Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endoscopic ultrasonography (EUS)-guided celiac plexus interventions consist of the injection of neurolytic agents or steroids into ganglia to produce neurolysis or temporary block.
Celiac plexus block or neurolysis is the most common EUS-guided intervention in current practice. Significant pain control is achieved with the injection of ethanol in the setting of pancreatic cancer. More modest results are seen in patients with abdominal pain arising from chronic pancreatitis.
Advanced techniques include the use of brachytherapy in selected patients unfit for surgery or for palliative control of locally advanced cancers. Although preliminary data are promising, most of these procedures are still under clinical investigation.
EUS-guided placement of radiopaque markers into the tumor facilitates the delivery of radiation/proton therapy.
Endoscopic ultrasonography (EUS) today is not only an essential diagnostic tool for the diagnosis of gastrointestinal diseases but also has become a significant part of our therapeutic armamentarium. Using fine-needle aspiration (FNA) accessories, interventional EUS is often based on FNI therapy. Developments in interventional EUS have also highlighted a broad range of therapies beyond FNI, including celiac plexus neurolysis and block, brachytherapy, and fiducial placement.
In this chapter, the current clinical and experimental applications of interventional EUS for celiac plexus neurolysis, brachytherapy, and fiducial placement are reviewed and described with technical details.
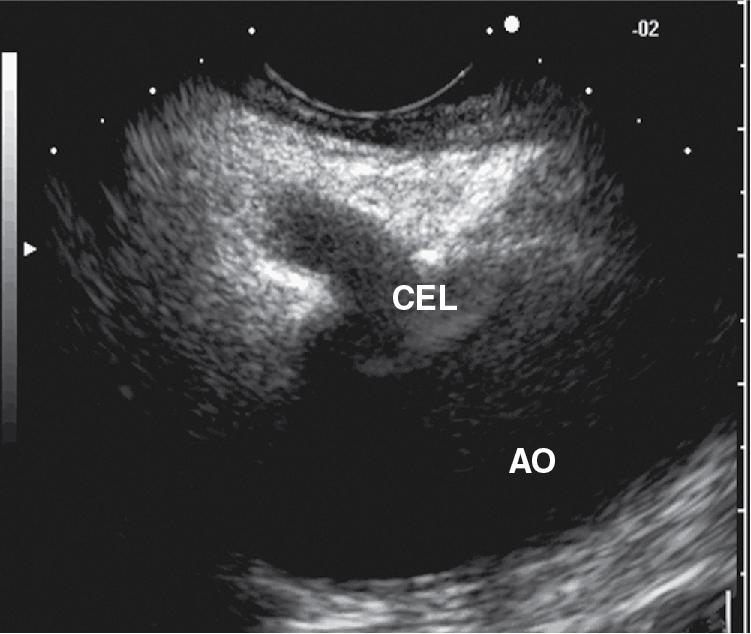
The principle of celiac injection therapy is based on the ability of EUS to guide injection of neurolytic agents directly into the celiac ganglia or the area around it. Celiac ganglia are sub-centimeter, elliptical, hypoechoic structures usually located around the celiac trunk as it takes off the abdominal aorta usually anteriorly or to the left ( Fig. 24.1 ). Presumably, the injected agent, such as ethanol, comes into contact with the ganglia and disrupts the ascending sympathetic ganglia. Histologically, there is evidence of neuronal vacuolization in nerves injected with ethanol. Because the efferent nerves from the pancreas travel with the sympathetic chain, interruption of the celiac ganglia should result in a decreased sense of pain. In the setting of pancreatic cancer, there is evidence of sensory nerve hyperplasia, and this may be the basis for often observed chronic abdominal pain.
