Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Describe viable and nonviable pregnancy with appropriate terminology
List sonographic features of failed pregnancy
Describe sonographic findings of retained products of conception
Explain the clinical and sonographic findings in ectopic pregnancy
Discuss the normal range for fetal cardiac rhythm
Describe the cranial abnormalities seen in the first trimester
Distinguish among normal bowel herniation, gastroschisis, and omphalocele
Explain the sonographic findings with cystic hygroma in the first trimester
Name the types of umbilical cord masses that may be seen with ultrasound
Differentiate between a hemorrhagic corpus luteum cyst and other ovarian masses
Discuss the difference between a fibroid and uterine contraction on sonography
The first trimester consists of a series of complex, sequential events that make up the early stage of embryonic development. Interruption in development may lead to complications in the embryonic period. Approximately 15% of clinically recognized pregnancies are spontaneously miscarried. The loss rate may be even higher for early pregnancies that are not clinically recognized. The most common presentation for complications is vaginal spotting or frank bleeding, which occurs in nearly 25% of patients during the early stage of pregnancy. In many cases, bleeding is inconsequential, resulting from implantation of the conceptus into the decidualized endometrium. However, if bleeding is accompanied by severe pain, uterine contractions, or a dilated cervix, the pregnancy is unlikely to progress. Patients benefit from early transvaginal examination to carefully investigate the uterine cavity for the presence of an embryo, a fetal heartbeat, a yolk sac, or retained products of conception.
A threatened abortion covers a wide range of conditions based on the stage of development and the sonographic appearance of the products of conception. Threatened abortion is a term used for pregnancies of fewer than 20 weeks when the patient has a viable embryo, documented fetal heartbeat, and vaginal bleeding. The diagnosis of threatened abortion is made when the cervix is long and closed in a patient with vaginal bleeding. At least 50% of pregnant women with these complications will go on to spontaneously lose or “abort” the pregnancy. Specific terminology has been adopted to describe the complications of these pregnancies. Embryonic demise , or failed pregnancy , is used when there is clear evidence of a nonviable embryo (absence of cardiac activity). Blighted ovum , or anembryonic pregnancy , is used to describe a uterus containing a gestational sac but no visible embryo. Pregnancy of unknown location (PUL) refers to the patient who has a positive urine or serum pregnancy test but presents with no intrauterine nor ectopic pregnancy visualized on transvaginal ultrasound.
Other conditions that may present clinically as a threatened abortion are ectopic pregnancy and gestational trophoblastic disease. Knowledge of the quantitative level of serum human chorionic gonadotropin (hCG) is necessary to make this diagnosis and should be correlated with the sonographic appearance.
Historically the diagnosis of pregnancy failure has relied upon several diagnostic criteria: the absence of cardiac activity at a certain crown-rump length (CRL), the absence of a visible embryo at a certain mean sac diameter (MSD), or the absence of an appreciable embryo by a point in time. These criteria were reviewed by the Society of Radiologists in Ultrasound (SRU), whose consensus paper was published in the New England Journal of Medicine (NEJM) in October 2013. The SRU believed that the previous studies which determined these threshold values were based on very small patient populations and that the criteria were at risk for increased false-positive results. These criteria reflect their attempt to increase the specificity to 100% and give a positive predictive value of close to 100%. The goal was to prevent erroneously diagnosing nonviability and preventing surgical or medical intervention that damages a true viable pregnancy. See the criteria in Boxes 48.1 and 48.2.
The embryonic placenta, or frondosum, may become detached, resulting in the formation of a hematoma, which typically causes vaginal bleeding. Most of these hemorrhages are contiguous with a placental edge. Although no risk factors have been associated with first-trimester placental separation, it has been reported to have a 50% or greater fetal loss rate. Although the prognosis seems to depend on the size of the hematoma, no specific volumes have been correlated in the first trimester with fetal outcomes. That said, improved outcomes do seem to be consistent with smaller hematomas.
