Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The fetal spleen is an important center of hematopoiesis until the late fetal period. In postnatal life, the function of the spleen is mainly as an immune organ, with lymphocyte and monocyte production continuing throughout adult life. During fetal development, the spleen appears between the fifth and eighth gestational weeks as an aggregation of reticular mesenchymal cells in the dorsal epigastrium of the stomach. The gastrosplenic ligament connects the spleen to the greater curvature of the stomach, and the splenorenal ligament connects the spleen to the dorsal abdominal wall. The fetal spleen shows distinct lobules that disappear before birth. The developing spleen acquires its characteristic “coffee bean” shape early in the fetal period.
The fetal spleen is usually not seen on ultrasound (US) before 18 weeks, and absence of the spleen may be very difficult to prove by US. Several prospective observational studies have measured fetal spleen size and volume according to gestational age. Normal values for fetal spleen dimensions have been proposed. From a clinical point of view, the rationale for developing normal values is the association of splenic size with hematologic and infectious diseases and developmental syndromes. The proposed normal ranges for size and volume of the fetal spleen according to gestational age are summarized in Table 32.1 .
| Gestational Age (Completed Weeks) | Width Measured From Side to Side (cm) | Circumference (cm) | Area (cm 2 ) | Volume (cm 3 ) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schmidt et al. | Hata et al. | Aoki et al. | You et al. | Schmidt et al. | Aoki et al. | You et al. | Srisupundit et al. | Hata et al. | Aoki et al. | You et al. | You et al. | |
| 16 | 2.8 | |||||||||||
| 20 | 1.3 | 1.4 | 1.5 | 2.0 | 4.5 | 4.2 | S.2 | 4.4 | 0.6 | 1.0 | 1.3 | 0.7 |
| 24 | 2.5 | 2.0 | 2.2 | 2.3 | 6.1 | 6.1 | 6.2 | 6.0 | 1.9 | 2.2 | 1.9 | 1.2 |
| 28 | 3.1 | 2.5 | 2.9 | 3.0 | 7.4 | 79 | 79 | 7.6 | 3.2 | 3.6 | 3 1 | 2.3 |
| 32 | 3.8 | 3.1 | 3.5 | 3.5 | 8.9 | 9.5 | 9.6 | 9.1 | 4.5 | 5.2 | 4.7 | 4.0 |
| 36 | 4.8 | 3.6 | 4.0 | 4.1 | 10.9 | 11.0 | 11.2 | 10.6 | 5.8 | 70 | 6.4 | 6.3 |
| 40 | 6.2 | 4.2 | 4.3 | 13.8 | 12.3 | 12.0 | 71 | 9.0 | 7.2 | |||
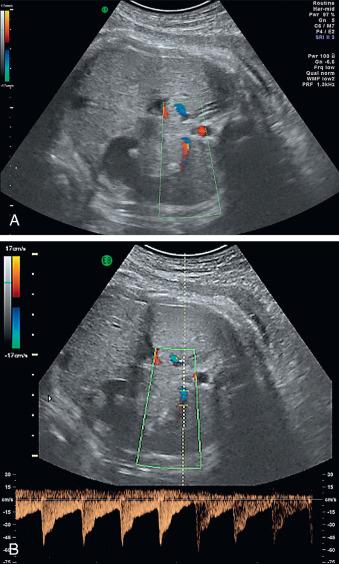
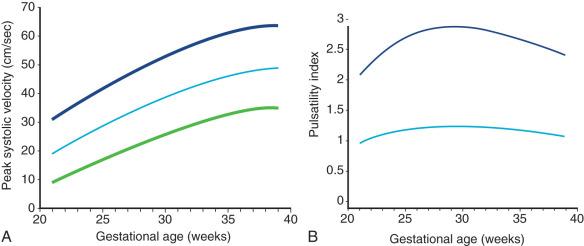
Doppler measurements of the splenic artery are another potentially clinically useful aspect of US assessment of the fetal spleen. Several groups reported the association of splenic artery pulsatility and flow velocities with fetal growth restriction and anemia. The splenic artery is usually visualized in an axial plane and can be identified by its course originating from the celiac trunk in front of the aorta and running behind the stomach to the spleen ( Fig. 32.1 ). Ebbing et al. published the first systematic longitudinal study of Doppler measurements in the fetal splenic artery and the celiac artery and proposed reference ranges for splenic artery pulsatility indices (PI) and peak systolic velocity (PSV). PI and PSV in the splenic artery were strongly and positively correlated with PI in the middle cerebral artery and the umbilical artery. Because Doppler measurements of the middle cerebral artery PI are widely used to assess potential anemic conditions of the fetus, Doppler velocimetry of the splenic artery could be useful as an additional tool to establish or confirm diagnosis. The study by Ebbing et al. also showed that splenic artery flow and celiac artery flow correlate with portocaval pressure and umbilical venous supply to the right liver lobe. For this reason, Doppler measurements of the splenic artery may provide a method for the differential assessment of splanchnic circulation in the fetus. Reference values for splenic artery Doppler measurements are provided in Fig. 32.2 .
