Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Inward deviation of the visual axes, with an onset before 6 months of age.
Esotropia greater than 30Δ present before 6 months.
Cross-fixation.
Little or no binocular vision.
Normal refractive error for age.
Initially, similar deviation at distance and near fixation.
Inferior oblique overaction.
Dissociated vertical deviation.
Fusion maldevelopment nystagmus (formerly known as latent nystagmus ).
Amblyopia in about one-third of patients.
Inward deviation of the visual axes caused by high hyperopia or a high ratio of accommodative convergence to accommodation, or both.
Initially intermittent acquired esotropia.
Esotropia larger at near than distance fixation.
Typical age of onset usually between 18 months and 3 years.
Typically hyperopic, but patients who have a high ratio of accommodative convergence to accommodation may have any refractive error.
Congenital miswiring of the medial or lateral rectus muscles or both.
Retraction of the affected globe(s) on attempted adduction.
Limitation of abduction, adduction, or both.
Abnormal head posture.
Present from birth; however, often noticed later in infant/toddler years.
Elevation (upshoot) or depression (downshoot) of the globe on attempted adduction.
Esotropia (or exotropia in some patients), rarely larger than 30°.
Esotropias represent the most common form of strabismus and include infantile, accommodative, cyclic, and nonaccommodative forms. They also are seen more frequently in children with neurological impairment or vision deficit (sensory esotropia) and in some patients who have Duane's and Moebius' sequence, cranial nerve VI palsy, and thyroid disease–associated strabismus.
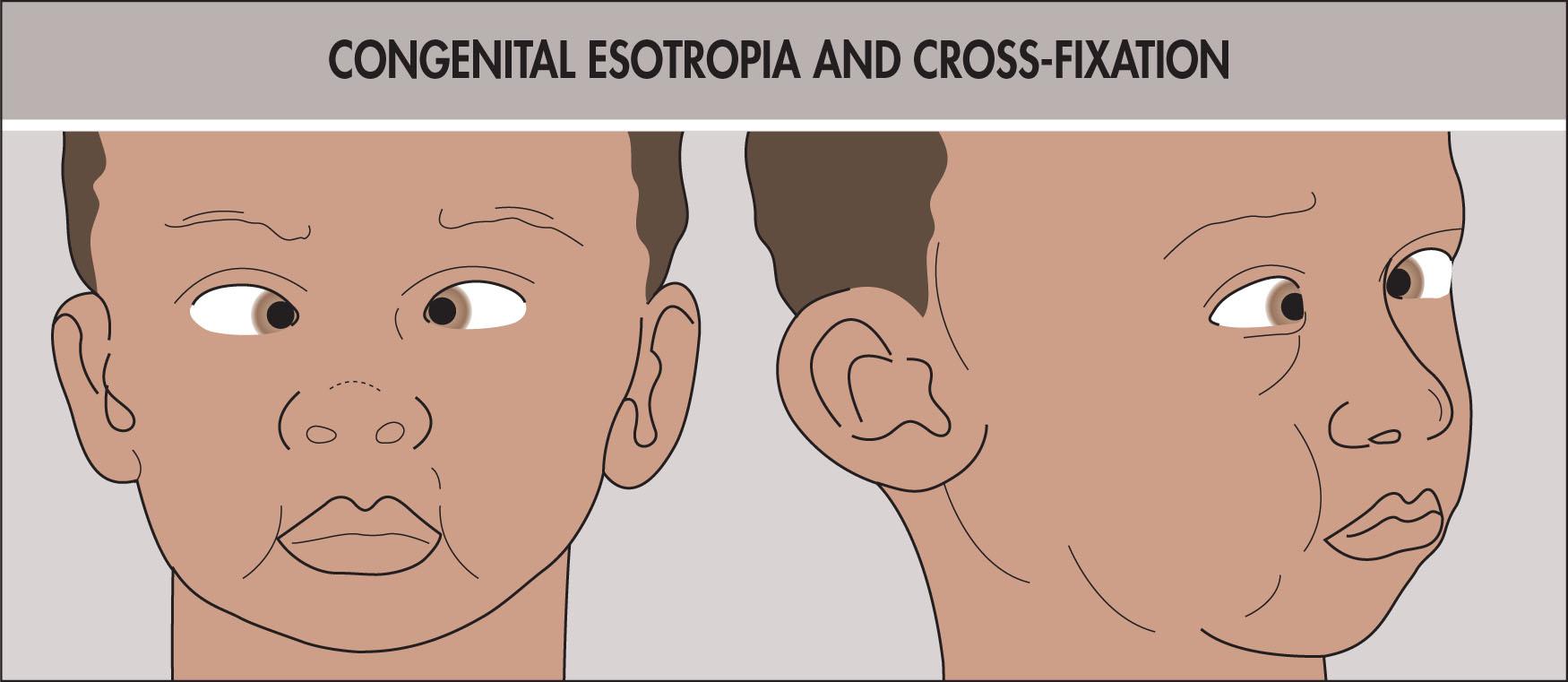
Infantile esotropia (previously termed congenital esotropia ) is defined as esotropia that presents before 6 months of age ( Fig. 11.6.1 ). Congenital esotropia is a misnomer because in very few cases, if any, are children esotropic at birth. Many normal infants will have an intermittent eso- or exotropia, which is thought of as developmental and disappears between 2 and 4 months of age. Prospective studies have determined that this is the age at which infantile esotropia is first noted. For younger infants, it cannot be predicted which ones will develop infantile esotropia by age 2–4 months.

