Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical examination of the upper extremity starts with a detailed and accurate patient history.
Physical examination of the upper extremity consists of inspection, palpation, measurement of length, girth, and ranges of motion, assessment of stability, and detailed assessment of the associated nerve and vascular systems.
Thorough understanding of the anatomy, physiology, and biomechanics of the upper extremity is essential to perform a physical examination correctly and to make a correct diagnosis of pathologic conditions of the upper extremity.
Examiners must master correct physical examination techniques based on the anatomy, physiology, and biomechanics.
The entire upper extremity should be examined, even if the patient's complaint focuses only on the hand.
It is essential to master correct techniques of physical examination to identify the pathologic conditions of patients.
Examiners should have their own routine protocol of examination of the upper extremity so as not to leave a part unexamined.
Comparison of the affected upper extremity with the contralateral unaffected one helps examiners identify pathologic conditions.
Imaging modalities such as X-rays, CT or MRI should be used to confirm the diagnosis drawn from the physical examinations.
Access video content for this chapter online at Elsevier eBooks+ ![]()
The patient history can be the most important tool in developing an accurate diagnosis. The history should not only detail the patient's current complaint, but should also document other elements of the patient's history which may be of great significance for interpreting the patient's current problem and choosing between treatment options. A patient history should include information on the patient's demographics, current complaint, medical history, allergies, medications, and socioeconomic status. The time course of the patient history interview should also be documented.
The patient's name, age, occupation, hand dominance, and hobbies should be documented. Information about previous injuries or diseases should be obtained regardless of whether they seem to be related to the patient's current complaint.
All information on the patient's current problem, including symptoms of pain, numbness, tingling (paresthesia), weakness, dislocation, coldness, clumsiness, or poor coordination and clicking or snapping should be documented. Each symptom should be characterized according to its location, intensity, duration, frequency, radiation and associated symptoms. The patient history should include information on activities or treatments that aggravate or ameliorate the symptoms. It is also important to record the time and place at which the initial injury occurred and the mechanism.
In trauma cases, the following data are especially important:
The time of the injury and the interval between the injury and the patient's presentation should be determined. The interval between an injury and revascularization of amputated fingers has a great effect on the outcome of replantation surgery.
The environment in which the injury occurred is important. Whether an injury occurred in a dirty or a clean environment may determine whether infection is likely to be present.
The mechanism of injury is also important. For example, information on the posture of the fingers and hand at the time of a tendon laceration is helpful for locating a transected tendon stump.
Any previous treatment associated with the injury is documented.
In non-trauma cases, the following data are especially significant:
The time at which symptoms such as pain, abnormal sensation, swelling or stiffness began and the subsequent progression of the symptoms is critical.
The effects of the symptoms on the patient's daily life, hobby or job are unique to that patient.
One must also ascertain whether or not the symptoms are limited to one part of the body.
Activities or postures that aggravate or ameliorate the symptoms are also discussed.
The association between time and the intensity of symptoms must be carefully documented (e.g., whether pain increases just after waking up in the morning or during the night).
The patient's health status may influence diagnosis and treatment. Before starting treatment, it is essential to determine whether the patient has diabetes, or cardiac, pulmonary, and/or renal disease and whether the patient has a history of rheumatologic disease. Documentation of the family's medical history may be helpful for making an accurate diagnosis and for choosing an appropriate treatment if the disease is hereditary. Patients and their families should be questioned about previous problems associated with bleeding and anesthesia. It is also important to determine the course of any prior surgery.
The patient history should include data on any medications that the patient is taking. Previous allergic reactions to foods or medications should be noted. People who are allergic to shellfish are often allergic to contrast media that contain iodine.
The social history includes the patient's use of tobacco and alcohol. The amount of tobacco and alcohol used should be documented. Substance abuse and infection with hepatitis virus or human immunodeficiency virus (HIV) should also be noted. The patient's hobbies or sports should be documented because these activities often determine the most appropriate treatment.