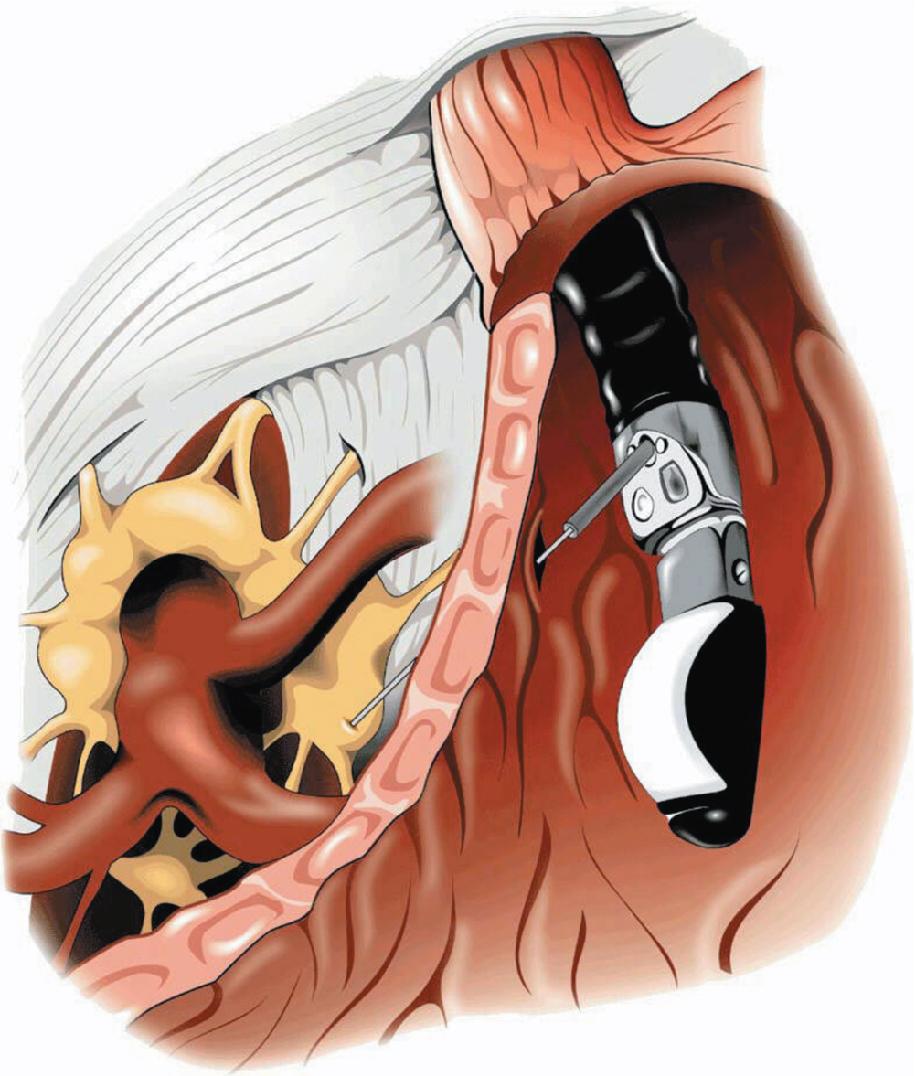
The technique for EUS-guided celiac plexus neurolysis (EUS CPN) and block is identical; the only difference is in the substances injected ( Fig. 24.2 , ![]() ). With a curvilinear array echoendoscope, the region of the celiac plexus is visualized from the lesser curve of the stomach by following the aorta to the origin of the main celiac artery. While studies have reported a high rate of celiac ganglia visualization by EUS in 62.5% to 89.4% of patients, others have reported only a modest rate of 25%.
). With a curvilinear array echoendoscope, the region of the celiac plexus is visualized from the lesser curve of the stomach by following the aorta to the origin of the main celiac artery. While studies have reported a high rate of celiac ganglia visualization by EUS in 62.5% to 89.4% of patients, others have reported only a modest rate of 25%.
A 22- or 19-gauge EUS FNA needle is usually used, but in some countries a dedicated 20-gauge cone-tip spray needle with multiple side holes is available and may allow solutions to disperse over a greater area. The needle tip is placed slightly anterior and cephalad to the origin of the celiac artery or directly into the ganglia if these can be identified as discrete structures. Aspiration is first performed to ensure that vascular puncture has not occurred. Three different administration methods have been described: (1) directly into the ganglia (when seen), (2) central (single) injection, and (3) bilateral injections. Central injection describes injecting the area at the angle of the celiac artery take off from the aorta anteriorly, while bilateral injection refers to injecting the sides of the celiac artery root by rotating the echoendoscope clockwise and anticlockwise (right and left to the celiac artery root). A local anesthetic is injected first, followed by alcohol (or triamcinolone for block). A recent study that compared 5 mL of Bupivacaine at two concentrations (0.375% and 0.75%) with 5 mL of 0.5% Ropivacaine found that 0.75% bupivacaine was superior in reducing postprocedural pain.