Sonographically, placental hematomas may be difficult to distinguish from subchorionic hemorrhages. Patients who present with placental hematomas generally do not have symptoms, bleeding, or spotting because the bleed is within the chorionic sac and has no communication with the endometrium.
The most common occurrence of bleeding in the first trimester is from subchorionic hemorrhage. These low-pressure bleeds result from the process of implantation of the fertilized ovum into the endometrial cavity and myometrial wall. The hemorrhage is found between the myometrium and the margins of the gestational sac and may or may not be associated with the placenta. This finding can help to distinguish a subchorionic hemorrhage from abruptio placentae, which generally occurs in the second trimester and may present as a lucency posterior to the placenta. Clinical findings may include bleeding, spotting, or uterine cramping. If the hemorrhage becomes large enough, this can lead to spontaneous pregnancy loss (SPL).
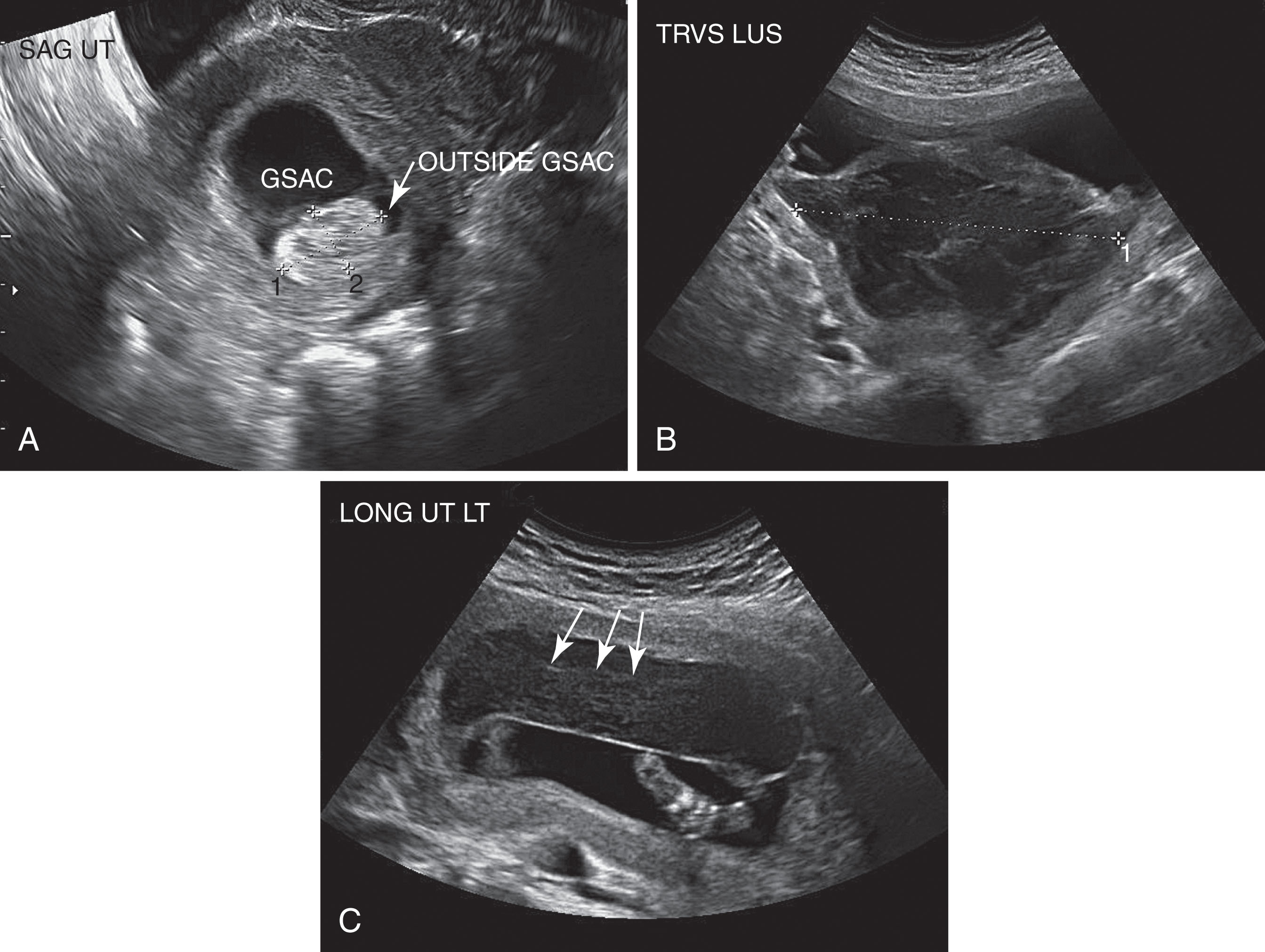
The appearance of bleeding varies with the stage of its organization. An early bleed may appear slightly echogenic as the red blood cells actively fill the area of hemorrhage. With time, the hemorrhage becomes more anechoic and may be seen between the uterine wall and the fetal membrane ( Fig. 50.1 ). Color flow Doppler will demonstrate the avascular nature of the hemorrhage. Patients may present with active vaginal bleeding, and the subchorionic bleed is easily seen by ultrasound adjacent to the gestational sac. Other patients may have no bleeding yet have a subchorionic lucency that can be seen with imaging. Patients may be symptomatic with a large subchorionic bleed, or asymptomatic with a small subchorionic bleed, perhaps only seen with transvaginal imaging.
