Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The facial nerve, also known as the seventh cranial nerve, combines motor, general sensory, special sensory, and autonomic (visceral) components. The intricate course of the facial nerve as it runs intracranially, intratemporally, and extratemporally is essential for any surgeon operating in the head and neck to understand. The facial nerve innervates the muscles derived from the second branchial arch and carries sensory and parasympathetic fibers of the nervus intermedius. The facial muscles, also known as mimetic muscles, function to protect the eye, maintain the nasal airway, provide oral continence, and articulate speech. Equally as important, these mimetic muscles provide humans the means for emotional expression and interpersonal communication. This chapter details an anatomic description of the facial nerve and musculature with a focus on anatomy and physiology as they relate to facial nerve disorder and treatment.
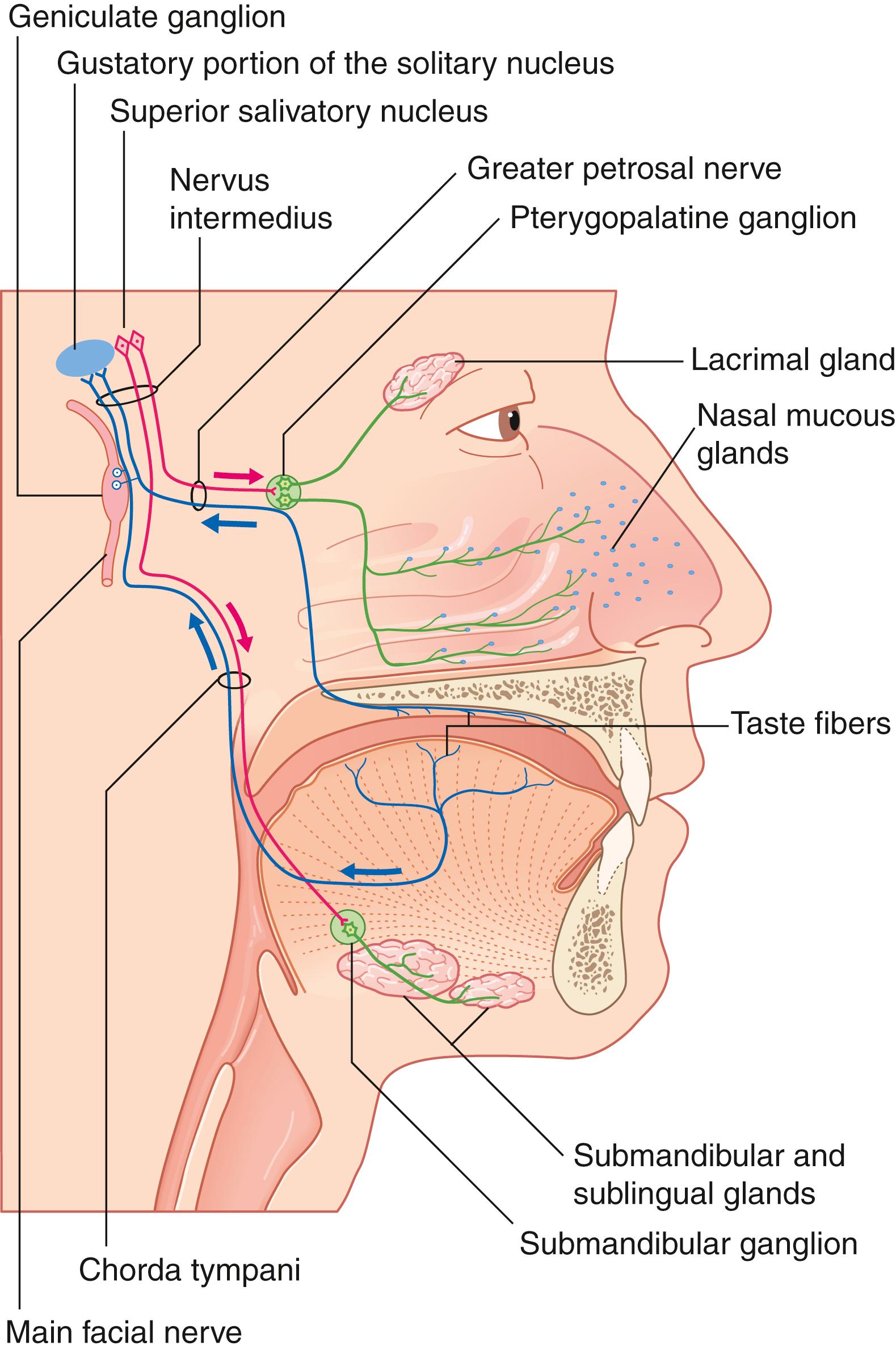
The facial nerve provides a diverse range of functions via efferent and afferent innervation to structures of the second branchial arch. The most well-associated function of the facial nerve is its innervation of striated muscles of facial expression. These functions will be the focus of this chapter. However, additional efferent motor fibers provide innervation to the stapedius muscle, the stylohyoid muscle, and the posterior belly of the digastric. Collectively, these motor fibers represent the special visceral efferents comprising the majority of the facial nerve fibers. The remaining efferent fibers of the facial nerve are general efferent fibers and form autonomic contributions. These autonomic nerves travel via the greater superficial petrosal nerve (GSPN) to the lacrimal gland and seromucinous glands of the nasal cavity and via the chorda tympani to the submandibular and sublingual glands. Traveling with this autonomic system, v isceral afferent fibers supply visceral sensation to the mucosa of the nose, pharynx, and palate. Additional afferent inputs include special sensory fibers and somatic sensory fibers. Special sensory fibers for taste to the anterior two-thirds of the tongue, tonsillar fossa, and palate originate from the geniculate ganglion cell bodies and travel within the chorda tympani and GSPN. Somatic sensory fibers provide touch sensation to the external auditory canal and conchal skin of the auricle as well as proprioceptive information from the facial muscles ( Fig. 1.1 ).
