Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Stroke is the second leading cause of death worldwide, accounting for 4 million deaths in 2004. Cerebrovascular disease is currently the fifth most common cause of death in the United States behind diseases of the heart, cancer, chronic lower respiratory diseases, and unintentional accidents. On average, every 40 seconds someone in the United States has a stroke and every 4 minutes, someone dies. Stroke is also a leading cause of long-term disability in adults, ranking third worldwide in 2015. There are a variety of nonmodifiable and modifiable stroke risk factors ( Box 28.1 ). Worldwide, a group of 10 modifiable risk factors (hypertension, current smoking, physical inactivity, high apolipoprotein ApoB/ApoA1 ratio, poor diet, high waist-to-hip ratio, psychosocial factors, cardiac disease, excessive alcohol consumption, and diabetes mellitus) account for 90.7% of population attributable stroke risk.
Age
Sex
Race-ethnicity
Diet/nutrition
Physical inactivity
Overweight/obesity
Environmental factors
Cigarette smoking
Alcohol consumption
Hypertension
Lipids
Diabetes
Atrial fibrillation
Sickle cell disease
Sleep disordered breathing
Fibrinogen, clotting factors, and inflammation
Blood homocysteine levels
Migraine
An estimated 795,000 people have a stroke in the United States each year, with an estimated 7.2 million people aged 20 years or older who have had a stroke living in the country. Ischemic strokes account for 87% of all strokes, with 10% due to parenchymal intracerebral hemorrhages (ICHs) and 3% occurring because of aneurysmal subarachnoid hemorrhages (SAHs). About 610,000 of these strokes are first events with 185,000 occurring in persons who had a prior stroke. The risk of first ischemic stroke varies by race-ethnicity. Based on data from 2005, age-adjusted ischemic stroke incidence was lower in whites (179/100,000) than blacks (294/100,000); incidence rates for ICH were 30 versus 56 and for SAH 8 versus 20 per 100,000 in whites compared to blacks, respectively). Approximately 55,000 more women than men had a stroke in the United States that year. In 2012, there were over 1 million hospital discharges for stroke and approximately 2.4 million physician office visits attributable to cerebrovascular disease. Likely an underestimate, about 5 million people in the United States report a physician-diagnosed transient ischemic attack (TIA). Two-thirds of patients hospitalized for stroke are over age 65. Among those over age 65 years, the rate of hospitalization for stroke is nearly three times higher for those over age 85 years (288/100,000) compared to those aged 65 to 74 years (108/100,000). Importantly, the population over age 85 years is anticipated to more than double from 6.3 million in 2015 to 14.6 million in 2040.
A TIA precedes approximately 15% to 23% of ischemic strokes, carries a 90-day stroke risk of 9% to 17%, and a 25% risk of death over the ensuing year. However, another study found lower 1-year rates of recurrent stroke or TIA (12%) or death (1.8%). About 20% of patients with symptoms of TIA or minor stroke are undiagnosed, and about half of all patients who have a TIA fail to report their symptoms to a healthcare provider. With an estimated 5 million people in the United States with a physician-diagnosed TIA, it is an important target for secondary stroke prevention.
Mortality from stroke accounted for 1 out of every 20 deaths in the United States in 2014 (133,000 deaths). Data on long-term survivorship following ischemic stroke reflect wide ranges of estimated mortality: 13% to 45% at 1 year, 36% to 69% at 5 years, and 31% to 87% at 10 years. In a recent population-based study, the cumulative mortality rates following stroke were 10.5% at 30 days, 21.2% at 1 year, 39.8% at 5 years, and 58.42% at 24 years. These estimates are primarily obtained from international studies or single regions within the United States. Women and minority populations may have higher long-term mortality following stroke, although the evidence is limited and more research is needed to evaluate differences by patient characteristics.
Disability and quality of life can be as important as mortality as stroke outcomes. Living with a major stroke can be considered as being worse than death by patients at high risk of stroke. Twenty percent of stroke survivors still require institutional care after 3 months, and 15% to 30% are permanently disabled. Given the large number of stroke survivors in the United States, effective rehabilitation and secondary prevention are important targets for public health interventions.
Acute stroke was among the 10 highest contributors to Medicare hospital costs in 2011, and was the 11th most costly for payers. In 2012 to 2013, the total annual cost of stroke in the United States was estimated at $33.9 billion with $17.9 billion attributed to direct costs. Total direct stroke-related medical costs are projected to increase to $184 billion by 2030. The mean lifetime cost of stroke was estimated to be $90,981 for ischemic stroke, $123,565 for ICH, $228,030 for SAH, and $103,576 averaged across all stroke subtypes.
Stroke mortality has varied regionally in the United States over the past 50 years, with the highest mortality rates in the southeast United States, a region of the country termed the “Stroke Belt” ( Fig. 28.1 ). The Stroke Belt is usually defined as including the eight southern states of North Carolina, South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas. These geographic differences have been documented since at least 1940, and despite some minor shifts, they still persist. The reason for the existence of the Stroke Belt remains uncertain. Within the Stroke Belt, a “buckle” region along the coastal plain of North Carolina, South Carolina, and Georgia was identified with even higher stroke mortality rates than the remainder of the Stroke Belt. Average stroke mortality is ≈ 20% higher in the Stroke Belt than in the rest of the nation and ≈ 40% higher in the stroke buckle. Overall, individuals living in the southeast United States have a 50% greater risk of dying from a stroke compared to residents of other regions. Higher stroke mortality rates are now also being noted in the Pacific northwest regions of the United States.