The incidence of infantile esotropia is roughly 1% in most series and may be more common in children who have neurological disorders. Sex and racial distributions are equal. Concordance in one series was 81% in monozygous twins and 9% in dizygous twins. It is common to find some form of strabismus in other members of the proband’s family.
Amblyopia occurs in 25%–40% of patients, but the majority “cross-fixate,” that is, use the right eye to fix across the nose to view objects to the left of the patient, and vice versa ( Fig. 11.6.2 ). A child who does not have amblyopia switches fixation at the midline as an object is brought from one side to the other. This phenomenon might cause the examiner to believe there is a true abduction deficit and pursue an unnecessary workup for “cranial nerve VI palsy.” In most cases, however, when one eye is covered, full abduction can be elicited in the uncovered eye. The doll’s head maneuver is helpful to demonstrate true abduction ability. As a general rule, the deviation is >30Δ and comitant, measuring roughly the same in all gaze positions, distance and near.
Inferior oblique involvement is noted in up to 75% of patients, with an onset most frequently during the second year of life; it may be unilateral or bilateral ( Fig. 11.6.3 ). Early surgical correction of the esotropia does not prevent the later development of inferior oblique involvement. This must be differentiated from dissociated vertical deviation (DVD), which also occurs in roughly 75% of these patients and has similar onset patterns ( Fig. 11.6.4 ) ; DVD may be manifest or latent, can be very asymmetrical, and may present as any combination of slow elevation, abduction, and excyclotorsion ( Box 11.6.1 ). Less commonly, the dissociated abduction is more prominent than elevation, and in that case, it is termed dissociated horizontal deviation (DHD). A dissociated torsional deviation (DTD) can be seen as a few nystagmus beats. Although its cause is unknown, DVD may represent a primitive eye-movement pattern uncovered by deficient fusion.


| Dissociated Vertical Deviation | Inferior Oblique Overaction |
|---|---|
| Present in all gaze positions | Present in adduction only |
| Does not obey Hering’s law | Obeys Hering’s law |
| Slow floating abduction, elevation, excyclotorsion movement | Rapid elevation, abduction movement |
| Not associated with A or V pattern | Often associated with V pattern |
Fusion maldevelopment nystagmus (FMN), formerly known as latent nystagmus , with a fast phase toward the unoccluded eye, is found in approximately 50% of patients.
Asymmetrical monocular pursuit is a feature of infantile esotropia, as measured by opticokinetic nystagmus (OKN). Temporal-to-nasal pursuit is favored; patients who have infantile esotropia show poor nasal-to-temporal OKN, regardless of the degree of stereopsis or the timing of surgery.