Sonography is routinely used to evaluate for the presence or absence of an intrauterine gestational sac. For example, if the patient presents with a positive pregnancy test with a normal sonographic appearance of the uterus but the endometrial complex shows no sign of a gestational sac, the differential diagnosis would include a very early intrauterine pregnancy, a nondeveloping pregnancy, or possible ectopic pregnancy.
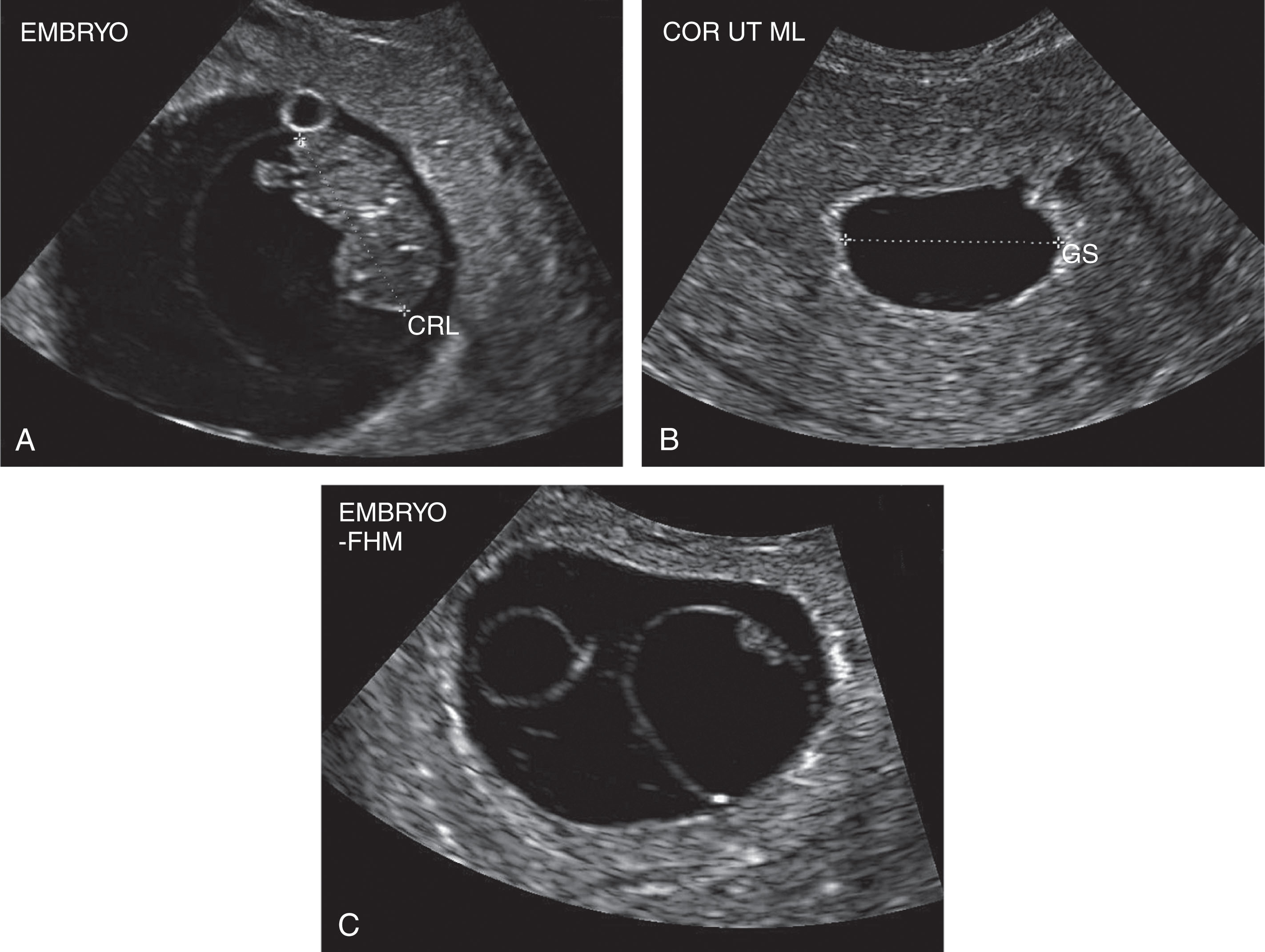
Characteristics for the sonographic diagnosis of an absent intrauterine sac include an empty uterus with no evidence of an endometrial fluid collection (early gestational sac), absence of adnexal masses or free fluid, and positive beta-hCG levels. Clinical findings may be characterized by bleeding and cramping. Correlation between the serum beta-hCG level and uterine findings can be used to confirm whether the sonographic indications of a first-trimester pregnancy have been met. Recall that the gestational sac is identified sonographically at 4 to 5 weeks’ gestation. The sac grows approximately 1 mm per day in the first trimester. The yolk sac should be visualized transvaginally when the gestational sac reaches 8 mm in size, and the embryo must be visualized when the MSD measures 25 mm. The normal embryo grows at a rate of 1 mm/day. Cardiac activity is visible by 5.5 to 6.5 weeks ( Table 50.1 ). Failure to observe these developmental markers suggests a pregnancy of “uncertain viability” (PUV). Applying the SRU criteria, pregnancy failure can be definitively stated when the embryo is 7 mm or greater without a heartbeat or the MSD is 25 mm but no embryo is visible.
| Terminology | Comments |
|---|---|
