Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
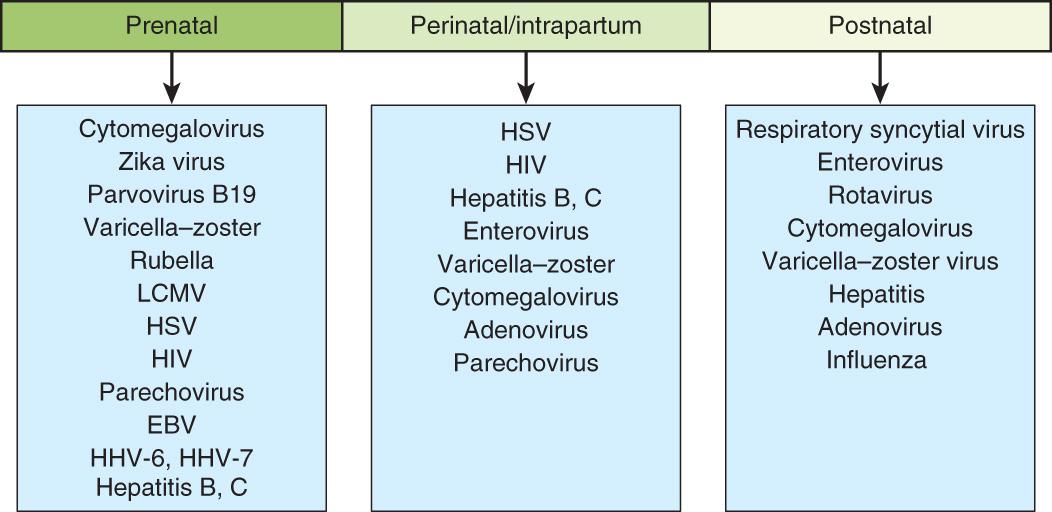
Infections in the newborn are often classified by their timing relative to birth and include congenital, perinatal, early-onset, and late-onset disease. These are clinically useful designations because the mechanisms of infection, etiologies, and outcomes are distinct at each stage. Congenital infection denotes infection acquired in utero. Such infections are generally caused by viral or other non-bacterial organisms and are often associated with injury to developing organs (see Chapter 131 ). Perinatal infection indicates acquisition around the time of delivery. Perinatally acquired organisms include both bacteria and viruses, some of which are the same as those causing congenital infection but often manifest with different features. Early-onset infection occurs in the 1st wk of life and is generally the consequence of infection caused by organisms acquired during the perinatal period. Late-onset infection occurs between 7 and 30 days of life and may include bacteria, viruses, or other organisms that are typically acquired in the postnatal period. Hospital-acquired infections typically occur beyond the 1st wk of life (see Chapter 130 ).
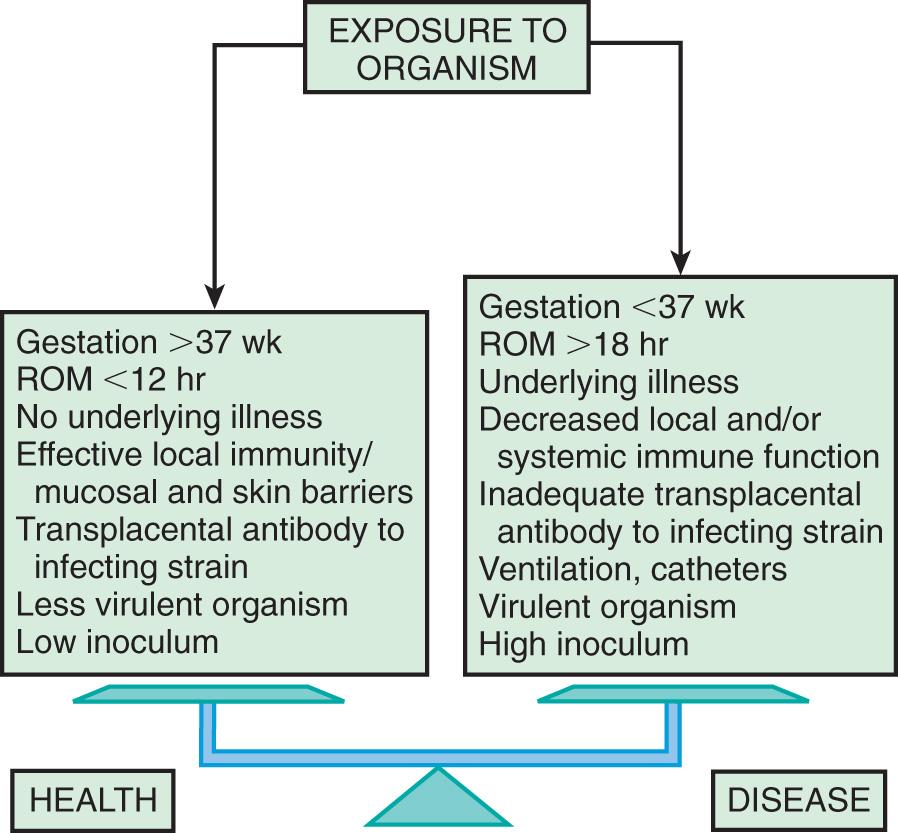
Neonates are uniquely prone to invasive disease because of their lack of fully responsive innate immunity ( Fig. 129.1 ). Attenuated immune responses often result in minimal or nonspecific clinical manifestations, and effective treatment requires attention to subtle signs of infection. Compared to older infants, newborns are often treated empirically while awaiting results of laboratory investigations. Preterm infants are particularly susceptible to infection because of their decreased innate immune and barrier defenses and their prolonged stay in hospital settings.
Despite advances in maternal and neonatal care, infections remain a frequent and important cause of neonatal and infant morbidity and mortality. Up to 10% of infants have infections in the 1st mo of life. Newborn infection is more common in areas with limited access to healthcare than in areas with well-established healthcare infrastructure. The overall incidence of neonatal sepsis ranges from 1 to 5 cases per 1,000 live births. Estimated incidence rates vary based on the case definition and the population studied. Globally, neonatal sepsis and other severe infections were responsible for an estimated 430,000 neonatal deaths in 2013, accounting for approximately 15% of all neonatal deaths.