The splenic vein can also be visualized in an oblique abdominal plane using Doppler. The flow pattern of the splenic vein is not pulsatile in normal conditions. Using Doppler, Musilova analyzed the flow pattern of the splenic vein in women with preterm prelabor rupture of membranes (PPROM), reporting that a pulsatile flow pattern in the splenic vein was predominantly observed in PPROM with chorioamnionitis (likelihood ratio 13.2), and with funisitis (likelihood ratio 5.7). They suggested that Doppler evaluation of the splenic vein could be a noninvasive tool for the prediction of these inflammatory complications. However, this single report lacks confirmation from other studies.
Pathologic findings of the spleen discovered during prenatal US screening examinations are mostly related to the location or size of the organ and the occurrence of malformations. Accessory spleens are a common finding in adults and are usually spherical homogeneous masses a few centimeters or less in size and with smooth borders. They are typically located near the splenic hilus or the tail of the pancreas but can be found anywhere else in the abdomen, where they can be mistaken for tumors. The complete absence of the spleen (asplenia) and a condition with multiple small spleens (polysplenia) are rare anomalies and should raise the suspicion for associated laterality and cardiac defects. US evaluation of the spleen can be important to establish the diagnosis or aid in the identification of numerous rare developmental disorders, such as cardiosplenic syndromes, polysplenia and situs inversus, and splenogonadal fusion limb defect.
Depending on histology and suspected etiology, splenic cysts can be divided into two types: primary cysts (approximately 25% of all splenic cysts), which are formed by cellular layers and have an inner epithelium; and secondary cysts or pseudocysts, which consist of a fibrous capsule. Primary cysts can be neoplastic and originate as dermoids, epidermoids, hemangiomas, or lymphangiomas. Secondary cysts are believed to be of posttraumatic, inflammatory, or degenerative origin.
Congenital splenic cysts are generally considered to be rare. However, since the advent of high-resolution fetal US scans, splenic cysts have been regularly detected and reported. The exact prevalence of congenital splenic cysts is unknown. A review of 13 cases was published by Kabra.
The exact origin of congenital splenic cysts is unclear. However, several etiologic mechanisms have been proposed, such as invasion of pluripotent stem cells into the fetal spleen, invagination of peritoneal endothelial cells during development, inclusion of cellulous mesothelium during organogenesis, or dilatation of normal lymphatic areas within the spleen.
Congenital splenic cysts are usually diagnosed during prenatal US from week 20 onward, typically as chance findings. In postnatal life, larger congenital splenic cysts can become symptomatic because of expansion, rupture, and bleeding, manifesting as sudden abdominal incidents.
The typical US pattern of a congenital cyst is an anechoic cyst with smooth walls. Epidermoid cysts have a complex pattern with irregularities and thickness of the posterior walls because of epithelial peripheral trabeculations and internal echoes from blood clots. Pseudocysts occasionally may be sonolucent, but calcifications are more frequently observed. Infarcts are characteristically triangular. Fresh hematomas appear hyperechoic, with subcapsular fluid collection.
There are only few reports on the use of magnetic resonance imaging (MRI) for the diagnosis of splenic cysts. On both T1-weighted and T2-weighted scans, splenic cysts usually have signal intensity equal to that of water; however, depending on the composition of the cystic fluid, the signal intensity in T1-weighted images may increase.