| Viable | A pregnancy is viable if it can potentially result in a liveborn baby. |
| Nonviable | A pregnancy is nonviable if it cannot possibly result in a liveborn baby. Ectopic pregnancies and failed intrauterine pregnancies are nonviable. |
| Intrauterine pregnancy of uncertain viability | A woman is considered to have an intrauterine pregnancy of uncertain viability if transvaginal ultrasonography shows an intrauterine gestational sac with no embryonic heartbeat (and no findings of definite pregnancy failure). |
| Pregnancy of unknown location | A woman is considered to have a pregnancy of unknown location if she has a positive urine or serum pregnancy test and no intrauterine or ectopic pregnancy is seen on transvaginal ultrasonography. |
| Diagnostic Tests | |
| Human chorionic gonadotropin (hCG) |
|
| Pelvic ultrasonography | Minimum quality criteria include transvaginal assessment of the uterus and adnexa and transabdominal evaluation for free intraperitoneal fluid and a mass high in the pelvis; oversight provided by an appropriately trained physician; scans performed by providers and interpreted by physicians, all of whom meet at least minimum training or certification standards for ultrasonography, including transvaginal ultrasonography; and scanning equipment permitting adequate visualization of structures early in the first trimester. |
In the case of pregnancy loss ( complete abortion ) , serial hCG levels demonstrate successive decline. Caution should be taken when a positive pregnancy test and an empty uterus are seen, given the possibility that an early normal intrauterine pregnancy between 3 and 5 weeks’ gestation may be present. Consequently, serial hCG levels should always be obtained and followed for appropriate rise or decline.