A number of bacterial and nonbacterial agents may infect newborns in the intrapartum or postpartum period ( Table 129.1 ). Although herpes simplex virus (HSV), human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), and tuberculosis (TB) can each result in transplacental infection, the most common mode of transmission for these agents is intrapartum , during labor and delivery with passage through an infected birth canal (HIV, HSV, HBV), or postpartum , from contact with an infected mother or caretaker (TB) or with infected breast milk (HIV) ( Fig. 129.2 and Table 129.2 ). Any microorganism inhabiting the genitourinary or lower gastrointestinal tract may cause intrapartum and postpartum infection. The most common bacteria are group B streptococcus (GBS), Escherichia coli, and Klebsiella spp. Salmonella spp. are common causes of gram-negative sepsis in developing countries; less common causes of bacterial infection in the United States include Citrobacter , enterococci, gonococci, Listeria monocytogenes , Streptococcus pneumoniae, and Haemophilus influenzae . The more common viruses are cytomegalovirus (CMV), HSV, enteroviruses, and HIV ( Table 129.2 ).
VIRUSES
MYCOPLASMA
FUNGI
PROTOZOA
|
| VIRUSES | CONGENITAL | NATAL | POSTNATAL |
|---|---|---|---|
| Adenovirus | + | + | + |
| Chikungunya | ++ | + | − |
| Cytomegalovirus | ++ | ++ | ++ |
| Dengue | ++ | − | − |
| Ebola virus | ++ | + | + |
| Echoviruses | + | + | + |
| Epstein-Barr | + | − | + |
| Hepatitis A | − | ++ | + |
| Hepatitis B | + | ++ | + |
| Hepatitis C | + | ++ | − |
| Herpes simplex | + | ++ | + |
| Herpesvirus-6 | + | − | + |
| Human immunodeficiency virus | + | ++ | + |
| Human parvovirus B19 | + | − | − |
| Influenza | (+) | − | + |
| Lymphocytic choriomeningitis virus | ++ | − | − |
| Measles | + | − | + |
| Mumps | + | − | − |
| Parechovirus | − | + | + |
| Polioviruses | + | + | + |
| Rubella | ++ | − | − |
| Smallpox | + | + | + |
| St. Louis encephalitis | (+) | − | (+) |
| Type B coxsackieviruses | + | + | + |
| Vaccinia | + | + | + |
| Varicella-zoster virus | ++ | + | + |
| West Nile virus | + | − | + |
| Western equine encephalitis | + | − | + |
| Zika virus | ++ | ? | (+) |
++ , Major demonstrated route; +, minor demonstrated route; (+), suggested route, few supporting data; −, route not demonstrated.
