Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Concern that contact lenses may be adversely affecting the corneal endothelium has resulted in endothelial examination becoming a routine procedure during biomicroscopic examination of the cornea of contact lens wearers ( Fig. 31.1 ). This concern can be traced back to the original observation by Zantos and Holden in 1979 of acute transient changes (‘blebs’) in the corneal endothelium associated with contact lens wear (see Chapter 30 ). This discovery gave the first clue to researchers and clinicians that the corneal endothelium was susceptible to short-term alterations in the physiological environment at the ocular surface.
Attention has also been directed towards the chronic endothelial changes induced by contact lenses; these include an apparent endothelial cell loss and changes in cell size/shape. This chapter will address the controversial question as to whether contact lens wear results in endothelial cell loss ( Fig. 31.2 ). The issue of contact lens–induced alterations to cell shape and size is dealt with in Chapter 32 .
There are differing opinions as to whether observable changes in the endothelium are of any real clinical significance; nevertheless, practitioners ought to be able to examine and assess the integrity of the endothelium and should be prepared to interpret any changes observed in the context of the various theories concerning corneal endothelial structure and function.
The corneal endothelium is a monolayer of approximately half a million cells (at birth) that constitutes the posterior corneal surface. Anteriorly, the endothelium is in apposition with a basement membrane that is formed by secretions from the endothelium itself. The basement membrane is known as the ‘posterior limiting lamina’ (or ‘Descemet’s membrane’). The anterior surface of the endothelial cell is known as the basal surface . The posterior (apical) surface of the endothelium is in direct contact with the aqueous humour.
Upon examination with the slit lamp biomicroscope, the endothelium can be observed using specular reflection. In the normal endothelium of an infant, all cells are approximately the same size and have a characteristic hexagonal shape. These features can only just be resolved by using a good-quality slit lamp biomicroscope at the highest magnification (× 40) ( Fig. 31.1 ).
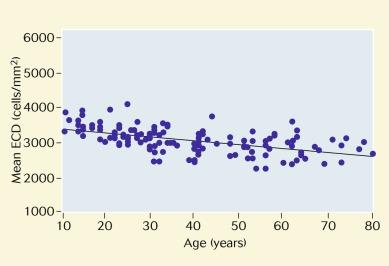
The convention that has been universally adopted for denoting the number of endothelial cells in the human cornea is to present the endothelial cell density , expressed as the number of cells per square millimetre. In the normal eye, endothelial cell density decreases from approximately 4,400 cells/mm 2 at birth to 2,200 cells/mm 2 at age 80 years ( Fig. 31.3 ). Obviously, any change in cell density thought to be attributed to contact lens wear must be considered in the context of this normal age-related change.
Early workers, all using different experimental methodologies, observed various degrees of endothelial polymegethism (see Chapter 32 ) in long-term contact lens wearers but failed to find evidence of a loss of endothelial cells. However, subsequent studies have challenged this notion.
Dada et al. examined the effects of long-term daily wear of polymethyl methacrylate (PMMA) lenses on the corneal endothelium in eight patients who had been prescribed lenses in one eye only. A significant reduction in cell density was observed in the lens-wearing eyes.
MacRae et al. examined 162 PMMA contact lens wearers and age-matched controls; 81 subjects had worn contact lenses for more than 20 years. These authors found that although the mean endothelial cell density in the PMMA lens–wearing group was not different from that in controls, a significantly greater percentage of lens wearers (9 (11%) of 81 patients) had cell densities less than 2,000 cells/mm 2 compared with controls (2 (2.5%) of 81 patients); that is, these authors noted a sub-group of PMMA contact lens wearers who were more susceptible to reduced endothelial cell densities with long-term contact lens use.