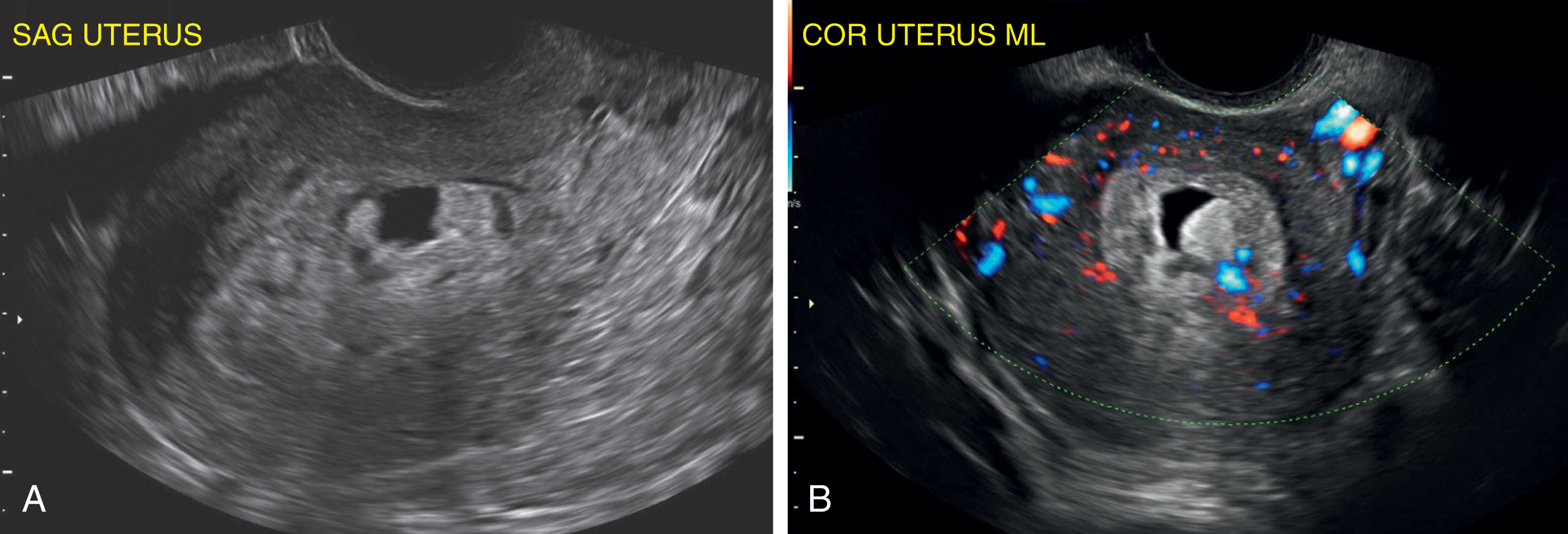
If the endometrium is abnormally thick or irregularly echogenic, the differential diagnosis includes intrauterine blood, retained products of conception after an incomplete spontaneous loss, a decidual reaction associated with an ectopic pregnancy, or decidual changes resulting from an early but not yet visible intrauterine pregnancy. Incomplete spontaneous abortion may show several sonographic findings, ranging from an intact gestational sac with a nonviable embryo to a collapsed gestational sac that is grossly misshapen ( Fig. 50.2 ). Women who are clinically undergoing a spontaneous abortion or who have had an elective termination often require follow-up sonography to determine whether retained products of conception are present. Sonographic signs of retained products may be subtle; a thickened endometrium greater than 8 mm and increased vascularization of the endometrial complex with color Doppler are strongly predictive. The presence of visible embryonic parts, a gestational sac, or an embryonic disk is obvious evidence of retained products of conception ( Fig. 50.3 ). It sometimes can be difficult to distinguish retained products of conception from blood clots. Quantitative hCG levels, which do not decline normally, a thickened endometrium, and increased vascular flow will provide discriminating evidence for retained products. Patients most often present with persistent bleeding after SPL, dilation and curettage, or being prescribed misoprostol for uterine evacuation.