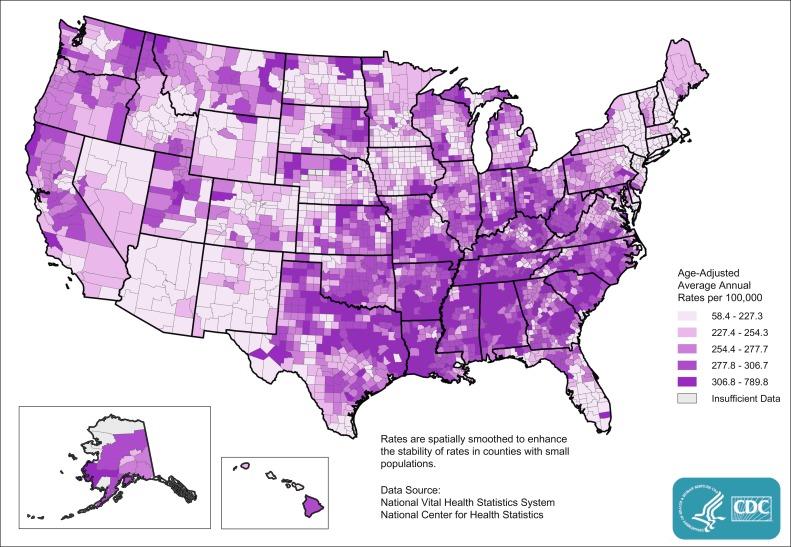
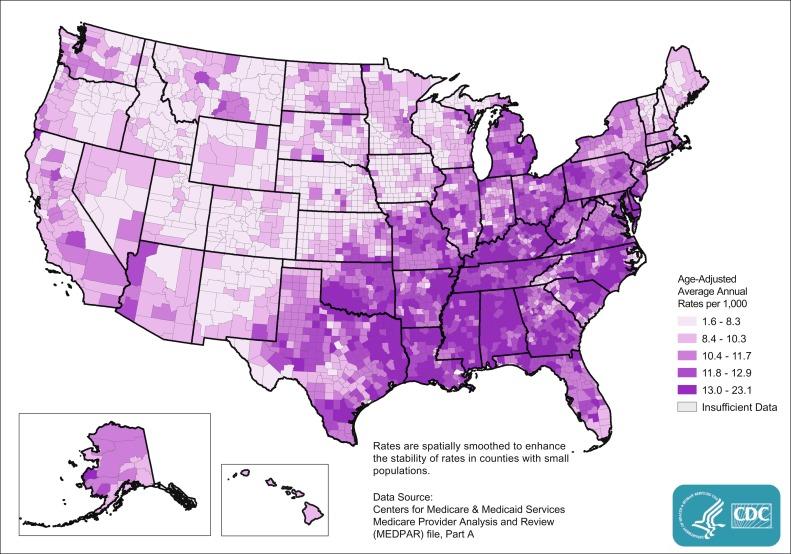
Total mortality reflects a combination of incidence and case-fatality rates. Stroke incidence is higher in the southeast, whereas case-fatality rates vary little across the country. Maps published by the Centers for Disease Control and Prevention (CDC) show geographic patterns in age-adjusted stroke hospitalization rates by county, which coincide with stroke mortality patterns ( Fig. 28.2 ). There are also regional differences in the rates of recurrent stroke events within the year after a stroke hospitalization, even after adjusting for common risk factors. The causes for these disparities remain unclear. National data are needed to monitor incident and prevalent stroke patterns over time, particularly by age, race-ethnicity, and sex subgroups.
Age is a major risk factor for stroke (the risk doubles with every decade of age over 55 years) and is relatively uncommon in children. The prevalence of perinatal strokes in the United States is 29/100,000 live births. Because of the lack of uniform case definitions, the true prevalence in likely higher. The overall annual incidence of stroke in US children aged 0 to 15 years is 6.4/100,000 children and for those aged 0 to 19 years is 4.6/100,000 children. Unlike adults, about half of all incident childhood strokes are hemorrhagic.
The rate of adverse outcomes and complications associated with stroke increase with advancing age. As reported by the CDC, 30-day stroke mortality rates increase with age from 9% in patients 65 to 74 years of age, to 13.1% in those 74 to 84 years of age, and 23% in those ≥ 85 years of age. The mean age of stroke patients in the United States is currently 70 years. The population aged > 65 years increased from 36.6 million in 2005 to 47.8 million in 2015 (a 30% increase) and is projected to more than double to 98 million in 2060; the population age > 85 years is expected to increase threefold, from 6.3 million in 2015 to 14.6 million in 2040. This will increase the proportions of the population at high risk of stroke, stroke mortality, and stroke-related complications based on age alone. Because stroke is so strongly age dependent, understanding the epidemiology of stroke in the elderly is critical for both clinicians and policy makers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here