Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The endovascular approach to venous obstructive lesions including stenoses and chronic total occlusions (CTOs) has replaced traditional open surgery. As a result, a broader spectrum of patients with comorbidities that might otherwise preclude an open approach have benefited. In addition, the results of venous stenting have been surprising enough to prompt a reexamination of fundamental pathophysiologic concepts in chronic venous disease: Venous obstruction seems to be as important as reflux in symptom expression and its resolution to treatment; obstructive pathology appears to be widely prevalent, not only in postthrombotic cases but also in most patients with deep venous disease of a nonthrombotic nature; and surprisingly, stent correction of venous obstruction alone in combined obstruction reflux seems to provide excellent symptom relief even when the associated reflux remains uncorrected. Taken together, these observations have the potential to change the treatment paradigms for chronic venous disease that have existed for more than 2 centuries.
It is now known that combined obstruction and reflux is the predominant pathology in postthrombotic syndrome (PTS). Strandness and colleagues showed that residual morphologic obstruction detectable by duplex ultrasound occurred in more than 80% in the chronic phase of the disease. The incidence of obstruction may be even higher based on intravascular ultrasound (IVUS) examination.
Valvular reflux has been considered for 2 centuries to be the salient pathology and the focus of treating chronic venous disease. Perhaps only 3% were thought to have an obstructive element related to the compression of the left iliac vein by the right iliac artery. The lesion was first described in early 19th century by McMurrich, and it is commonly referred to eponymously as May–Thurner syndrome or Cockett’s syndrome after their seminal publications on the topic.
The lesion is thought to result from trauma of repeated pulsations of the intimately related overlying artery. The obstruction results from luminal webs and membranes (some of which might have an embryologic origin) and not merely from external compression by the artery. Hence, the term nonthrombotic iliac vein lesion (NIVL) is preferred instead of the oft-used but misleading iliac compression syndrome.
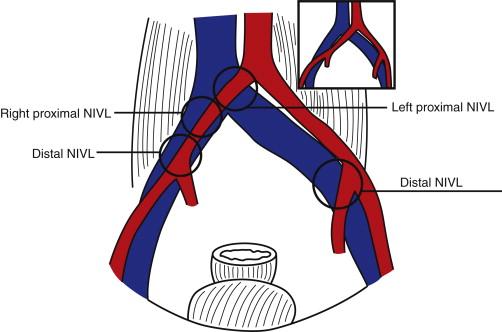
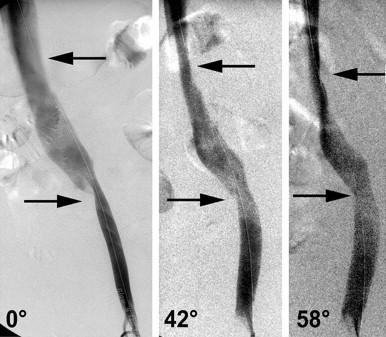
IVUS has greatly expanded current knowledge regarding NIVL. It occurs on both sides and in both sexes, involves all age groups, and is not confined to the left lower limb of young women as previously thought. NIVLs occur not only at the classic proximal site near the iliac–caval junction but also distally ( Figures 1 and 2 ).
NIVL and postthrombotic lesions of the iliac vein have a pathologic profile characteristic of permissive lesions. They can remain silent for long periods, even decades, until symptoms are precipitated by onset of additional or secondary pathologic event.
A general principle in treating such complex pathologies is to address the permissive lesion first, which often provides durable relief. It has been known for some time (recently confirmed by modern imaging techniques) that NIVLs are present in 30% to 50% of the general population in silent form. In fact, it has been a source of debate whether such lesions are pathologic or merely a normal anatomic variant. The dramatic clinical relief afforded by iliac vein stenting in symptomatic cases argues for the former concept.
Secondary events that can precipitate symptoms in the context of a preexisting NIVL include new onset of reflux, trauma, infection (cellulitis), venosclerosis (loss of elastic fibers) and seated orthostasis of the elderly, and many other secondary insults that upset the precarious compensated homeostasis that prevails. It is not surprising that NIVLs have a high prevalence on IVUS examination in patients with advanced chronic venous disease symptoms.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here