A gestational sac without an embryo or yolk sac on sonography may represent one of three conditions: (1) a normal early intrauterine pregnancy of less than 5 weeks, (2) an abnormal intrauterine pregnancy, or (3) a pseudogestational sac in a patient with an ectopic pregnancy.
The gestational sac should be imaged consistently by both transabdominal and transvaginal sonography when its mean diameter is 5 mm, which corresponds to a gestational age of 4 to 5 weeks. Transvaginal sonography may demonstrate the sac as early as 4 weeks, when it measures 2 to 3 mm. At this early size the “sac” can be described only as an intrauterine fluid collection. This cannot be definitively called a gestational sac until there is further growth and a yolk sac can be identified. Measuring the gestational sac at this early stage provides a baseline for monitoring appropriate interval growth. Caution should be used in evaluating these early stages of pregnancy to allow for the possibility that a patient may have inaccurate dates for their last menstrual period. Sequential scanning can document appropriate interval growth of 1 mm per day. Lack of appropriate growth indicates an abnormally growing gestational sac or a pregnancy of unknown viability.
Regarding gestational sac values, a gestational sac may be seen as early as 4.3 weeks, the threshold level , and must be seen by 5.2 weeks, the discriminatory level . Given the new pregnancy failure criteria, absence of a gestational sac at this stage would also be termed PUV and follow-up ultrasound would be ordered.
Transvaginal sonography is the ideal method to examine the early gestational sac. When the sac measures 8 mm or greater, a definitive yolk sac should be demonstrated. The yolk sac can be expected to grow 0.1 mm per 1 mm of MSD growth, up to 15 mm. When the gestational sac measures 25 mm, an embryo with cardiac activity must be seen. Follow-up examination in 7 to 10 days is recommended if the findings are indeterminate.