Microorganisms causing pneumonia acquired during labor and delivery include GBS, gram-negative enteric aerobes, L. monocytogenes, genital Mycoplasma, Chlamydia trachomatis, CMV, HSV, and Candida spp. ( Table 129.3 ).
TRANSPLACENTAL
PERINATAL
POSTNATAL |
* More likely with mechanical ventilation or indwelling catheters, or after abdominal surgery.
The most common bacterial causes of neonatal meningitis are GBS, E. coli, and L. monocytogenes. S. pneumoniae, other streptococci, nontypable H. influenzae, both coagulase-positive and coagulase-negative staphylococci, Klebsiella, Enterobacter, Pseudomonas, Treponema pallidum, and Mycobacterium tuberculosis infection involving the central nervous system (CNS) may also result in meningitis.
The terms early-onset infection and late-onset infection refer to the different ages at onset of infection in the neonatal period. Early-onset sepsis is defined as the onset of symptoms before 7 days of age, although some experts limit the definition to infections occurring within the 1st 72 hr of life. Late-onset sepsis is generally defined as the onset of symptoms at ≥7 days of age. Similar to early-onset sepsis, there is variability in the definition, ranging from an onset at >72 hr of life to ≥7 days of age. Early-onset infections are acquired before or during delivery ( vertical mother-to-child transmission). Late-onset infections develop after delivery from organisms acquired in the hospital or the community. The age at onset depends on the timing of exposure and virulence of the infecting organism. Very-late-onset infections (onset after age 1 mo) may also occur, particularly in very-low-birthweight (VLBW) preterm infants or term infants requiring prolonged neonatal intensive care.
The incidence of neonatal bacterial sepsis varies from 1-4 per 1,000 live births, with geographic variation and changes over time. Studies suggest that term male infants have a higher incidence of sepsis than term females. This sex difference is less clear in preterm low-birthweight (LBW) infants. Attack rates of neonatal sepsis increase significantly in LBW infants in the presence of maternal chorioamnionitis, congenital immune defects, mutations of genes involved in the innate immune system, asplenia, galactosemia (E. coli), and malformations leading to high inocula of bacteria (e.g., obstructive uropathy).
Data from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network documented rates of early-onset sepsis among almost 400,000 live births at Network centers. The overall rate of early-onset sepsis was 0.98 cases per 1,000 live births, with rates inversely related to birthweight: 401-1,500 g, 10.96 per 1,000 births; 1,501-2,500 g, 1.38/1,000; and >2,500 g, 0.57/1,000 ( Table 129.4 ).
| BIRTHWEIGHT (g) | ||||
|---|---|---|---|---|
| 401-1,500 | 1,501-2,500 | >2,500 | All | |
| All | 10.96 | 1.38 | 0.57 | 0.98 |
| Group B streptococci | 2.08 | 0.38 | 0.35 | 0.41 |
| Escherichia coli | 5.09 | 0.54 | 0.07 | 0.28 |
* NICHD Neonatal Research Network/CDC Surveillance Study of Early-Onset Sepsis.
The incidence of meningitis is 0.2-0.4 per 1,000 live births in newborn infants and is higher in preterm infants. Bacterial meningitis may be associated with sepsis or may occur as a local meningeal infection. Up to one third of VLBW infants with late-onset meningitis have negative blood culture results . The discordance between results of blood and cerebrospinal fluid (CSF) cultures suggests that meningitis may be underdiagnosed among VLBW infants and emphasizes the need for culture of CSF in VLBW infants when late-onset sepsis is suspected and in all infants who have positive blood culture results. Most neonates with sepsis presenting in the 1st day of life have a positive blood culture; analysis of CSF is usually deferred until the unstable cardiorespiratory status (shock, respiratory failure) has stabilized.