Accurate diagnosis of hand problems depends on a systematic, careful physical examination. Physical examination should be performed routinely following a specific protocol. Even if the patient complains of a problem limited to the hand, the physical examination should start at the neck and shoulder region because the hand is suspended by the bones of the forearm, which connect proximally to the elbow joint, which in turn is stabilized by the humerus and the shoulder joint. In addition, numbness of the hand may be associated with cervical problems. These elements (inspection, palpation, measurement of range of motion, musculotendinous assessment, stability assessment, nerve assessment, and vascular assessment) should be included in the examination procedure for patients with problems of the upper extremities. An understanding of the interrelationships among these elements is helpful for drawing accurate diagnostic conclusions. Repeated physical examinations reveal how symptoms change over time, which is important for assessing the effectiveness of the treatment.
When inspecting the upper extremities, it is essential to compare the affected extremity with the contralateral extremity because the latter can be used as a normal reference if the injury is unilateral.
An abnormal skin color or a change in the color of the skin of the upper extremity is indicative of a wide variety of problems. Infections often cause swelling and patches of redness with proximal streaking. Vascular problems caused by arterial inflow insufficiency often present as pale-colored and the distal part of the upper limb appears to have shrunk, whereas those caused by venous outflow insufficiency present as a purple or dark red discoloration and a swollen limb. The color of a hematoma can be used to estimate the interval since the trauma occurred. A fresh hematoma has purple or blue patches, which then become green and finally yellow.
Fractures, tumors, arthritis, and some infectious conditions can cause deformities of the upper extremity. Fractures of the phalanges of the fingers frequently result in angular rotation or malrotation of the fingers. When the fingers are held up, the point at which the long axes of the fingers converge corresponds with the position of the scaphoid tubercle. However, the long axis of a malrotated finger deviates from the position of the scaphoid.
It is important to determine whether atrophied muscles are innervated by specific peripheral nerves. If the atrophic muscles are innervated by a specific nerve, the atrophy may have been caused by a peripheral nerve disorder. Muscular atrophy may occur under systemic neural or muscular pathological conditions; in most of these cases, the atrophy is symmetrical in the bilateral extremities. Generally, neurogenic diseases involve muscles in the distal part of the extremity and muscular diseases involve the proximal part of the extremity. The girths of the arm (a portion measured should be noted, like the arm girth 20 cm distal to the acromion) and forearm (a portion with the maximum diameter of the forearm) of both upper extremities should be measured routinely because this often reveals a loss of muscle mass, which may not be obvious to the eye.
Trophic changes are associated with an abnormality of the sympathetic nervous system. Increased hair growth or abnormal perspiration of the hands is often observed in chronic regional pain syndrome.
Swelling can be identified by comparison with the uninvolved extremity. Localized swelling indicates recent trauma or inflammation. Diffuse swelling is often caused by infection. General swelling may originate from a lymphatic or venous obstruction. Swelling of the dorsum of the hand is also common.
Disappearance of skin creases is indicative of loss of motion of the joint under the creases and can be helpful in determining the validity of a complaint of an inability to move the fingers or upper extremities. Clear finger creases over joints that a patient claims he or she is unable to flex or extend indicate that the patient moves the joint. In such cases, the patient may be malingering or may have a psychiatric condition in which he or she cannot recognize motion of the joint.
Palpation is a powerful maneuver for identifying masses, abnormal skin temperature, areas of tenderness, crepitance, clicking or snapping, and effusion. Masses in the deep layer can be detected by palpation before they emerge as masses under the skin. When performing palpation, special attention should be paid to differences in hardness or mobility relative to that of the surrounding tissue. For example, subtle palpation can identify a palmar bowstring of a flexor tendon in a patient who complains of lack of finger flexion after an injury of the flexor pulleys.
The integrity of the tendon and the strength of the muscle should be considered when conducting a musculotendinous assessment.
When musculotendinous units are examined, it should be kept in mind that the muscle strength and ranges of motion of the hand and digits change depending on the posture of the wrist, forearm or digits. For example, the range of motion of the distal interphalangeal (DIP) joint of a finger is less when the proximal interphalangeal (PIP) joint is passively extended than when the PIP joint is flexed.
