Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Early diagnosis and treatment of ocular surface squamous neoplasia translates to preservation of the eye and vision.
Clinical monitoring for recurrence is imperative following treatment.
Suspicion should be raised with any unusual appearing pterygia or ocular surface tumefactions.
Excision with adjunct cryotherapy or postoperative topical chemotherapy/immunomodulatory therapy provides pathology for diagnosis and is the gold standard treatment of ocular surface squamous neoplasia.
Topical immunomodulatory therapy with interferon α-2b is an attractive alternative to surgery in ocular surface neoplasia.
Sebaceous cell carcinoma should be strongly considered in all unusual and unresponsive cases of blepharitis, chalazia, and ocular surface inflammation.
Expert histopathology is imperative for diagnosis and patient management.
The ectodermally derived nonkeratinized stratified squamous epithelia of the cornea and conjunctiva are contiguous. Therefore tumors arising within them are pathologically inseparable. Although they are contiguous, a significant transition occurs at the corneoscleral limbus. Here, the delicate substantia propria of the conjunctiva becomes condensed into the Bowman layer, a dense acellular connective tissue layer beneath the corneal epithelium. The presence of the Bowman layer provides the cornea with unique protection from deep invasion by epithelial neoplasia. Also at the limbus, the nonsquamous conjunctival cells, including mucin-producing goblet cells and most immunogenic cells, are normally excluded from the corneal epithelium. At the limbus itself, numerous melanocytes are present. Most importantly, the limbal epithelium is mitotically active and is the source of all new corneal epithelial cells. If the cornea becomes traumatically deepithelialized, epithelial cells slide in from the peripheral limbus, filling the defect. As with other body regions with a high level of mitotic activity (e.g., the uterine cervix), most cases of ocular surface squamous neoplasia (OSSN) arise from the limbal zone and spread to include the adjacent conjunctival and corneal surfaces.
During evaluation of the patient with a suspected OSSN, the clinician should obtain a careful history including time of onset, growth pattern, history of sun exposure, and history of systemic disease or immunosuppression. Clinical evaluation should include careful slit lamp examination, palpation of the orbit, and examination of regional lymph nodes. Clinical photography is also important when suspicious lesions are being followed. Imaging using ultra–high-resolution optical coherence tomography (OCT) or in vivo confocal microscopy is increasingly being studied for its appropriate role in the diagnosis, staging, treatment, and follow-up of ocular surface neoplasms.
This chapter describes benign and malignant squamous epithelial neoplasms of the conjunctiva and cornea. For completeness, inflammatory and degenerative lesions and nonsquamous neoplasia are also discussed.
Benign hereditary intraepithelial dyskeratosis (BHID) is an autosomal dominant, bilateral, highly penetrant disorder that usually affects individuals in their first decade of life. Molecular analysis in two separate families has demonstrated duplication of a gene located on chromosome 4 (4 q35). Although spontaneous cases have been reported, it affects primarily members of the Haliwa Indians, a consanguineous kindred derived from an interracial mixture of black, white, and Native American backgrounds. The Haliwa reside in the Halifax and Washington counties of North Carolina.
The lesions are V-shaped, hyperplastic, translucent elevations that arise at the limbus ( Fig. 51.1 ). Foci of whiteness and dilated vessels may be present. Although the lesions do not extend centrally, corneal opacity with resultant visual loss can occur. Lesions may also arise in the oropharynx and buccal mucosa.
