Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute aortic dissection (AAD) is a precipitous event associated with a wide range of outcomes from uncomplicated to catastrophic. Current endovascular strategies are based on identifying features that portend increased risk of death or other poor outcome, and applying interventional techniques to prevent the life-threatening complications of the dissection.
During the last 2 decades, there has been increasing interest in exploring endovascular procedures for management of aortic dissection. Initially, endovascular approaches focused on addressing branch vessel involvement and ischemic complications associated with the dissection process ( Fig. 34.1 ). Subsequently, endovascular aortic stent grafts (initially developed to repair aortic aneurysms) were applied in type B aortic dissection to cover the primary entry tear of the dissection and promote thrombosis of the thoracic aortic false lumen ( Fig. 34.2 ). These basic endovascular tactics are now routine in the contemporary armamentarium for treatment of aortic dissection and its myriad manifestations.
Endovascular approaches are complementary to the two traditional therapeutic paradigms of open surgical repair for type A dissection and medical treatment for uncomplicated type B disease. Invasive interventional procedures fit between the existing operative and noninvasive alternatives to provide effective options for type A dissection with severe branch vessel compromise (before or after ascending aortic repair), complicated type B dissection (branch vessel involvement, descending aortic rupture, extension of disease, or early aortic dilation, etc.), arch involvement, and ascending aortic intramural hematoma associated with an intimal tear distal to the left subclavian artery.
This chapter will review the specific endovascular procedures currently in use to manage aortic dissection, the patient subgroups in which these techniques are commonly employed, and the outcomes of these interventions.
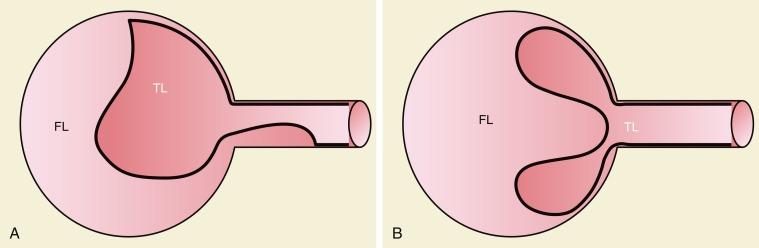
Branch vessel involvement accompanying aortic dissection is a well-recognized complication occurring in more than 30% of cases. For appropriate intervention selection, the pathoanatomical concepts of static and dynamic branch involvement are crucial to selection of the endovascular option for reperfusion of an affected vascular bed. As the dissection process extends distally from the primary entry tear, the dissection septum may engage the ostia of branch vessels. If the aortic flap, which consists of the intima and portion of the media shorn away from the wall, engages a branch orifice as it extends, two pathophysiological situations referred to respectively as static and dynamic branch involvement may occur ( Fig. 34.3 ).
One manifestation that may arise when the advancing dissection septum intersects an aortic branch is static branch vessel involvement ( Fig. 34.4 ). In static involvement, the aortic dissection flap extends directly into the branch for a variable distance. In this case, orientation of the septal trajectory is such that the branch ostium is incompletely engaged by the edge of the dissection plane. Rather than being circumferentially shorn by the septum, there is only partial circumferential involvement of the branch by the dissection. The aortic flap extends into the branch, creating a false lumen within the artery. As a result, the individual branch has both a true and false lumen, like the aorta.

Also similar to the aorta, a branch affected by static involvement may have multiple fates. At the end of the dissection where the flap terminates in the branch, a reentry tear in the false lumen may or may not occur. If a reentry tear occurs at the end of the false lumen, branch perfusion results from blood flow in both the true and false lumens. In many such cases, dual lumen perfusion is not associated with ischemic branch vessel symptoms. If reentry does not occur in cases of static branch vessel involvement, however, the false lumen within the branch has no outflow. The absence of a distal tear to allow communication with the vascular bed beyond the dissection may impair blood flow significantly. This no reentry state within the branch’s false lumen renders perfusion limited to that contributed by the true lumen. Unfortunately, the true lumen may be compromised by the engorged false lumen. The blind pouch of the false lumen, without outflow, swells to a maximum dimension at its distal end. The pressure exerted by the false lumen severely distorts and compresses the true lumen to markedly reduce branch vessel flow. Commonly, the degree of ischemia experienced by the involved vascular bed may be significant and can lead to irreversible tissue necrosis if not relieved quickly.
In no-reentry situations, a local solution directed at improving flow within the affected artery is required because the problem is localized within the specific branch. Two options for endovascular treatment are possible. Resistance to outflow within the false lumen may be decreased by creating a distal tear or fenestration within the blind channel. This can be accomplished with the end of a guidewire or other endovascular probe placed within the false lumen through the aortic false lumen. This approach is associated with practical challenges, including the avoidance of distal extension of the dissection process, safe penetration of the false lumen wall to create an effective outflow tear, and determination of the presence of thrombus within the blind sac of stagnant false lumen blood to avoid its distal embolization.
In most cases, the preferred strategy involves increasing branch flow by decreasing the resistance to true lumen blood flow. This is performed by placing a stent in the true lumen of the branch through catheterization from the aortic true lumen. The stent is typically placed from beyond the end of the false lumen in the branch back to the aortic true lumen. A self-expanding nitinol stent is commonly employed because this distance is frequently greater than 2 cm and because there is a risk of squeezing any existing clot out of the false lumen with a balloon-expandable stent. These stents are sized to the total transarterial diameter of the branch and allowed to progressively expand on their own (post deployment) without supplemental balloon dilation. There are many successful reports of this approach in mesenteric, renal, and iliac arteries affected by no-reentry or static involvement.