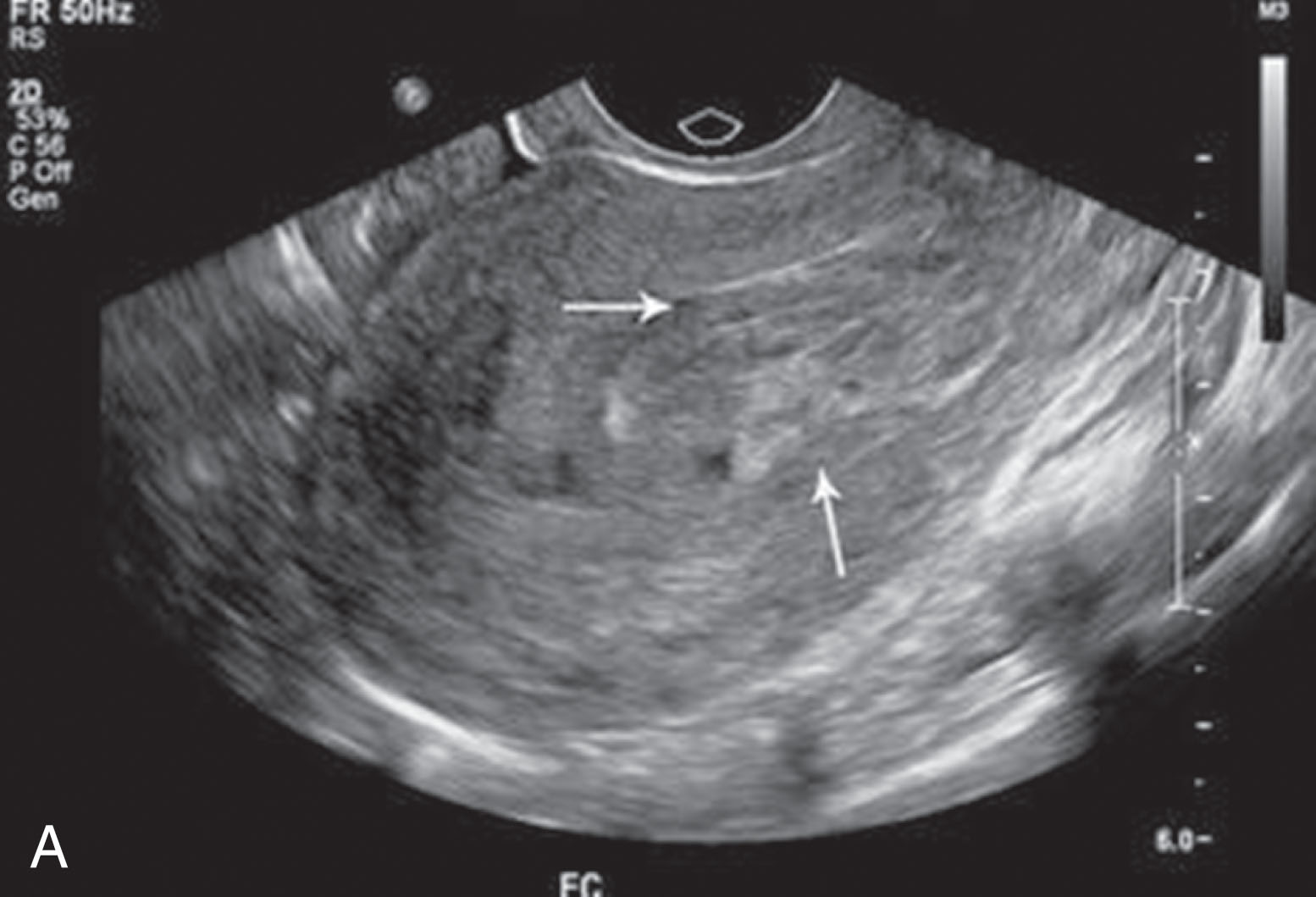
By definition, anembryonic pregnancy , or blighted ovum , is a gestational sac in which the embryo fails to develop or stops developing at such an early stage that it is imperceptible by ultrasound (see Table 50.1 ). The trophoblastic tissue may continue to proliferate despite the failed embryonic growth, the gestational sac will continue to grow, and hCG levels may continue to rise, although not at the expected rate. The typical sonographic appearance of anembryonic pregnancy is a large, empty gestational sac that does not demonstrate a yolk sac, an amnion, or an embryo ( Fig. 50.4 ). The MSD increases by 1.13 mm/day in a normal gestation, but the growth rate of an abnormal sac is only 0.70 mm/day. Therefore abnormal sac growth can be diagnosed when the MSD fails to increase by 0.6 mm/day. In subsequent repeat studies, the sonographer evaluates growth size of the sac, presence of the yolk sac, development of an embryo, and presence or absence of cardiac activity. Box 50.1 outlines several sonographic intrauterine findings associated with abnormal pregnancies. The SRU criteria for failed pregnancy in the presence of an empty sac is an MSD of 25 mm without an embryo.
Absence of cardiac motion in embryos ≥5 mm
Absence of cardiac motion after 6.5 menstrual weeks
Large yolk sac or amnion without a visible embryo
Calcified yolk sac
>18 mm lacking a viable embryo
>8 mm lacking a visible yolk sac
Irregular or misshapen
Cornual, low, or hour-glassing through cervical os
Irregular
Absent double decidual sac finding
Thin trophoblastic reaction <2 mm
Intratrophoblastic venous flow
Gestational sac growth of <0.6 mm/day
Absent embryonic growth
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here