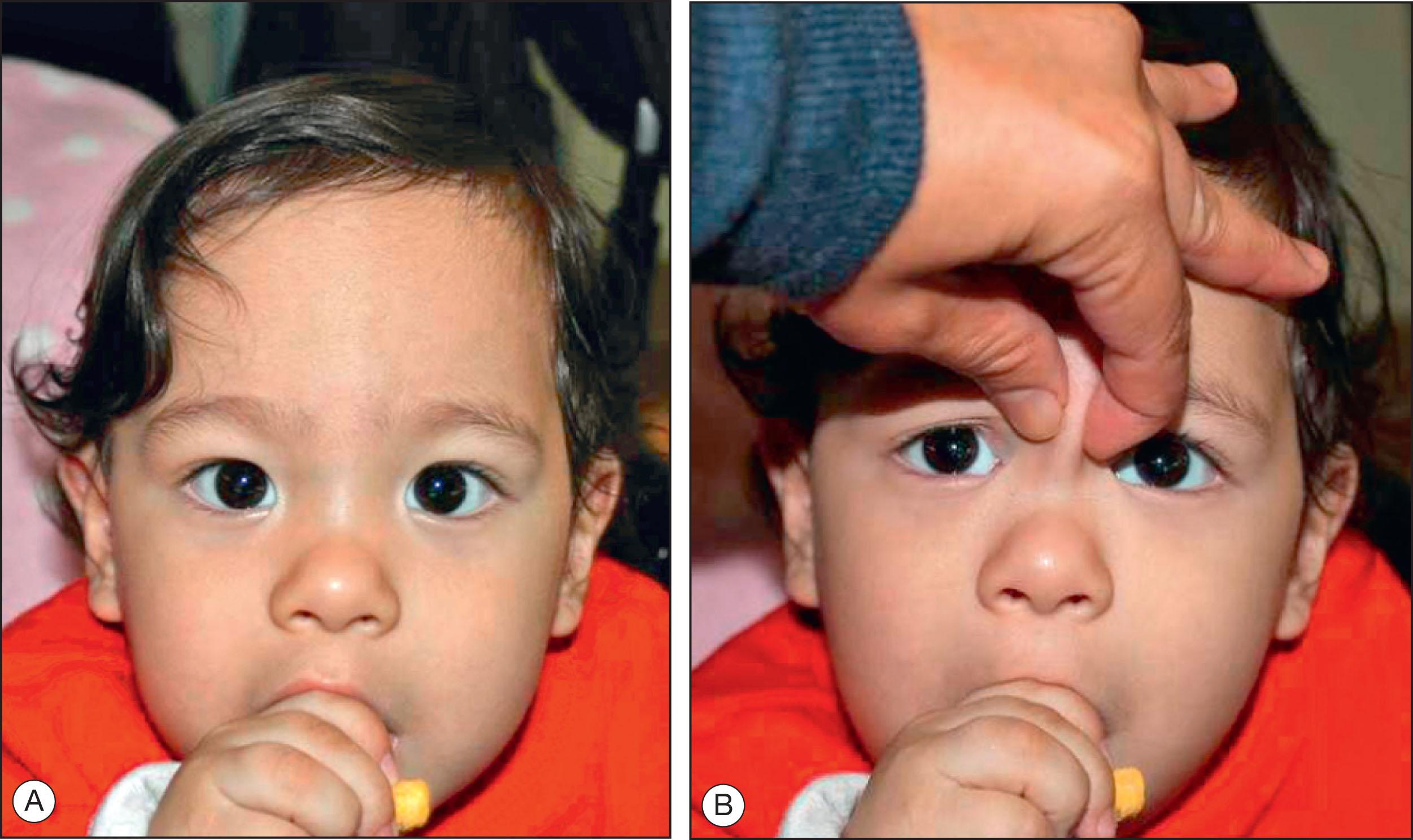
Roughly half of young children sent to ophthalmologists by pediatricians for esotropia have pseudostrabismus, an illusion caused by a wide and flat nasal bridge, wide epicanthal folds, and the ability of young children to converge to very close distances ( Fig. 11.6.5A ). In the Asian population, where a flat nasal bridge and wide epicanthal folds are more common, pseudoesotropia is more likely. A recent study found that the positive predictive value of referral for infantile esotropia in children of Chinese descent was only 5.9% (as opposed to 36% in non-Chinese children).
Cover test measurements to measure the angle of strabismus may be difficult in very young children. The light reflex tests (Hirschberg and Krimsky) are easier to perform in infants. A variation of the light reflex test in which the deviation is neutralized by prisms held apex to apex before both eyes may be required if the angle of strabismus is very large. The deviation tends to be constant but may vary; spontaneous resolution may occur if the deviation is small (<40Δ) or intermittent. Refractive errors tend to be similar to those of normal children of the same age.
In older children with surgically corrected or uncorrected infantile esotropia, FMN may confound attempts at monocular acuity measurement; fogging one eye with plus lenses, a translucent occluder, or the use of anaglyph (red–green) lenses may provide a more accurate acuity measurement in the face of FMN.
