses with hypoxia due to homozygous alpha thalassemia, this same pattern of distal limb deficiency has been identified. Animal studies indicate that hypoxic episodes in the first trimester of human pregnancy could occur by temporary constriction of the uterine arteries. This also could be a consequence of exposure to cocaine, misoprostol, or severe shock resulting from failed attempts at pregnancy termination.
Similar exposures have resulted in hypoxia-related malformations in the human, and fetal limb-reduction defects have been reported after early hypoxic injury, such as CVS before 66 days’ gestation. Failed dilatation and uterine curettage in early pregnancy has been associated with fetal oromandibular limb hypogenesis syndrome, which is consistent with this hypothesis concerning the role of hypoxic trauma in inducing fetal structural defects in early pregnancy.
Case reports of infants born after failed attempts at dilatation and curettage describe vascular disruption defects such as limb-reduction defects and amniotic band–related defects affecting the limbs, facial clefts, and cranium. Failed termination of pregnancy is a relatively rare occurrence, with estimates ranging from 0.02% to 0.07% when termination is undertaken by dilation and curettage or dilation and extraction. Among 2500 unselected patients with arthrogryposis, there were 11 cases of failed termination of pregnancy in which the individuals were subsequently born with arthrogryposis. Infants who survive attempted termination of pregnancy (both surgical and medical) are at increased risk to be born with multiple congenital contractures. Among infants who survived attempted termination of pregnancy and had arthrogryposis, more than half also had intellectual disability. Maternal cocaine use during pregnancy has been associated with congenital contractures, suggesting that vascular compromise may play a role in this type of limb anomaly, and maternal trauma also leads to vascular compromise of the fetus and arthrogryposis. A woman who conceived with an intrauterine device in place had the device removed at 7 weeks’ gestation, and her sonogram at 25 weeks’ gestation revealed transverse limb reduction of the right forearm. A dichorionic-diamniotic twin was born with hydrocephalus, clubfeet, and hypoplastic toes following myomectomy at 12 weeks’ gestation for a 10-cm posterior retroplacental subserous uterine myoma. Severe abdominal trauma at 52 days postconception, caused by blunt trauma to the abdomen, resulted in terminal transverse limb-reduction defects and porencephaly.
Maternal hyperthermia during the late first trimester, resulting in fever greater than 39°C (102.2 °F) for more than 2 days, can cause severe congenital limb disruption with hypoglossia, terminal transverse hemimelia, and Möbius sequence ( Fig. 50.2 ). In a metaanalysis of 22 studies, maternal influenza exposure was defined as any reported influenza, influenza-like illness, or fever with influenza, with or without serologic or clinical confirmation during the first trimester of pregnancy. First-trimester maternal influenza exposure was associated with an increased risk for neural tube defects (odds ratio [OR]: 3.33; 95% confidence interval [CI]: 2.05–5.40), hydrocephaly (OR: 5.74; 95% CI: 1.10–30.00), congenital heart defects (OR: 1.56; 95% CI: 1.13–2.14), aortic valve atresia or stenosis (OR: 2.59; 95% CI: 1.21–5.54), ventricular septal defect (OR: 1.59; 95% CI: 1.24–2.14), cleft lip (OR: 3.12; 95% CI: 2.20–4.42), digestive system abnormalities (OR: 1.72; 95% CI: 1.09–2.68), and limb-reduction defects (OR: 2.03; 95% CI: 1.27–3.27). Associations between maternal reports of periconceptional fever and transverse limb deficiency and intercalary limb deficiency were confirmed in a subsequent large study, which found no association with longitudinal limb deficiency, which is more likely to have a genetic basis. This study also noted associations between maternal fever and intestinal atresia, as well as spina bifida. When there is a history of significant first-trimester hyperthermia in an infant with a transverse limb-reduction defect with or without other defects, the possibility of a febrile illness causing these defects should be considered.

When administered inappropriately, first-trimester misoprostol and/or methotrexate for induction of abortion can result in damage to a continuing pregnancy. In 1998, it became apparent that misoprostol, a synthetic prostaglandin E1 analog used in the prophylaxis and treatment of peptic ulcers, was being used to induce abortion in South and Central America where abortions are illegal. A study of 42 infants from São Paulo, Brazil, who were exposed to misoprostol during the first trimester revealed distinctive patterns of birth defects due to vascular disruption: 17 infants had equinovarus with cranial nerve defects and 10 had equinovarus as part of more extensive arthrogryposis. The most distinctive phenotypes were arthrogryposis confined to the legs (five cases) and terminal transverse limb defects (nine cases) with or without Möbius syndrome. In a study of 265 women exposed to misoprostol during the first trimester and followed through delivery, the main indication for misoprostol was voluntary abortion (60.9%). Ten major malformations (5.5%; 95% CI: 2.65–9.82%) were reported, and five of them were consistent with the pattern of malformations attributed to misoprostol: Möbius sequence, hydrocephalus, terminal transverse limb reduction associated with a clubfoot, syndactyly, and posterior encephalocele. A prospective study of first-trimester misoprostol exposure after medical prescriptions found the malformation rate was higher among 236 exposed pregnancies (4%) than in 255 controls (1.8%). Three malformations in the exposed group were consistent with the misoprostol-specific spectrum (2%). In a systematic review and metaanalysis of 4899 cases of congenital anomalies and 5742 controls, prenatal exposure to misoprostol was associated with an increased risk of Möbius sequence and terminal transverse limb defects.
Methotrexate is a folate antagonist that is used to treat malignancies and rheumatoid or inflammatory autoimmune diseases. It is also used for the nonsurgical treatment of ectopic pregnancies and the elective termination of pregnancy, and it is teratogenic when used in high doses for cancer or termination of tubal pregnancy. A prospective study of women exposed to low-dose methotrexate for rheumatologic conditions revealed one case of typical methotrexate embryopathy ( Fig. 50.3 ) among the eight exposed pregnancies. Among 188 postconception methotrexate-exposed pregnancies at dosages typically used in the treatment of rheumatic diseases, there was an increased risk of spontaneous abortion (42.5%) and major birth defects (6.6%) when compared to a cohort of disease-matched controls and to women without autoimmune disease. Occasionally, methotrexate and misoprostol are used together to terminate a pregnancy. Data from eight patients who were exposed to both medications in the first trimester indicated a significant teratogenic risk. Reported anomalies included growth deficiency, absence or hypoplasia of the frontal bones, craniosynostosis, large fontanelle, ocular hypertelorism, short palpebral fissures, wide nasal bridge, malformed and low-set ears, micrognathia, syndactyly, short forearms, missing ribs, dislocated hips, and talipes equinovarus.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here