Both passive and active ranges of motion should be documented. The range of motion of both the contralateral healthy limb and the affected limb should be measured and compared. The range of motion may be affected by the posture of the adjacent joints. For example, active and passive distal interphalangeal (DIP) joint flexion is limited when the proximal interphalangeal (PIP) joint of the same finger is extended. When the wrist joint is flexed, the active range of finger flexion decreases. The range of motion of a joint should be measured in a posture that permits maximum motion.
The passive range of motion is measured by holding proximal and distal to the joint in question and then moving the joint from one limit of motion to the other in the absence of any muscular contraction by the patient. A limited range of passive motion is associated with joint stiffness and/or soft-tissue contracture.
The active range of motion of a joint is that which occurs when the patient contracts his or her muscles. The active range of motion is affected by tendon excursion, the posture of the hand and fingers, nerve function, and muscular strength.
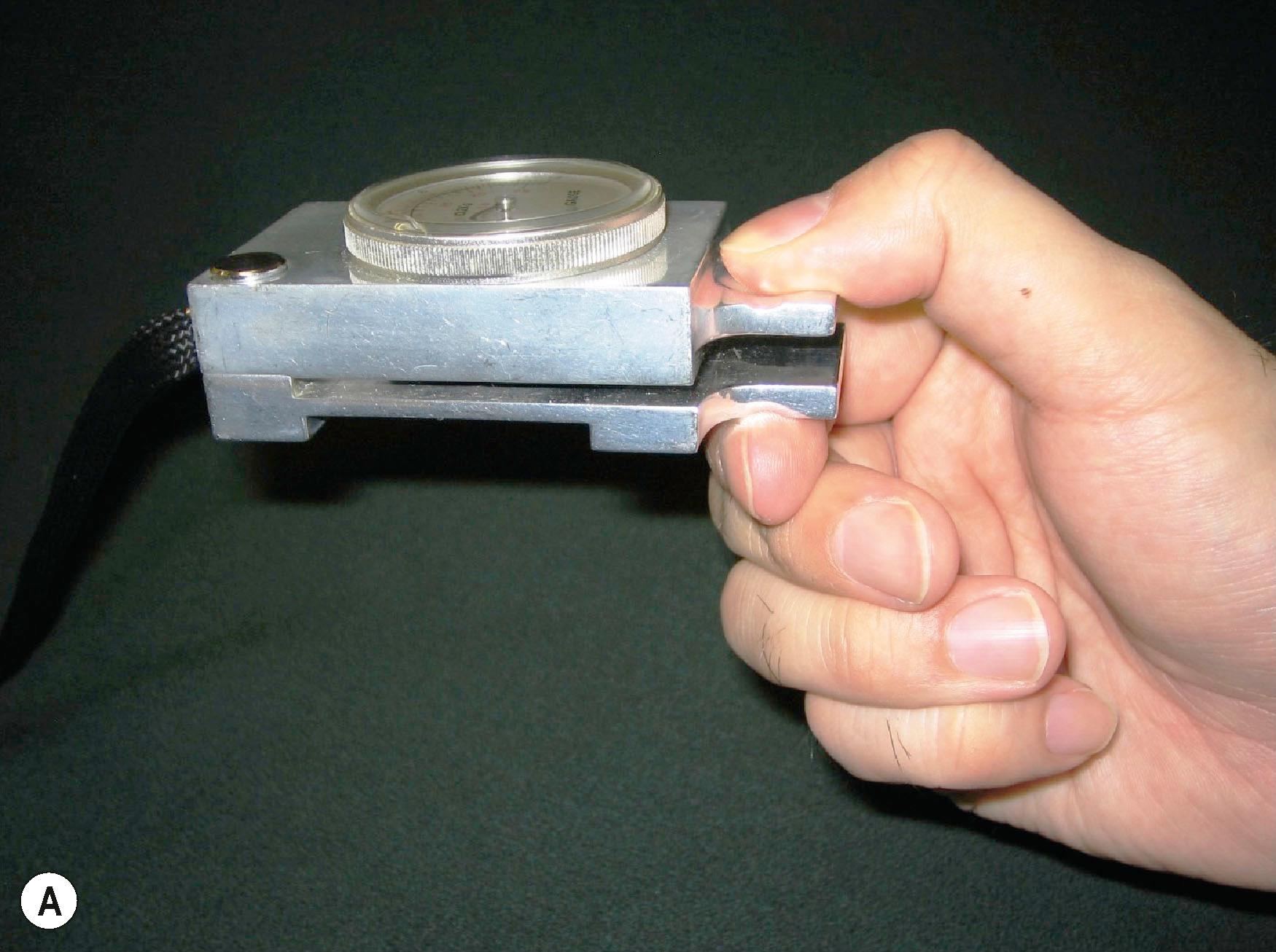
Muscle power is classed according to the Medical Research Council scale, which ranges from zero to five (0–5) ( Table 2.1 ). Grip strength is a good indicator of the global muscle strength of the upper extremity. Grip strength is measured using a dynamometer with the shoulder and elbow joints stabilized. The patient grips the dynamometer with the elbow straightened beside the trunk in the standing position or flexed 90° in the sitting position. Measurement of pinch grip strengths includes the average of three grip strength trials on the affected and unaffected hands using a Jamar pinch gauge in two different postures. These include a lateral pinch grip measured between the thumb pulp and the radial aspect of the second digit, and a thumb–forefinger pinch grip measured between the tips of the thumb and forefinger ( Fig. 2.1 ). For both grips, the shoulder is adducted and neutrally rotated, and the forearm and wrist are in a closely neutral and comfortable position.
| Grade | Physical examination findings |
|---|---|
| 0 | No contraction |
| 1 | Flicker or trace contraction |
| 2 | Active movement with gravity eliminated |
| 3 | Active movement against gravity |
| 4 | Active movement against gravity and resistance |
| 5 | Normal power |