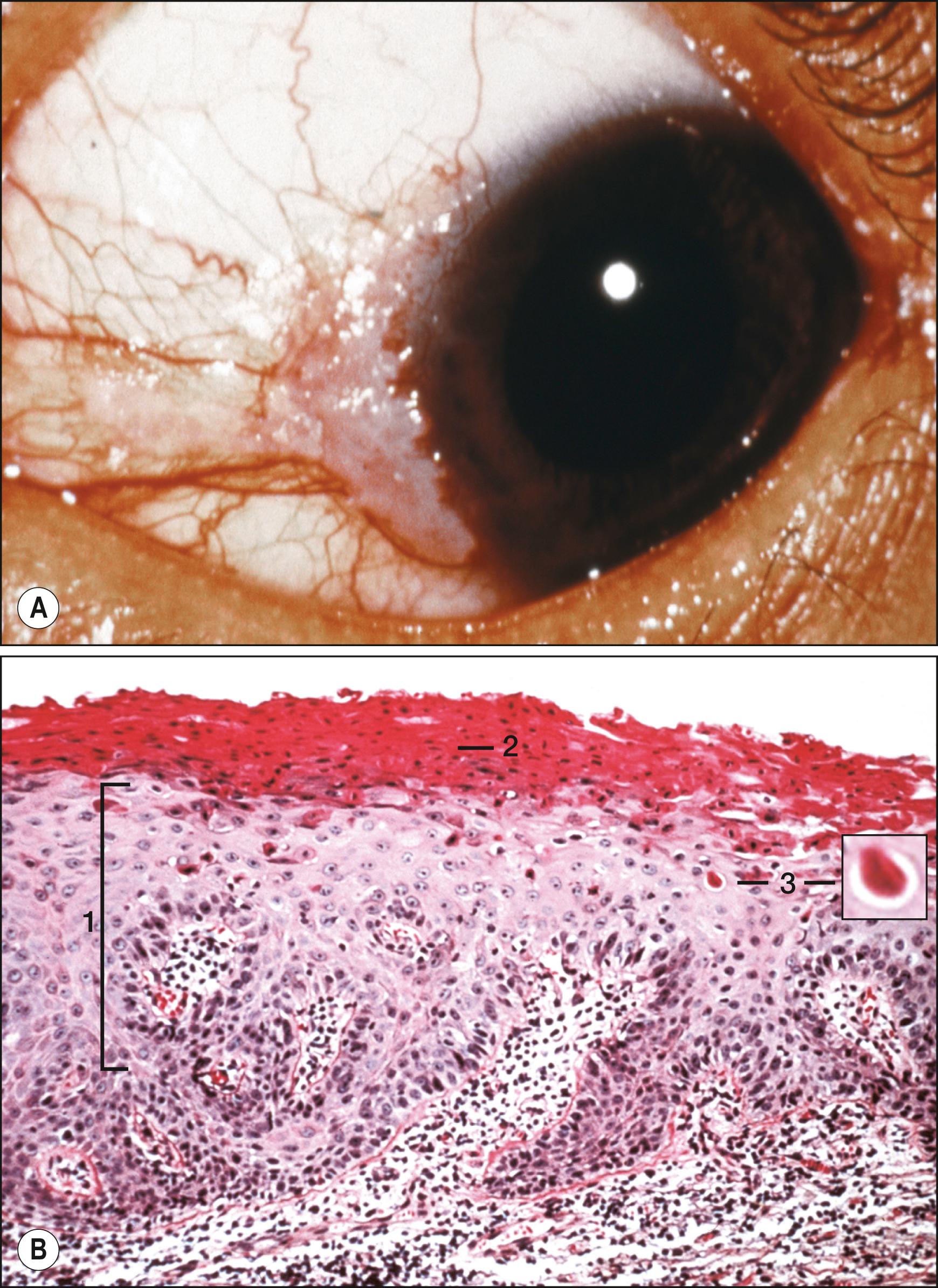
Biopsy reveals epithelial acanthosis, parakeratosis, and dyskeratosis (premature individual cell keratinization), and the stroma usually contains chronic inflammatory cells. Atypia is not present, and there is no dysplastic potential. Complete excision is the treatment of choice, although recurrences are likely because of the inherited nature of these lesions.
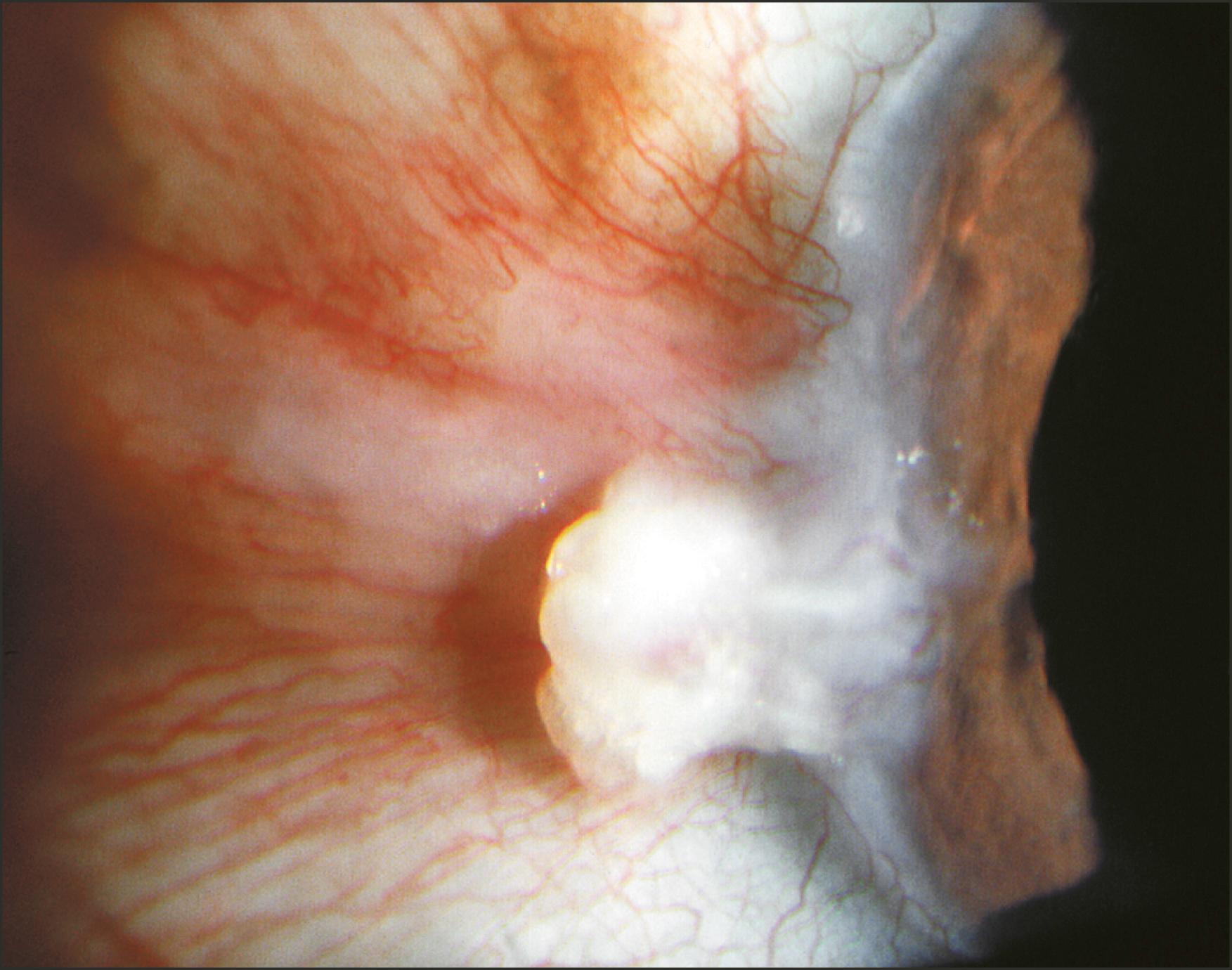
Pseudoepitheliomatous hyperplasia (PEH) is a benign, rapidly growing (usually arising over weeks to months) proliferation of conjunctival or corneal epithelium. , , Lesions often occur in response to some preexisting inflammation such as a pterygium. Clinically, the lesion is a white elevated mass with a hyperkeratotic surface. A central umbilication may be present. PEH can mimic ocular surface neoplasia ; when it arises at the limbus, differentiation from a squamous cell carcinoma can be difficult. PEH has a more rapid onset and lacks the capillary fronds seen as regular red dots in cases of squamous papillomas and carcinomas.
Histopathologically, massive epithelial acanthosis without severe cytologic atypia is present ( Fig. 51.2 ). Mitotic figures are often seen. The acanthotic epithelium may be pushed downward into the substantia propria, forming lobules of squamous cells with keratin whorls (invasive acanthosis). A nongranulomatous chronic inflammatory cell infiltrate is often present subjacent to the invading epithelium. The lateral margins of the lesion show a smooth transition into the surrounding normal epithelium in distinction to squamous dysplastic processes, in which the transition is abrupt.