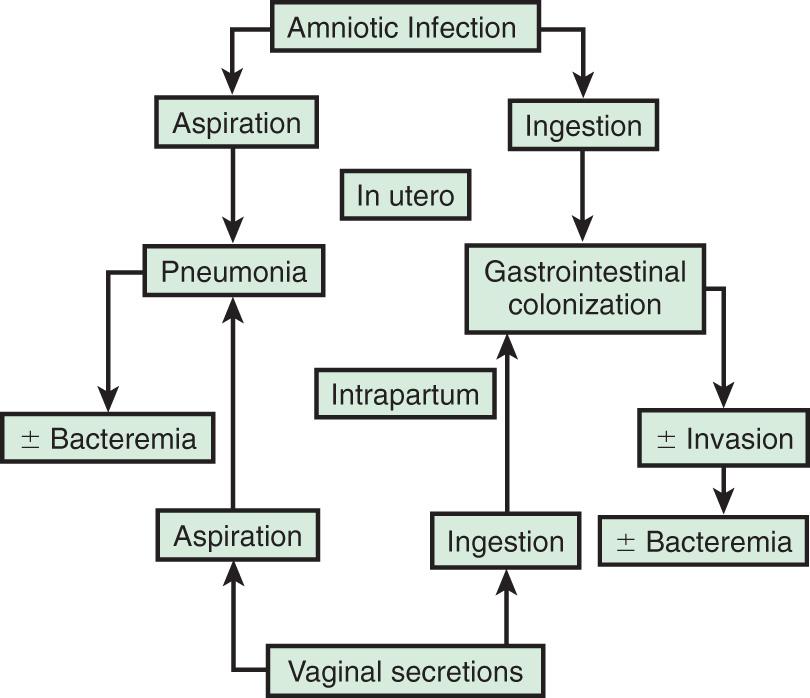
In most cases, the fetus or neonate is not exposed to potentially pathogenic bacteria until the membranes rupture and the infant passes through the birth canal and/or enters the extrauterine environment. The human birth canal is colonized with aerobic and anaerobic organisms that may result in ascending amniotic infection and/or colonization of the neonate at birth. Vertical transmission of bacterial agents that infect the amniotic fluid and vaginal canal may occur in utero or, more often, during labor and delivery ( Fig. 129.3 ).
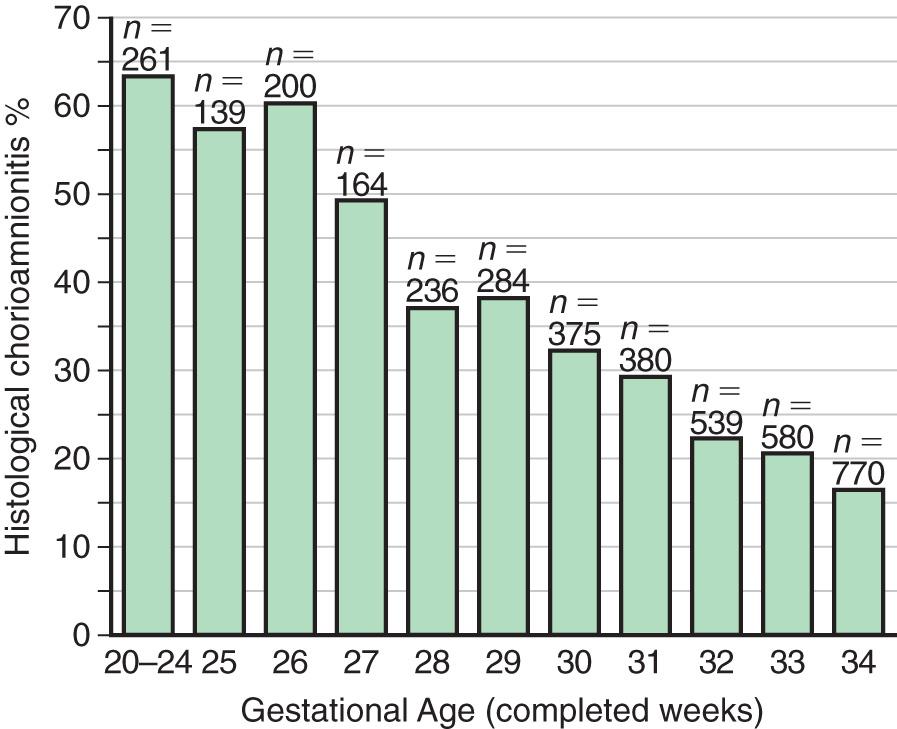
Chorioamnionitis results from microbial invasion of amniotic fluid, often as a result of prolonged rupture of the chorioamniotic membrane. Amniotic infection may also occur with apparently intact membranes or with a relatively brief duration of membrane rupture. The term chorioamnionitis refers to the clinical syndrome of intrauterine infection, which includes maternal fever, with or without local or systemic signs of chorioamnionitis (uterine tenderness, foul-smelling vaginal discharge/amniotic fluid, maternal leukocytosis, maternal and/or fetal tachycardia). Chorioamnionitis may also be asymptomatic, diagnosed only by amniotic fluid analysis or pathologic examination of the placenta. The rate of histologic chorioamnionitis is inversely related to gestational age at birth ( Fig. 129.4 ) and directly related to duration of membrane rupture.
