Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endovascular therapy has become the mainstay of treatment for numerous vascular diseases and has even become preferable over open intervention in a variety of circumstances. In order to fully harness these therapies, vascular surgeons must be facile with a variety of instruments and techniques used for endovascular access, selective vessel catheterization, image acquisition, and post-processing, as well as with techniques to mitigate complications that can occur. The first step to any endovascular diagnostic procedure is to obtain access to a variety of arteries and veins located throughout the body. Safe and effective conduct of these procedures requires proper selection of needles, wires, and catheters. The purpose of this chapter is to familiarize the reader with these tools and techniques for diagnostic purposes.
The initial step of most endovascular diagnostic procedures is through percutaneous access of an artery or vein. The common femoral artery (CFA) is the most common site of access especially for aortoiliac or lower extremity diagnostic purposes. Brachial or axillary access is the second most common and can be a useful access point in patients with significant aortoiliac occlusive disease or for approaching the mesenteric or renal vessels due to the favorable angle for cannulation.
When choosing the access vessel, multiple factors must be considered including suitability of the vessel in relation to the procedure being completed, the ability to achieve hemostasis, the ease to readily convert to an open procedure and thoughtfulness of possible effects to tissues downstream of the cannulated vessel.
The suitability of a vessel for a procedure relates most importantly to the size of the vessel; anticipating the size of the catheters or sheaths required for performing the procedures and ensuring the target vessels can be readily reached or intervened on from the access vessel. For example, the aorta, iliac and downstream lower extremity vessels can be easily cannulated and accessed via the femoral vessels. If the iliac arteries are heavily calcified, stenotic, or occluded, an alternate choice might be the left brachial artery.
The terminal step of all angiography procedures is the attainment of hemostasis and is a critical step to ensure safe completion. In fact, the most common complication of angiographic procedures as a whole is related to access site complications (see Ch. 52 , Local Endovascular Complications and Their Management). These can include hematoma or pseudoaneurysm which may require further operative intervention. While there are numerous closure devices that can be used to achieve this step, they can be limited by vessel size or the presence of significant calcification which can result in device failure. As such, manual pressure should always be considered as an option for hemostasis. This makes the femoral vessels ideal for access as they can be easily compressed against the femoral head posteriorly. The brachial artery can similarly be compressed against the medial epicondyle of the humerus although the artery’s mobility renders compression more challenging. Furthermore, due to the encasement of the brachial sheath, a small hematoma is less forgiving and may result in nerve compression.
In the event of an immediately recognized access complication, such as sheath dislodgement or bleeding, the ability to convert percutaneous access to open to assess and repair any vessel injury is an important consideration. As an example, percutaneous access of the CFA is readily converted to open via a groin cutdown whereas vessels such as the axillary artery would entail much larger, possibly time-consuming surgical exposures for repair.
Selection of an appropriate vessel for access also entails that it is appropriately sized for the anticipated catheter and sheaths being used during the planned procedure. Small vessels may be completely occluded by larger sheaths thus resulting in ischemia in the downstream extremity or tissue being supplied by the access vessel. Although occlusion is less likely during diagnostic procedures since they tend to require smaller caliber catheters and sheaths, this is always an important consideration given that sluggish flow through the vessel can predispose to thrombosis and resultant ischemia. As such, cannulation of smaller vessels or the use of larger sheaths should always prompt consideration for intra-procedure heparinization.
Venous access typically mirrors arterial access with respect to vessel choice with the femoral vein being the most frequently accessed. Following venous cannulations, it is typically easier to achieve hemostasis given the more compliant vessel walls and lower pressures. Therefore, common venous access sites, such as the internal jugular vein (IJV) for vena cava filter retrieval or popliteal vein for venous thrombolysis, may not require direct posterior bony prominence for adequate compression and hemostasis.
Understanding the anatomy of each vessel is key to avoiding potential complications.
Anatomically, the CFA begins as the external iliac artery emerges from under the inguinal ligament. One can note the origins of the superficial epigastric and circumflex iliac arterial branches at its most proximal aspect as it overlies the medial aspect of the femoral head. It courses for a short distance of 5–8 cm and then bifurcates into the superficial and deep femoral arteries. Within the femoral sheath, the CFA is immediately medial to the femoral nerve, and lateral to the CFV. The inguinal ligament is a useful landmark that can be identified using surface anatomy, but it is critical to recognize that this anatomy can be easily distorted by body habitus or prior surgical procedures. The use of fluoroscopy can assist in identifying the femoral head as well as bony landmarks of the superior iliac spine and pubic tubercle which may be less than easy to palpate. Identification of these bony landmarks are helpful in delineating the superior-most extent of the common femoral artery prior to its transition into the external iliac above the inguinal ligament ( Fig. 62.1 ). Using a skin marker may be useful to define inguinal ligament.