There are many muscles and tendons in the hand. Muscles, the origin and insertion of which are both distal to the wrist joint, are called intrinsic muscles. Muscles extending across the wrist joint are called extrinsic muscles. Other muscles often compensate for a nonfunctioning muscle, in which case the nonfunctioning muscle appears to function. To evaluate muscle function, each muscle should be evaluated in a posture or situation in which the cooperative muscles do not function. For example, the extensor pollicis longus (EPL) can compensate for impaired thumb adduction. Even when the thumb adductors do not function because of ulnar nerve palsy, patients may be able to adduct the thumb using a functional EPL.
The presence of abnormal muscles or an abnormal linkage of tendons should sometimes be considered. The flexion function of the PIP joint of a finger is generally accepted to be independent of that of the other fingers because the flexor digitorum superficialis (FDS) tendon of each finger has its own muscle belly. The motion of the FDS tendon of the small finger is often linked to that of the ring and/or the long finger and the PIP joint flexion of the small finger often coordinates with that of the ring and/or long fingers. The extensor digitorum manus brevis is sometimes present in the middle finger and causes dorsal wrist pain.
The flexor digitorum profundus (FDP) tendons insert on the palmar surface of the distal phalanx of the fingers. Because the FDP muscles share a common origin, holding the DIP joint of a finger in full extension may prevent motion of all FDPs.
Purpose : This test is used to assess the continuity, excursion, and muscle power of each of the FDP tendons.
Maneuver : The patient's hand is placed palm up on a table. The examiner presses down on the proximal and middle phalanges of the target finger to keep the metacarpophalangeal (MCP) and PIP joints in extension and asks the patient to flex the DIP joint. The test should be performed on each finger.
The flexor digitorum superficialis (FDS) tendons insert on the proximal half of the palmar surface of the middle phalanx of the fingers. Because each FDS tendon has its own muscle belly, its function is independent of the FDS of the adjacent fingers.
Purpose : This test is used to assess the continuity, excursion, and muscle power of each of the flexor digitorum superficialis tendons.
Maneuver : The patient's hand is placed palm up on a table. The examiner presses down on the distal phalanges of all fingers except that of the finger to be tested to keep the MCP, PIP, and DIP joints of the other fingers in full extension. The patient is then asked to flex the finger to be tested. Each finger is tested individually. The FDS moves when the other fingers are kept fully extended.