Side-gaze observations by nonophthalmologists may be particularly deceptive in the case of pseudostrabismus because the adducted eye is buried easily under the skin fold. Hirschberg's light reflexes may demonstrate alignment to parents, as can elevation of the nasal bridge skin away from the face to alter the facial appearance temporarily (see Figure 11.6.5B ).
The differential diagnosis of infantile esotropia ( Box 11.6.2 ) includes the entities discussed in detail later. The nystagmus blockage (compensation) syndrome, in the opinion of some investigators, accounts for a significant segment of the young population with large-angle, early-onset esotropia. These patients have a large esotropia and nystagmus at a young age. The nystagmus is of minimal amplitude in adduction and maximal in abduction. Therefore the patient makes a continuous effort to maintain both eyes in adduction through the use of convergence, and it may be impossible to neutralize the esodeviation using prisms held before one or both eyes. This is in contrast to nystagmus associated with the common form of infantile esotropia, which presents in equal degrees in all gaze positions. Various series imply that nystagmus blockage syndrome affects 10%–12% of patients with infantile esotropia, but many investigators believe that it is much less common. Cranial nerve VI palsies need to be considered in the transient newborn form, which often resolves spontaneously over a few days or weeks, as well as the more common acquired postviral or postimmunization form.
Early-onset accommodative esotropia
Nystagmus blockage (compensation) syndrome
Moebius’ sequence
Duane’s syndrome
Congenital cranial nerve VI palsy
Cyclic esotropia
Esotropia associated with visual loss in one eye (sensory esotropia)
Neurological impairment
Strabismus fixus and other fibrosis syndromes
The theoretical goals of treatment include the following:
Excellent visual acuity in each eye
Perfect single binocular vision in all gaze positions at distance and near
A normal esthetic appearance
All are obtainable except for perfect single binocular vision because (with rare exceptions) these patients, even with early treatment, do not view with both foveae simultaneously. However, as discussed later, most obtain peripheral fusion with the monofixation syndrome and generally stable alignment. Other reported benefits of successful surgical alignment include improvement in fine motor skills, heightened bonding of parents and child, and enlarged binocular visual field.
Amblyopia traditionally is treated preoperatively for multiple reasons: (1) compliance is usually better because families are more motivated when they can see the strabismus, (2) visual behavior may be evaluated more easily (the eye moves to take up fixation in the presence of a large strabismus), (3) amblyopia responds more quickly in a younger child, and (4) postoperative occlusion treatment would interfere with the potential development of binocularity. Amblyopia associated with infantile esotropia seems amenable to treatment, and with the appropriate optical correction and occlusion therapy adjusted throughout the first years, 20/20 vision can be achieved in most patients. The impact of treatment of refractive errors of less than +2.00 D usually is variable and minimal. Larger refractive errors are corrected, and the deviation is remeasured, because postoperative exotropia may occur if surgery is performed on uncorrected, highly hyperopic eyes, denoting a possible accommodative component.
When infantile esotropia is left untreated, patients do not display binocular vision of any variety when they become old enough to cooperate for testing of their visual sensory status; the primary goal of surgical treatment at this age is to align the eyes sufficiently to stimulate the development of binocularity. This binocularity usually fulfills the criteria for monofixation syndrome as defined by Parks and is generally a stable alignment. The work of Drs. Birch and Ing revealed that the time windows during which stereopsis and fusion develop are during the first year and second year of life, respectively. This binocular function timeline favors early surgical correction. Some studies suggest that surgical correction by the age of 1 year is more effective than that performed later. A recent study by Yagasaki et al. showed that some stereopsis response was present in 96% of patients with infantile esotropia operated at 8 months of age or earlier. Some even suggest very early surgical correction (at the age of 2–4 months) in order to develop better binocularity. However, this is typically difficult because most patients do not present this early to a strabismus specialist.
Advocates of surgery after 2 years of age are concerned about the later development of inferior oblique overaction and DVD, which require separate surgical procedures, and the difficulty of measuring acuity in children who have aligned visual axes. They also are unconvinced of the benefits of the monofixation syndrome (peripheral fusion without central fusion). Given reproducible strabismus measurements, informed and supportive parents, the availability of safe pediatric anesthetic, and the absence of amblyopia, most strabismus surgeons in the United States opt for attainment of horizontal alignment during the first year of life.