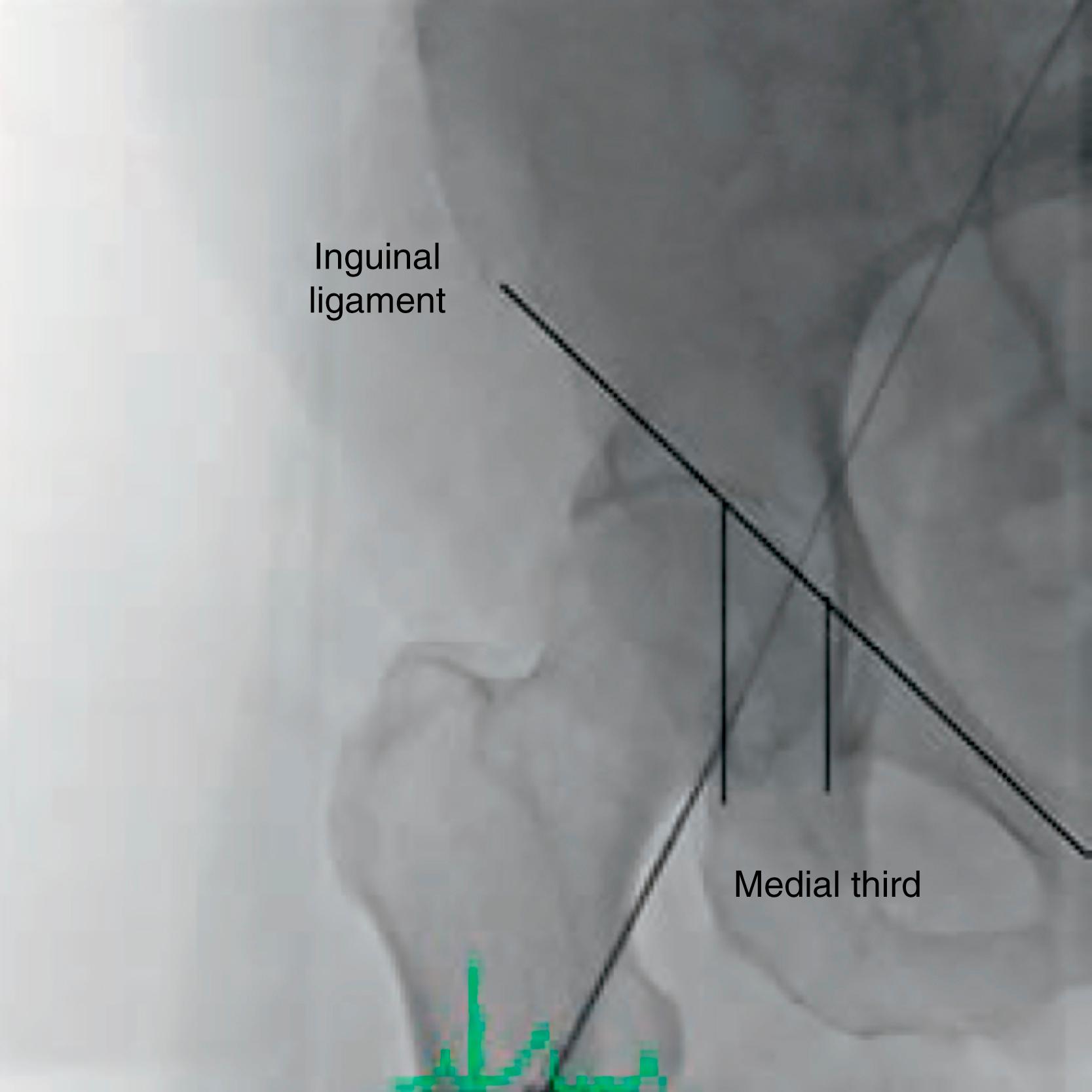
The CFA is an ideal choice for cannulation. It provides direct retrograde access to the aortoiliac system as well as most any arterial bed in the body. Its large caliber permits large devices introduction as well as safe room for most marketed percutaneous closure devices. Probably most importantly, the underlying femoral head allows easy compression and safe hemostasis even in the event of closure device failure. Most commonly, the CFA is accessed in retrograde fashion over the medial aspect of the femoral head. The location of the puncture is critical (see later). If puncture occurs too cephalad, either through or above the inguinal ligament, inadvertent puncture of the external iliac artery occurs, and a life-threatening retroperitoneal hematoma can result. Alternatively, if puncture is too distal, occurring in the superficial femoral artery (SFA), the risk of developing a pseudoaneurysm is quite high. SFA access can also result in an AV fistula from the profunda femoris artery or plaque dissection of the proximal SFA.
