Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A painful, stiff shoulder is an undesired but not uncommon complication following rotator cuff repair. Postoperative shoulder stiffness, commonly known as POSS, is an “acquired” condition, and several authors have defined it in various ways, depending on the patterns of motion loss with a stabilized scapula. Simply put, it is a persistently painful, stiff shoulder 6–12 weeks following a rotator cuff repair, and this includes loss of both active and passive range of motion (ROM), particularly abduction, forward flexion, and external rotation. Recovery is seen in most cases by 6 to 24 months with appropriate rehabilitation. Incidence varies from 0 to 32.7% following open, miniopen, or arthroscopic repair. Age, diabetes mellitus, tendency for keloids, preexisting stiffness, personality of the patient, complex regional pain syndrome, rehabilitation compliance, and delay between cuff tear and repair surgery are the factors described in the literature as possibly contributing to POSS.
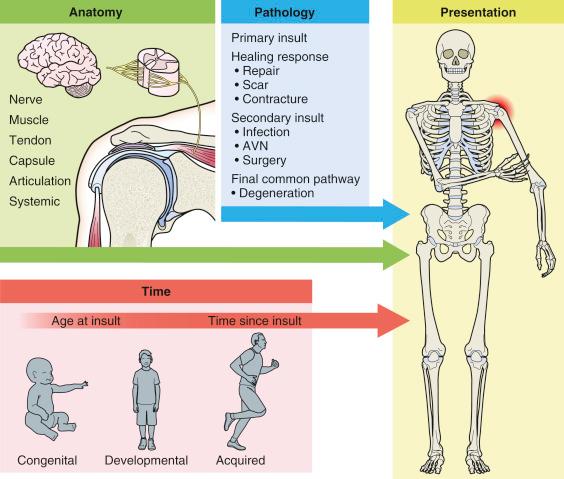
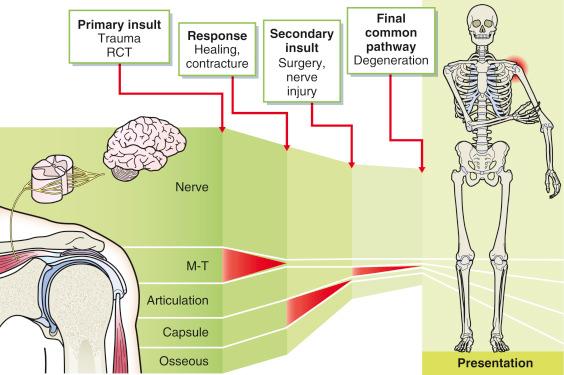
Reduced joint motion is the result of pathological changes to normal structures. The outcome of these changes varies with time. The pathological processes that lead to a shoulder contracture are dependent on the premorbid state, the initial insult, and the response to this insult over time ( Figs. 34.1 and 34.2 ). Therefore anatomical, pathological, and time aspects must all be assessed.
Tailored rehabilitation protocols remain a mainstay of treatment. Corticosteroids can be used in those cases in which there is persistent pain after at least 6 months but where there is good rotator cuff strength. In our opinion, manipulation under anesthesia (MUA) should not be performed, owing to the risk of tendon repair retear. Second-look arthroscopy can be performed, which allows assessment of the rotator cuff repair, adequacy of subacromial decompression, and identification of capsular contractures. Release of the contractures can be performed.