Most ophthalmologists in the United States will choose symmetrical medial rectus recessions on both eyes (possibly adding a monocular or binocular lateral rectus resection or plication for very large deviations). However, monocular surgery is often preferred when one eye has poor vision to avoid the risk of surgical complication in the good eye. Monocular surgery is typically recession of the medial rectus and resection or plication of the ipsilateral lateral rectus. Some surgeons prefer a limbal incision because of the ease of access and orientation, as well as the ability to recede contracted conjunctiva and thus augment the effect of the medial rectus recession. Many prefer the fornix approach popularized by Parks because it avoids proximity to the cornea, enabling rapid patient mobilization. It may also have better early cosmesis. Some surgeons prefer to perform recessions measured from the limbus rather than the original muscle insertion because of increased uniformity and better results. A common protocol for surgical treatment is given in Table 11.6.1 . There may be some variability in certain patient populations. Recently, Park and Oh found that in preterm infants with infantile esotropia, the overcorrection rate was greater than in full-term children, even though the extent of surgery was reduced by 0.5 mm per muscle in preterm patients.
| Deviation a (Δ) | Symmetrical | Asymmetrical (one eye) | |
|---|---|---|---|
| Recess Medial Rectus, Both Eyes (mm) | Resect Lateral Rectus (mm) | Recess Medial Rectus (mm) | |
| 30 | 4.5 | 5.5 | 4.5 |
| 35 | 5.0 | 6.0 | 5.0 |
| 40 | 5.5 | 6.5 | 5.5 |
| 50 | 6.0 | 7.0 | 6.0 |
| 60 | 6.5 | 7.5 | 6.5 |
| 70 | 7.0 | 8.0 | 7.0 |
a There are many surgical dosage tables. This one is commonly used around the world.
Another approach to infantile esotropia is the use of botulinum toxin, originally popularized by Scott. A retrospective study comparing botulinum toxin to surgical bilateral medial rectus recession for esotropia in patients younger than 2 years found that no statistically significant difference occurred in terms of alignment and stereopsis between the groups. Advocates of botulinum toxin argue that reduced anesthesia time gives it a distinct advantage. However, many patients require more than a single injection, and because anesthetic risk primarily occurs during induction and emergence, this advantage may evaporate. Some surgeons suggest the use of botulinum toxin injections as a measure to augment the effect of standard surgery in cases of large-angle esotropia. Potential side effects from the toxin, such as ptosis, consecutive exotropia, and the induction of vertical strabismus, are to be considered because these young patients are in the amblyogenic age range.
Patients with DVD usually exhibit no binocularity when DVD is present. The treatment of DVD is generally surgical. This can be symmetrical or asymmetrical and may involve significant recessions of the superior rectus muscles or inferior oblique muscles in the presence of inferior oblique overaction. When there is inferior oblique overaction, the most common inferior oblique–weakening procedures are myectomy and recession. For mild cases, some recommend a “z” myotomy. Anteriorization of the oblique insertion to the margin of the inferior rectus significantly weakens the muscle and may be an effective treatment for simultaneous DVD. Clear separation between DVD and inferior oblique overaction is necessary, however, because weakening of a normally functioning inferior oblique muscle may cause limitation of elevation in adduction, compensatory head postures, and all the signs and symptoms of cyclovertical muscle palsy.
Children who have surgery for infantile esotropia require long-term follow-up because of the possible development of DVD, inferior oblique overaction, FMN, and amblyopia. The optimal result is alignment within 8Δ of orthophoria. Residual esotropia of >10Δ found 4–6 weeks after initial surgery may respond to antiaccommodative measures if the patient is significantly hyperopic, with a repeat procedure likely. This might consist of bilateral lateral rectus resection for those who initially underwent bilateral medial rectus recessions and a recess–resect procedure on the unoperated eye for those who underwent a unilateral procedure. A surgical correction for DVD or inferior oblique overaction might be indicated as well. Thus it is not uncommon for a patient with infantile esotropia to have two or three surgical procedures during childhood. A significant fraction of patients who initially achieve alignment later develop accommodative esotropia and require treatment with glasses. Preoperative parental education regarding these common postoperative scenarios cannot be overemphasized. Asymmetrical monocular pursuit as measured by OKN testing persists indefinitely and may be a perpetual marker for infantile esotropia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here