In a 2017 study, Kappelle and colleagues compared various EUS-guided celiac plexus administration techniques and ethanol volumes in four human cadavers by injecting either 1 or 4 mL in identified ganglion or 20 mL either centrally or bilateral to the celiac trunk. They found large-volume injections, either 4 mL in ganglia or 20 mL around the celiac trunk gave a more favorable ethanol distribution and likely were more effective in achieving neurolysis.
Patients should be observed for 2 to 4 hours with careful monitoring of pulse, blood pressure, temperature, and pain scores. Most units administer 500 to 1000 mL of intravenous normal saline preprocedure or postprocedure to avoid postprocedural hypotension.
The safety and efficacy of EUS CPN to alleviate refractory pain due to pancreatic cancer has been demonstrated in multiple large prospective clinical studies. , In a recent meta-analysis of 16 studies performed on 727 patients, the overall response rate to EUS-CPN was 68% (95% CI 61%–74%) at week 2 and 53% (95% CI 45%–62%) at week 4. It also looked at the three administration methods of ethanol: direct into ganglia versus central and bilateral techniques and found no difference between the three injection methods. Another meta-analysis of 16 studies showed a similar rate of pain relief with EUS-guided neurolysis of 71% (95% CI 68%–74%) ( Table 24.1 ).
| Authors (Year) | Patients (n) | Diagnosis | Technique | Pain Score Change |
|---|---|---|---|---|
| Puli et al. (2009) (meta-analysis) | 283 | Pancreatic cancer | CPN | 80% improvement (pooled data) |
| Puli et al. (2009) (meta-analysis) | 376 | Chronic pancreatitis | CPN | 59% improvement (pooled data) |
| Koulouris (2021) (meta-analysis) | 727 | Pancreatic cancer | CPN | 68% improvement at week 2 and 53% at week 4 |
| Asif (2021) (meta-analysis) | 980 | Pancreatic cancer | CPN | Overall symptom relief in 71%. 66% with central vs. 57% with bilateral injection |
| Wyse et al. (2011) | 48 | Pancreatic cancer | Early CPN | Significant decrease in mean pain score |
| Sakamoto et al. (2010) | 77 | Pancreatic cancer | CPN or BPN | Significantly better pain reduction in BPN cohort |
| LeBlanc et al. (2009) | 50 | Chronic pancreatitis | 1 or 2 injections for block | 65% for 1 injection and 59% for 2 injections at 4 weeks |
| Levy et al. (2008) | 33 | Pancreatic cancer and chronic pancreatitis | Direct ganglia injection | 94% improvement (cancer); 50% improvement (chronic pancreatitis) |
| Ascunce et al. (2011) | 64 | Pancreatic cancer | Direct ganglia injection or bilateral neurolysis | 65% improvement at direct ganglia, 25% in bilateral at first week |
| Doi et al. (2013) | 68 | Pancreatic cancer | Direct ganglia or celiac plexus neurolysis | 73% for ganglia and 45% for celiac plexus at first week |
| Bang JY (2019) | 26 | Pancreatic cancer | CPN vs RFA | Better quality of life at 4 weeks with RFA as compared to CPN. |
The effect of early EUS CPN was investigated in 96 patients with newly diagnosed, painful, inoperable pancreatic cancer in a randomized, double-blind, controlled trial. Pain relief was greater in the EUS-treated group at 1 month and significantly greater at 3 months. Morphine consumption tended to be lower at 3 months in the neurolysis group. However, there was no difference in quality of life or survival between the groups. Similar to this study, large trials have failed to demonstrate a significant improvement in survival time in patients with pancreatic cancer despite the high rates of symptom response to injection therapy.
To improve the efficacy of EUS CPN, EUS-guided broad plexus neurolysis (EUS BPN) extending over the territory of the superior mesenteric artery (SMA) was investigated and compared with standard EUS CPN in 67 patients with advanced abdominal cancer. EUS BPN patients exhibited significantly greater pain reduction at days 7 and 30 without incurring serious complications. This study suggests that broad neurolysis over the SMA may provide superior analgesia, but no further data have been published to confirm these promising observations. The same group reported that EUS celiac ganglia neurolysis (CGN) in conjunction with EUS BPN, when the celiac ganglia are visible, yielded significantly better pain relief at 1 and 4 weeks.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here