Occasionally, static branch vessel involvement with reentry anatomy and double-barrel flow may require endovascular intervention. The most common indication for stent placement in this setting occurs with involvement of a renal artery ( Fig. 34.5 ). The kidney supplied by a dissected renal artery may be affected by the physical presence of a flap within the branch. The variable flow reduction caused by the flap, and resultant disrupted pattern of true and false lumen perfusion, may contribute to an exacerbation of hypertension. In cases where high blood pressure is sustained and recalcitrant to numerous intravenous (IV) medications, endovascular intervention may be warranted to restore a single lumen without flap. The approach to treatment involves placement of a balloon-expandable renal stent within the true lumen of the renal artery through the aortic true lumen. In most cases, this type of reentry involvement does not extend into the branch as far as the no-reentry extension. Thus stents less than 2 cm long are typically implanted. This technique is well established at most centers that manage cases of aortic dissection frequently.
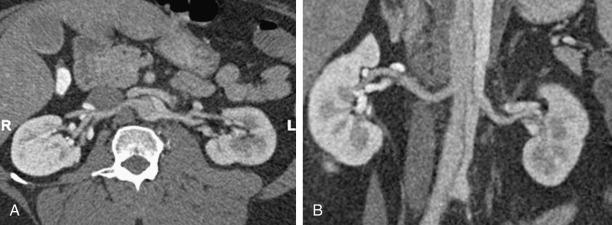
In addition to primary branch pathology that occurs as a complication of aortic dissection, another mechanism, dynamic branch vessel involvement, may be responsible for organ ischemia. Dynamic branch involvement is a phenomenon associated with obstruction to branch vessel flow by an aortic septum that has prolapsed over the branch ostia like a curtain. In contrast to static involvement, where the aortic flap extends directly into a branch, dynamic obstruction occurs as an aortic process exclusively without an associated branch lesion. Propagation of the aortic flap may create a circumferential cleavage of the aortic wall surrounding the branch ostium ( Fig. 34.6 ). Factors associated with this event include the flap trajectory, the resultant orientation of the septal plane proximal to the branch, and the inclusion of the ostium by the cleaved flap as it extends past. In this situation, the dissection septum surrounds the branch ostium as it tears distally. The cleavage plane extends 1 to 2 mm into the branch, and then circumferentially reenters, creating a cylindrical tear, coring out a short segment of the intimal/medial lining of the most proximal aspect of the branch. The septum retracts into the aortic lumen with a fenestration corresponding to the branch orifice. This gives the flap a stencil-like appearance when viewed en face, with the number of holes related to the number of branch vessels involved in this phenomenon. When imaged in an axial plane, the affected artery appears to originate exclusively from the aortic false lumen. Closer inspection usually allows the identification of a tear in the flap at the level of or adjacent to the level of the branch. The flap often displays small projections angled from the edge of the tear, giving its outline on axial imaging an appearance similar to the contour of a metal rivet, the short-legged extensions corresponding to the amputated proximal lining of the branch.

In dynamic branch obstruction, hemodynamic flow patterns result in a large aortic false lumen with a diminutive or collapsed true lumen. There is variability, however, in the degree of true lumen obliteration related to the dynamic compromise.
In the majority of aortic dissection cases with true and false lumen aortic flow (often called double-barrel flow ), the process described does not cause critical branch perfusion abnormalities. Flow to the branch originates primarily from the false lumen, with a small contribution from the true lumen through the corresponding fenestration in the aortic septum. Most of the false lumen flow usually occurs in diastole. During systole, the small contribution from the true lumen arrives through the septal window into the false lumen and branch. If the proximal primary tear is very large or the entry tear is in close proximity to the branch, the dominant flow pattern supplying branch perfusion may be in systole. In general, a branch that originates exclusively from the aortic false lumen is rarely affected by an ischemic complication.
Consistently, the aortic septum prolapses with a convex contour toward a compromised crescent-shaped true lumen. Consequently, all branches originating from the true lumen are at risk of obstruction. In this regard, the aortic septum in a dynamic obstructive process often assumes a coronal position, oriented across the aorta from left to right, in the distal descending thoracic proximal abdominal aortic segments. Thus the anteriorly oriented mesenteric vessels are in peril of ischemia because they frequently originate exclusively from a miniscule aortic true lumen. The likelihood of developing clinically relevant dynamic branch vessel compromise appears related in part to the area of the proximal entry tear. Although the process of dynamic involvement is dependent on multiple factors, as a general rule, the more severe the true lumen collapse, the larger or more circumferential the size of the proximal primary entry tear. Management of more than one ischemic vascular bed related to dynamic branch involvement and an obliterated aortic true lumen that supplies the compromised branches is most expeditiously and effectively approached by an endovascular aortic procedure rather than a strategy directed at the individual branches.
More than one mechanism of branch involvement can coexist in any given patient. The clinical manifestations and the analysis of imaging for any patient requires an individualized approach that must synthesize information and aortic and branch vessel involvement to customize an optimal treatment strategy that will safely, successfully, and durably address the most compelling effects of the dissection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here