Setala et al. made observations similar to those of MacRae et al. These authors used a specular microscope to examine the endothelia of 101 subjects wearing soft lenses and PMMA lenses with wearing experience of 10 years or greater and that of 50 matched control subjects. The mean corneal endothelial cell density of the lens wearers (2,846 cells/mm 2 ) was statistically significantly less than that of the control eyes (2,940 cells/mm 2 ). The mean endothelial cell density of the eyes exposed to lens wear for greater than 25 years (30 eyes) was 2,575 cells/mm 2 , and very low densities (< 2,000 cells/mm 2 ) were observed in 16 eyes of the lens-wearing group (8%). Cell densities less than 2,500 cells/mm 2 were observed in a total of 41 eyes (20%) in the lens-wearing group, whereas in the control group (100 eyes), all of the subjects, except one, had cell densities of more than 2,500 cells/mm 2 in both eyes.
McMahon et al. reported that a group of 16 long-term PMMA lens wearers had an endothelial cell density (2,147 cells/mm 2 ) that was statistically significantly less than that of a matched control group of non–lens wearers (2,865 cells/mm 2 ). Hollingsworth and Efron reported that endothelial cell density was unaffected by rigid gas permeable lens wear (p = 0.36)
The effect on endothelial cell density of the duration of soft contact lens–wearing periods was explored by Lee et al. These authors divided 90 soft contact lens wearers into three equal groups: (a) short-term users (< 5 years of lens wear), (b) intermediate-term users, (6–10 years of lens war) and (c) long-term users (> 10 years of lens wear). Thirty non–contact lens wearers were included as controls. All eyes were examined with a specular microscope. The authors found that soft contact lens wear was significantly correlated with decreasing corneal endothelial cell densities with time.
Suzuki and Okamura reported that mean endothelial cell area increased by only 3% (i.e. endothelial cell density decreased) among 78 patients wearing disposable soft contact lenses. Chang et al. did not detect a change in endothelial cell density in 76 daily soft lens wearers who had been wearing lenses for at least 5 years. Yagmur et al. compared the endothelium of 71 contact lens wearers with myopia to 71 non–contact lens wearing controls. Endothelial cellular density in lens wearers (2,611.2 ± 298.4 cells/mm 2 ) was not significantly different from that of control subjects (2,643 ± 218.2 cells/mm 2 ).
Doughty et al. examined the endothelia of 18 patients who had been wearing hydrogel lenses for 5.5 years (range 3–9 years). The patients were re-fitted with silicone hydrogel lenses (Focus Night & Day) for continuous wear over 30 days and nights and were assessed immediately before and 6 months after the re-fitting, with lens replacement every 30 days. The mean endothelial cell area increased slightly from 358 to 363 μm 2 (p = 0.701), indicating a lower cell density.
Doughty also examined one eye of each of 46 subjects who had been wearing rigid lenses for 6.0 ± 1.6 years (range 3–9 years), using a non-contact specular microscope. The group cell area value was 401 ± 42 μm 2 to give an estimated endothelial cell density of 2,520 ± 273 cells/mm 2 . These values were not significantly different from values derived from a historical database.
Sanchis-Gimeno et al. studied the differences in endothelial cell density in a pair of 31-year-old monozygotic female twins; one had been wearing contact lenses for the past 15 years and the other had never worn contact lenses. Lower central corneal endothelial cell densities were found in both eyes of the monozygotic contact lens–wearing twin.
None of the reports highlighted here reported any adverse effects of altered endothelial cell density in lens wearers.
Leem et al. found that central endothelial cell density was lower in subjects with diabetes versus control subjects without diabetes. They also observed lower central endothelial cell densities in contact lens wearers with diabetes versus patients with diabetes who did not wear contact lenses. These data suggest that diabetes exacerbates endothelial cell redistribution. However, O’Donnell and Efron found that endothelial cell characteristics were similar for a group of patients with diabetes (type 1, n = 26; type 2, n = 4) who wore soft contact lenses versus a group of age-matched control subjects without diabetes who were also contact lens wearers (p > 0.05).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here