Chorioamnionitis was thought to result from infection of the amniotic fluid but is now better defined by the term intrauterine inflammation or infection at birth (Triple I) . This is defined by fetal tachycardia, maternal leukocytosis (>15,000 cells in the absence of corticosteroids), purulent fluid from the cervical os, biochemical or microbiologic amniotic fluid changes consistent with infection, and fever (≥39.0°C/10.2°F) (see Chapter 131.2 ).
Rupture of membranes for >24 hr was once considered prolonged because microscopic evidence of inflammation of the membranes is uniformly present when the duration of rupture exceeds 24 hr. At 18 hr of membrane rupture, however, the incidence of early-onset disease with group B streptococcus (GBS) increases significantly; 18 hr is the appropriate cutoff for increased risk of neonatal infection (see Chapter 211 ).
Bacterial colonization does not always result in disease. Factors influencing which colonized infant will experience disease are not well understood but include prematurity, underlying illness, invasive procedures, inoculum size, virulence of the infecting organism, genetic predisposition, the innate immune system, host response, and transplacental maternal antibodies ( Fig. 129.5 ). Aspiration or ingestion of bacteria in amniotic fluid may lead to congenital pneumonia or systemic infection, with manifestations becoming apparent before delivery (fetal distress, tachycardia), at delivery (failure to breathe, respiratory distress, shock), or after a latent period of a few hours (respiratory distress, shock). Aspiration or ingestion of bacteria during the birth process may lead to infection after an interval of 1-2 days.
Resuscitation at birth, particularly if it involves endotracheal intubation, insertion of an umbilical vessel catheter, or both, is associated with an increased risk of bacterial infection. Explanations include the presence of infection at the time of birth or acquisition of infection during the invasive procedures associated with resuscitation.
After birth, neonates are exposed to infectious agents in the neonatal intensive care unit (NICU), the nursery, or in the community (including family). Postnatal infections may be transmitted by direct contact with hospital personnel, the mother, or other family members; from breast milk (HIV, CMV); or from inanimate sources such as contaminated equipment. The most common source of postnatal infections in hospitalized newborns is hand contamination of healthcare personnel, underscoring the importance of handwashing.
Most cases of meningitis result from hematogenous dissemination. Less often, meningitis results from contiguous spread as a result of contamination of open neural tube defects, congenital sinus tracts, or penetrating wounds from fetal scalp sampling or internal fetal electrocardiographic monitors. Cerebral abscess formation, ventriculitis, septic infarcts, hydrocephalus, and subdural effusions are complications of meningitis that occur more often in newborn infants than in older children. Metabolic factors, including hypoxia, acidosis, hypothermia, and inherited metabolic disorders (e.g., galactosemia), are likely to contribute to risk for and severity of neonatal sepsis
The most important neonatal factor predisposing to infection is prematurity or LBW. Preterm LBW infants have a 3- to 10-fold higher incidence of infection than full-term normal-birthweight infants. Possible explanations include (1) maternal genital tract infection is considered to be an important cause of preterm labor, with an increased risk of vertical transmission to the newborn; (2) the frequency of intraamniotic infection is inversely related to gestational age (see Figs. 129.1 and 129.5 ); (3) premature infants have documented immune dysfunction; and (4) premature infants often require prolonged intravenous access, endotracheal intubation, or other invasive procedures that provide a portal of entry or impair barrier and clearance mechanisms, putting them at continued risk for hospital-acquired infections.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here