Facial muscle movement starts with a conscious or unconscious impulse in the motor cortex of the precentral gyrus of the cerebral hemispheres. The majority of cerebral fibers then project to the contralateral facial motor nucleus via the corticobulbar tract through the thalamus along the posterior limb of the internal capsule. However, a subset of cerebral fibers controlling movement of the frontalis and upper orbicularis oculi project to both the ipsilateral and contralateral facial motor nuclei. A central lesion will thus cause frontalis-sparing facial paralysis due to the bilateral contributions to the upper face. The precentral gyrus fibers synapse in the facial motor nucleus, residing in the pontine tegmentum. Postsynaptic fibers then travel dorsally within the brainstem, loop around the floor of the fourth ventricle at the facial colliculus, and exit the ventrolateral aspect of the brainstem at the caudal border of the pons in the cerebellopontine angle ( Fig. 1.2 ).
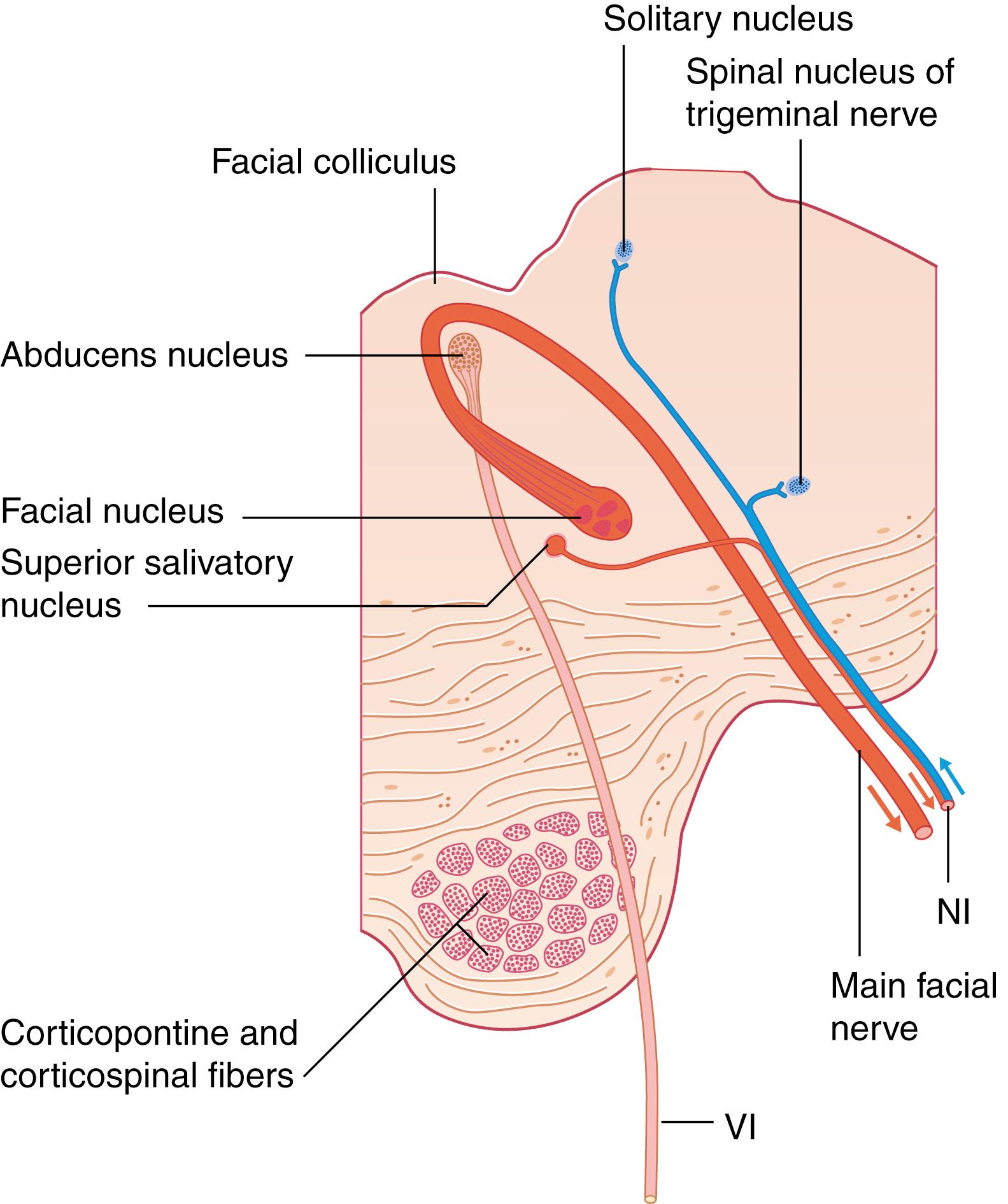
Collectively known as the nervus intermedius , preganglionic fibers of the superior salivatory nucleus and sensory fibers from the nucleus of tractus solitarius exit the brainstem directly lateral to the facial nerve motor root. Together, the facial nerve motor root and nervus intermedius enter the internal auditory canal (IAC) at the porus acusticus. For the purposes of this chapter, the facial motor root and nervus intermedius will be collectively referred to as the facial nerve.
The facial nerve travels through the temporal bone via a bony channel, the fallopian canal . The first segment of the fallopian canal is the meatal segment or IAC. The facial nerve travels in the superior anterior aspect of the IAC. The transverse (falciform) crest separates the facial nerve from the cochlear nerve inferiorly and Bill’s bar, a lateral ridge of bone, and separates the facial nerve from the superior vestibular nerve posteriorly. Within the IAC, the nerve lacks a fibrous sheath or endoneurium and is surrounded by a thin layer of arachnoid.