Two cases of large cell acanthoma have been described. Clinically, the lesions are well defined with a fimbriated appearance. Histopathologically, these lesions are squamous proliferations comprising cells that are two to three times larger than normal conjunctival cells. Immunohistochemistry using p53, Ki-67, and cytokeratin stains can help to differentiate acanthomas from OSSN and squamous papillomas. Complete excision is required, as they may recur and rarely undergo malignant transformation. ,
Although usually of cutaneous origin, keratoacanthomas may also arise in the conjunctiva and caruncle and are considered by many to represent a variant of well-differentiated squamous cell carcinoma. Marked acanthosis is present histopathologically, but keratoacanthomas grow in an endophytic cup-like fashion about a central core of keratin debris. Simple excision is usually curative.
Conjunctival squamous papillomas are unilateral or bilateral benign lesions that may arise anywhere on the conjunctiva. These lesions are termed papillomas because of the presence of a central vascular core surrounded or covered by squamous epithelium. Clinically, the lesions may be either exophytic or, much more rarely, inverted (see later). Exophytic lesions (termed pedunculated ) may either arise from a stalk (be pedunculated) or be flat, sessile, lesions ( Fig. 51.3 ). Lesions may occur singly or may multiply. The presence of multiple lesions is especially suggestive of an infection with human papillomavirus (HPV); subtypes 6, 11, 16, 18, and 33 have been associated with these conjunctival lesions and have been detected using hybrid capture and polymerase chain reaction (PCR) assays. HPV 45 has also been associated with conjunctival papilloma.