The differential diagnosis of a fetal abdominal cystic mass includes the following:
splenic cyst
renal cyst
hydronephrosis (see Chapter 12 )
cystic dysplasia of the kidneys (see Chapters 15 and 16 )
obstruction-duplication of the urinary tract (see Chapters 12 and 13 )
adrenal cyst (see Chapter 17 )
hepatic cyst (see Chapters 24 , 25 , and 28 )
choledochal cyst (see Chapter 25 )
pancreatic pseudocyst
mesenteric cyst (see Chapter 24 )
urachal cyst
omental cyst (see Chapter 24 )
congenital duplication of stomach
duodenal atresia (see Chapter 26 )
ovarian cysts (see Chapter 24 )
giant hydrosalpinx
No prenatal treatment of congenital splenic cysts has been reported.
Most authors agree that congenital splenic cysts have a good prognosis; spontaneous regression of the cysts occurs in many cases. For this reason, most authors recommend an expectant approach. In the rare cases in which congenital splenic cysts become symptomatic—most often through progressive enlargement, infection, bleeding, or rupture—various interventional procedures have been suggested. Besides surgical options, percutaneous drainage and sclerotherapy with alcohol have been applied successfully.
Congenital splenic cysts are usually incidental findings with a good prognosis. However, the detection of congenital splenic cysts should prompt an evaluation for cystic structures in other organs—in particular, kidney, liver, pancreas, and lungs—to rule out the possibility of polycystic disease.
Defects in the development of normal human left-right asymmetry result in so-called heterotaxy syndromes (see Chapter 91 ). The best-known heterotaxy syndrome is situs inversus, in which unpaired thoracic and abdominal organs are positioned in a mirror-image fashion but are otherwise structurally normal. The more common partial defects in left-right asymmetry result in so-called situs ambiguus or cardiosplenic syndromes. Situs ambiguus or cardiosplenic syndromes are divided into two distinct conditions: polysplenia syndrome/left isomerism and asplenia syndrome/right isomerism.
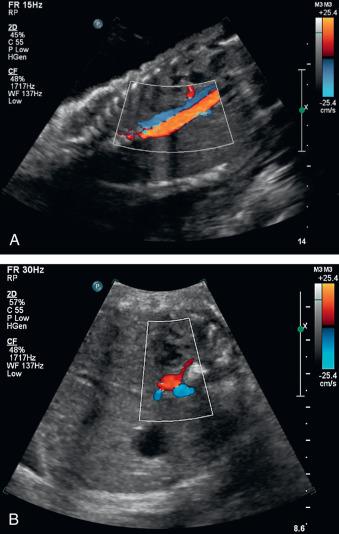
Polysplenia syndrome, or left isomerism (bilateral left-sidedness, also known as Ivemark syndrome ), is characterized by paired left-sided viscera. The hallmark findings of this condition are multiple spleens associated with cardiac anomalies (often ventricular or atrioventricular septal defects and outflow tract abnormalities) and heart block. Also typical of this condition are bilateral bilobed lungs, a malpositioned stomach, a midline liver, and interruption of the inferior vena cava with the venous return from the lower body occurring over the prominent azygos vein (right to the aorta) or hemiazygos vein (left to the aorta), running parallel to the descending aorta ( Fig. 32.3 and ![]() and
and ![]() ).
).
Asplenia syndrome, or right isomerism (bilateral right-sidedness), is characterized by agenesis of the spleen in combination with paired right-sided viscera. Typical findings are right atrial isomerism with bilateral superior vena cava, multiple and more severe cardiac anomalies (including anomalous pulmonary venous connections, often atrioventricular septal defects, and outflow tract abnormalities), bilateral trilobed lungs, and a midline liver. The association of asplenia with cardiovascular anomalies was first described by Ivemark.
In the Baltimore-Washington Infant Study, the incidence of cardiac defects associated with left-right asymmetry malformations was estimated at 1.44 : 10,000. This figure might be an underestimation because not all left-right asymmetry malformations are deleterious, and malformations without severe cardiac defects might go undiagnosed for a long time.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here