Exiting the IAC, the facial nerve turns gently anteriorly within the otic capsule bone between the cochlea and superior semicircular canal into the labyrinthine segment. This portion is on average 3 to 6 mm in length—the shortest and narrowest section of the fallopian canal. In this segment, the facial nerve is at its thinnest and particularly vulnerable to injury. The vascular supply is a watershed between the terminal arterioles of the vertebrobasilar system (via the labyrinthine branch of the anterior inferior cerebellar artery [AICA]) and the external carotid artery (via the petrosal branch of the middle meningeal artery). There is also a lack of epineurium vascular plexus along the labyrinthine segment.
At the distal end of the labyrinthine segment, the nerve travels superior to the cochlea and opens into the geniculate fossa. The geniculate fossa is separated from the middle fossa floor by a thin layer of bone, which is dehiscent in about 25% of cases. Here the first fibers leave the facial nerve as the GSPN. The GSPN carries preganglionic parasympathetic innervation to the lacrimal gland and nasal mucosa. These fibers join the deep petrosal nerve from the carotid plexus to become the Vidian (or pterygoid) nerve. The thin bone above the geniculate and anterior attachment of the GSPN exerting intraneural traction place the nerve at increased risk of traumatic injury at this location. After the geniculate fossa, the facial nerve makes an acute posterior and slightly inferior turn, nearly 180 degrees, to enter the tympanic segment or horizontal segment.
The tympanic segment is located along the medial wall of the anterior attic, travels superomedial to the cochleariform process, and forms the superior wall of the oval window niche posteriorly. On average 8 to 11 mm in length, dehiscence of the horizontal fallopian canal occurs in up to 20% of patients, with 80% above the oval window and 12% anterior to the cochleariform process. At the pyramidal eminence, the facial nerve makes a second genu anteroinferior to the lateral semicircular canal and enters the mastoid or vertical segment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here