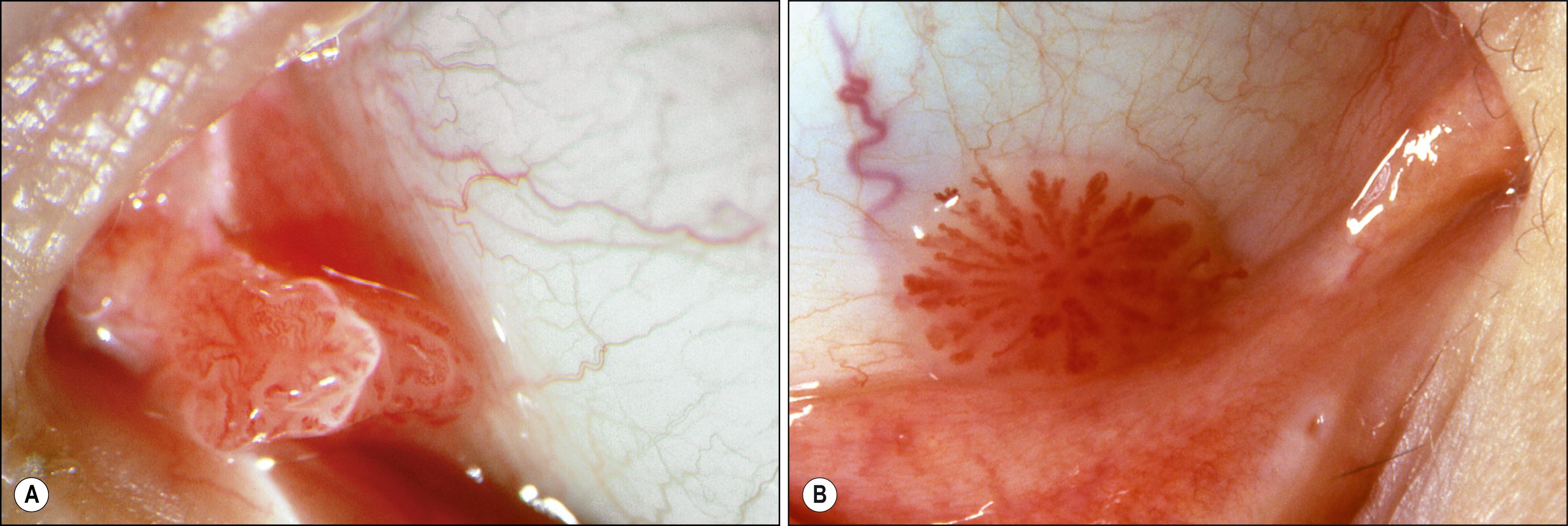
Clinically, the lesions may occur anywhere on the conjunctival surface. Papillomas have a transparent glistening surface through which the clinician can visualize multiple underlying capillaries that supply the connective tissue cores. These capillaries are seen as a characteristically arranged set of red dots. When the lesion is irritated, focal areas of keratinization may obscure underlying vascular details. Pigmentation may be present in darkly pigmented individuals. When lesions arise next to the cornea, a vascular pannus is present, but the cornea tends not to be invaded.
Most papillomas behave in a benign fashion, with little tendency to undergo malignant transformation. Signs of dysplasia include keratinization, symblepharon formation, inflammation, and palpebral conjunctival involvement.
Histopathologically, the lesions show acanthotic, nonkeratinizing squamous epithelium with a frond-like architecture. Melanocytes and goblet cells are variably present. Viral etiology is suggested by the presence of koilocytotic cells with hyperchromatic, “raisinoid” nuclei surrounded by clear cytoplasm as well as binucleation. Immunohistochemistry demonstrates that benign squamous papillomas tend to display lower levels of heat-shock protein 90 (HSP-90) expression than do higher-grade squamous dysplastic lesions, and they display a lower proliferation index with Ki-67 immunohistochemistry. ,
Management of papillomas is difficult and is complicated by multiple recurrences, especially in children. Multiple regimens including α-interferon, bevacizumab, and mitomycin C have been tried with variable success. The most effective treatment is simple excision with cryotherapy to the base and surrounding the lesion. Belfort et al. have described a novel in-office procedure using toluidine blue activated by pattern scanning photocoagulation, which produced a 100% response rate. Amniotic membrane transplantation can facilitate complete excisions of large lesions. Oral cimetidine (Tagamet) may act as an immunomodulator and thereby provide a systemic method of treatment. ,
Inverted conjunctival papillomas are a rare variant of the aforementioned conjunctival squamous papilloma. Also known as benign mucoepidermoid papilloma of the conjunctiva, the lesion grows in an endophytic manner. , Clinically, these lesions are benign and not precancerous, in distinction to inverted papillomas of the nasal tract, which can be locally destructive with significant malignant potential. Histopathologically, lobules of benign epithelial cells with numerous mucin-secreting cells (hence, the term mucoepidermoid ) push downward into the underlying connective tissue layer. Cellular atypia is not present; inflammatory cells may surround the lesion. Treatment is complete excision; recurrence after excision has not been reported.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here