In certain circumstances, antegrade CFA access may be desired, more often for interventional rather than diagnostic purposes. Antegrade access may be chosen if the patient has a raised bifurcation in the setting of kissing iliac stents, causing difficulty with pushing a sheath over the aortic bifurcation. Antegrade access has the advantage of working in a single plane with excellent push ability for distal extremity procedures. Antegrade access into the CFA, however, can be more challenging than retrograde access. Needle puncture must still enter the CFA, but in antegrade access, the location is generally more on the proximal CFA to allow room to navigate wire and sheath into the SFA rather than the profunda artery. As such, this requires having a steep downward angle. In larger patients, this can be facilitated by retracting the pannus with tape.
Anatomically, the SFA becomes the popliteal artery when it exits Hunter’s canal in the distal medial thigh. Fluoroscopically, this is often defined as the point when the femoral artery passes posterior to the medial aspect of the distal femur. The popliteal artery travels behind the knee and bifurcates into the anterior tibial artery and tibioperoneal trunk. The latter subsequently divides into the peroneal artery and posterior tibial artery (together, the so-called trifurcation). The popliteal artery is flanked on each side by the duplicated popliteal vein.
While almost never done for diagnostic purposes, retrograde access of the popliteal artery while in a prone position can be used to attempt to cross and re-enter an occlusion of the SFA. Ultrasound guidance is paramount to distinguish the artery from its accompanying popliteal veins. This method has been largely abandoned as compression in the fatty popliteal space is often ineffective and pedal access has become more attractive.
Pedal access has gained favor in some fields especially for recanalization of severe tibial disease when antegrade attempts fail. Ultrasound guidance and micropuncture needles are universally used. Once arterial access is confirmed, work is often completed without a sheath, using wires and catheters directly.
Anatomically, the anterior tibial artery courses anterolaterally from the below-knee popliteal and traverses deep within the anterior compartment of the leg. It becomes more superficial at the ankle and becomes the dorsalis pedis artery. The dorsalis pedis is the ideal pedal access point for its superficial location and ease of compression for hemostasis. The posterior tibial artery courses posteromedially from the tibioperoneal trunk and is located in the deep posterior compartment of the leg. It becomes palpable near the ankle. This relatively superficial location is also amenable to percutaneous access and can be compressed readily for hemostasis. The peroneal artery is rarely used for percutaneous access. Coursing straight inferiorly from the tibioperoneal trunk, it is difficult to reach in its deep location within the deep posterior compartment of the leg, between the tibia and fibula.
Because of inability to manually compress, as well as vital surrounding structures, percutaneous iliac artery access is contraindicated. If these arteries are needed for device deployment, open surgical approach is required. Often these are cases in which a conduit is sewn end-to-side to the iliac artery to allow introduction of large bore sheaths and devices. Alternatively, endo-conduits can be used within the iliac system to allow larger delivery systems of TEVAR and TAVR devices using femoral access (see Ch. 80 , Thoracic Aortic Aneurysms: Endovascular Treatment).
Percutaneous cannulation of the axillary artery has been historically done in the intramuscular groove between the triceps and coracobrachialis muscle with the upper arm in abduction and flexion. This location has until recently been abandoned due to difficulty with adequate compression against the humerus and risk of median nerve compartment syndrome. Since the caliber change as it becomes the brachial artery, most practitioners favor the latter if upper extremity access is desired. However, percutaneous access of the infraclavicular axillary artery more proximal has recently been described. Theoretically, this allows for larger caliber access similar to the CFA if multiple sheaths are required during complex endovascular interventions. This technique is still under review for two reasons. Compression is impossible in the event of closure device failure and quick surgical exposure (unlike femoral access) carries risk of brachial plexus injury.