It is important to consider the differential diagnosis of the patient who has a persistent painful, stiff shoulder after a previous rotator cuff repair ( Table 34.1 ). It is important to identify whether the patient falls within part of the normal spectrum of healing of a rotator cuff or whether there are some other factors that demonstrate that the patient has a complication of surgery.
|
In principle, the pain and stiffness can be:
A normal part of the recovery of surgery or
A preexisting pathology that was overlooked
Those cases that require urgent assessment include those with an infection. Other cases that may require surgical intervention include those for which the tendon has failed to heal, where there is failure of implant fixation, and/or those involving retear of the tendon. All of these are likely to present with symptoms suggestive of weakness of the rotator cuff structures. Other, less common complications include deltoid weakness due to surgical release of the deltoid as part of an open exposure. Failure of the deltoid repair can be a significant problem. Another cause of deltoid weakness can be axillary nerve palsy, in which case there is likely to be associated paresthesia in the axillary nerve distribution. It is not uncommon for patients with diabetes or other general medical conditions to develop a “secondary frozen shoulder” following rotator cuff repair. Other pathologies that may have been present prior to the initial surgery include acromioclavicular joint arthrosis, subacromial bursitis, calcific tendonitis, and biceps tendonitis. Iatrogenic causes of pain and stiffness include irritation from the sutures or suture anchors in the subacromial space. Acromial fracture could theoretically occur from an overzealous acromioplasty.
Finally, other causes of shoulder pain that are well described can occur incidentally despite the previous repair. This includes conditions such as referred pain from the neck from a disc prolapse, brachial neuritis, and polymyalgia rheumatica. Even patients with carpal tunnel syndrome can experience referred pain to the shoulder. There can be other local causes of pain in the shoulder, such as bicipital tendonitis, subacromial bursitis, and acromioclavicular joint arthrosis. To ensure the correct management of the patient who has a persistent painful shoulder, it is important to identify the correct cause of the pain, which in some clinical situations can be difficult.
Persistent painful shoulder provoked by movement following rotator cuff repair after more than 12 weeks postoperatively. Pain typically described as constant, often worse at night, and may be refractory to oral analgesics.
Age, diabetes mellitus, tendency for keloids, delay between initial cuff tear and repair surgery, and preexisting stiffness.
Personality of the patient, rehabilitation compliance.
Any history suggestive of infection or reaction to the implant should be obtained (fevers, wound erythema or discharge).
A history of fall, strains, or sudden loss of function following the surgery may suggest retear.
Inspection: swelling, redness, healing of scars, wasting of rotator cuff or deltoid
Palpation: tenderness, warmth
Strength of cuff function
Loss of both active and passive ROM, particularly abduction, forward flexion, and external rotation
Pain at the extremes of motion. Failure to heal or retear.
Assessment of sensation (suprascapular and axillary nerve)
X-rays: acromion–humerus distance, acromial morphology.
Infection suggested by lysis around implant, progressive loss of joint space, erosion of the humeral head and/or glenoid.
Deltoid failure/axillary nerve palsy: inferior migration of the humeral head.
Implant failure: anchor floating freely in the subacromial space.
Acromial fracture or greater tuberosity fracture.
Sclerosis and joint space narrowing suggest osteoarthritis.
MRI to evaluate implant location and orientation and to assess cuff repair, subacromial bursitis, and capsular contracture.
Blood tests, including complete blood count, erythrocyte sedimentation rate, and C-reactive protein, mainly to rule out infection.
Blood glucose levels and Hb1AC to assess for diabetes.
Electromyography for assessment of denervation of deltoid or rotator cuff.
The mainstay of treatment is physiotherapy.
Corticosteroids could be used in those cases in which there is persistent pain after at least 6 months, with good rotator cuff strength.
Second-look arthroscopy can be performed, which allows for assessment of the rotator cuff repair, adequacy of subacromial decompression, and identification of capsular contractures. Release of the contractures can be performed.
If there is any history of infection, it is important to obtain a microbiological diagnosis. We usually perform arthroscopy of the shoulder and obtain biopsies under direct inspection. Matched specimens are harvested so that histologic and microbiologic results can be determined.
If the patient has had a failure to heal, then secondary reconstructive surgery is unlikely to be effective. In some cases, we have used a hamstring graft to act as a bridging graft to supplement the constructs. Other cases require a reverse total shoulder replacement to be performed.
In our opinion, MUA should not be performed, owing to the risk of tendon repair retear.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here