The flexor pollicis longus (FPL) inserts on the palmar surface of the distal phalanx of the thumb and can be tested by asking the patient to flex the interphalangeal (IP) joint of the thumb.
Purpose : To evaluate the continuity and excursion of the extrinsic flexors of the thumb and fingers. This test and the dynamic tenodesis test ( ![]() ) are useful for distinguishing nerve palsy from tendon rupture.
) are useful for distinguishing nerve palsy from tendon rupture.
Maneuver : The patient is asked to place the dorsum of the forearm and the hand on a table and to relax. The examiner pushes down on the musculotendinous junctions of the flexor tendons around the palmar aspect of the mid-forearm. If the tendons have normal excursion and no adhesions, the fingers and thumb flex as the forearm is pushed down.
The extensor pollicis brevis (EPB) inserts at the dorsal base of the proximal phalanx of the thumb. It is sometimes connected to the EPL. The abductor pollicis longus (APL) has several tendon slips and inserts at the dorsolateral base of the thumb metacarpal and trapezium. Both tendons pass through the first dorsal compartment at the wrist (the APL tendon lies radial to the EPB in the compartment). Because the EPB is a phylogenetically new muscle, it often shows extremely poor development or even complete absence. The number of the APL tendon slips is usually greater when the EPB is absent than that when the EPB is present. When the patient abducts the thumb maximally, the EPB and APL tendons as well as the EPL tendon merge under the skin over the radiodorsal side of the wrist and create the snuffbox. The EPB and APL tendons are palpable as taut tendons in the radiopalmar border of the snuffbox. The tendinitis of the EPB and APL at the radial wrist level is known as de Quervain's tenosynovitis. There are two provocative tests for diagnosing de Quervain's tenosynovitis.
Purpose : To detect de Quervain's tenosynovitis.
Maneuver : The patient places the hand on a table with the thumb up. The examiner pushes down on the proximal phalanx of the thumb. A patient with de Quervain's tendinitis will experience pain or discomfort in the first extensor compartment of the wrist.
Purpose : To detect de Quervain's tenosynovitis.
Maneuver : The patient is asked to hold the thumb with the four flexed fingers of the affected hand. The hand is deviated ulnarly by the examiner. A patient with de Quervain's tenosynovitis will experience pain or discomfort in the first extensor compartment of the wrist.
The extensor carpi radialis longus (ECRL) and brevis (ECRB) tendons insert at the dorsal bases of the second and third metacarpal bones, respectively. The function of these muscles is to extend the wrist joint. Because the functional axis of the ECRL deviates radially, the ECRL extends the wrist dorsoradially. When the ECRB does not function, extension of the wrist deviates radially because of the intact ECRL tendon. The extensor digitorum communis (EDC) tendon also may function as a wrist extensor. To remove the EDC contribution to wrist extension, the patient is asked to make a fist and then extend the wrist. Making a fist eliminates EDC function.
The extensor pollicis longus (EPL) passes through the third dorsal compartment, turns radially at the Lister's tubercle and inserts at the dorsal base of the distal phalanx of the thumb. The EPL extends the IP joint of the thumb. The hand is placed palm down on a table with the thumb adducted. The patient is asked to lift only the thumb off the surface of the table, keeping the thumb adducted. The taut EPL tendon is palpable in the radiodorsal aspect of the wrist.
The EPL tendon is often connected to the extensor pollicis brevis (EPB) tendon. Although the EPL tendon is not functioning, the thumb IP joint can be extended by means of the force of the EPB tendon. When examining EPL function, one must eliminate EPB function by stabilizing the thumb MCP joint.
The extensor digitorum communis (EDC) tendons pass through the fourth extensor compartment and insert at the dorsal base of the middle phalanges of the fingers. They mainly extend the MCP joint, while the intrinsic extensors extend the PIP and DIP joints. EDC function is examined by asking the patient to lift the MCP joints of four fingers (the index to the small finger) keeping the PIP and DIP joints flexed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here