The axillary artery becomes the brachial artery as it passes under the teres minor. It can be easily palpated over the olecranon process when the arm is supinated. Ultrasound-guided access is often used in conjunction with a micropuncture needle to facilitate safe entry into the vessel. One must take care to access the artery over the medial epicondyle to allow for compression and hemostasis. Furthermore, ultrasound guidance is recommended to ensure a single puncture attempt at the 12 o’clock position. Even a small hematoma can cause nerve compression with the tight brachial sheath. Most practitioners comfortably use 6F or 7F sheaths at this location. Brachial artery access is often used for coronary revascularization procedures, dialysis access, subclavian artery disease and some EVAR or complex EVAR procedures (see Ch. 75 , Aortoiliac Aneurysms: Endovascular Treatment). Many favor brachial access for mesenteric vessel cannulation due to the downward angle of their origins.
The brachial artery bifurcates into the radial artery and ulnar arteries generally at the antecubital fossa. One should note that patients can have a higher bifurcation anywhere along the humerus. The radial artery has become the access of choice for most cardiologists and more recently for peripheral interventions. It is readily palpable in the distal extremity over the distal radius, and thus can be cannulated with ease, with or without using ultrasound guidance. Subsequent hemostasis is relatively straightforward through compression against the radius. Most patients are ulnar-dominant but all patients should undergo Allen’s testing or further imaging to ensure an intact palmar arch. If the patient is radial dominant and this is lost during intervention, the hand may become ischemic without collateral flow from the ulnar artery. The radial artery can accommodate sheaths between 4F and 6F, thus facilitating endovascular procedures that are using a 0.014” or 0.018” platform (see later).
Percutaneous common carotid artery (CCA) access is rarely performed for purely diagnostic purposes due to the risk of cerebral ischemia or embolization. Hemostasis is also a concern due to the inability to manually compress the carotid. Most practitioners will use CFA access with long guiding catheters or sheaths (see later) to achieve cannulation of the carotid artery. A hybrid technique is relied on for transcarotid artery revascularization (TCAR) when a small surgical incision is made to expose the CCA and direct puncture is then performed for antegrade sheath placement.
Venous access differs from arterial access in several important ways. While the pressure is significantly less, making hemostasis easier, it can also make access more difficult. There is less radial force keeping the vessel open, and one may find the wall collapsing with each attempt of needle puncture. Using a through and through technique in this case may be appropriate in some veins. While veins are capacitance vessels and can be quite large, they cannot stretch as much as arteries. When compared to arteries, veins are more prone to tearing if too large a sheath or device is used. The final important consideration is that while a simple access needle can be used to access arteries and confirm vessel entry, a syringe is helpful for venous cannulation. This serves two purposes: first, the plunger can be pulled back to generate a vacuum and confirm proper entry into the vein, and second, inadvertent entry of air into the venous system (air embolism) is avoided. This is particularly important when accessing a vein located above the heart, such as the IJV with the patient’s head up, where a negative venous pressure may exist and facilitate the entry of air into the system with potentially fatal consequences.
The CFV is commonly used for access when completing diagnostic procedures in the vena cava or its branches, such as the ovarian and internal iliac veins for pelvic congestion syndrome. The CFV is located medial to the CFA and can be compressed over the femoral head. Ultrasound guidance is often used for access to avoid injury to the CFA. This access readily allows catheterization of the contralateral extremity venous system, though navigating against the valves can require patience.
To access the popliteal vein, the patient is generally positioned prone. Popliteal veins are paired, flanking the popliteal artery on each side, and either vein can be used for access. Ultrasound is used for guidance, which is particularly important when cannulating this vessel to diagnose and treat deep vein thrombosis of the extremity veins, as the access location itself may be thrombosed, rendering blood return via the needle meager or nonexistent. Ultrasound visualization of the puncture and guide wire passage can be extremely helpful in this situation. Accessing a thrombosed popliteal vein can require practice as the halting advancement of the guide wire can fool the practitioner into believing they are not intraluminal.
The great and small saphenous veins are often cannulated for diagnostic and therapeutic purposes when treating patients for extremity deep vein thrombosis or for chronic venous insufficiency. Ultrasound guidance is typically necessary for access given their small size and distensibility. Most saphenous veins, both great and small, will typically accommodate at least a 6F sheath. The proximal small saphenous can be accessed to provide direct access to the popliteal vein to facilitate thrombolysis of femoral deep vein thrombosis (see Ch. 149 , Acute Lower Extremity Deep Venous Thrombosis: Surgical and Interventional Treatment).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here