Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Right Orbital Subperiosteal Abscess Drainage
Acute rhinosinusitis (ARS) accounts for one-fifth of all adult and pediatric antibiotic prescriptions. Bacterial ARS can lead to orbital or intracranial infections by direct or hematogenous spread. If left untreated, this can result in permanent vision loss, meningitis, intracranial abscess, sepsis, and death. The incidence of serious complications from ARS has been estimated to be 1:12,000 in children and 1:32,000 in adults. Orbital complications are more common than intracranial complications and most commonly occur in male children.
Orbital complications have historically been categorized by Chandler’s classification, as shown in Table 30.1 . Most orbital complications occur from an infected ethmoid sinus, whereas the other paranasal sinuses are less frequently the source of the infection. Theories for explaining orbital spread include congenital dehiscence of the lamina papyracea, direct spread via ethmoid artery foramina, and the presence of valveless venous anastomoses draining the ethmoid and maxillary sinuses.
| Grade | Symptoms |
|---|---|
| 1 | Preseptal cellulitis |
| 2 | Orbital cellulitis |
| 3 | Subperiosteal abscess |
| 4 | Orbital abscess |
| 5 | Cavernous sinus thrombosis |
Subperiosteal abscesses (SPAs) of the orbit most commonly affect the medial wall but can also involve the inferior and superior orbital walls. In the past, surgical approaches for abscess drainage involved open orbitotomies and external approaches to the sinuses. More recently, endoscopic sinus surgery has largely replaced open techniques, as this obviates the need for a facial incision. However, visualization can be difficult owing to bleeding from the inflamed mucosa. This chapter illustrates the surgical management of SPAs that are amenable to transnasal endoscopic drainage.
Children are frequently seen in clinics with symptoms of fever, nasal congestion, nasal drainage, and facial pain consistent with ARS. Those with orbital complications are distinguished by ophthalmologic symptoms including eye swelling, blurry vision, pain, and limited ocular movements. Examination can demonstrate upper and lower eyelid swelling, decreased visual acuity, ophthalmoplegia, chemosis, and/or proptosis. SPAs may be difficult to distinguish from orbital cellulitis by clinical examination, but lateral or inferior displacement of the globe is suggestive of abscess formation. Nasal endoscopy may show swollen turbinates and purulent nasal drainage.
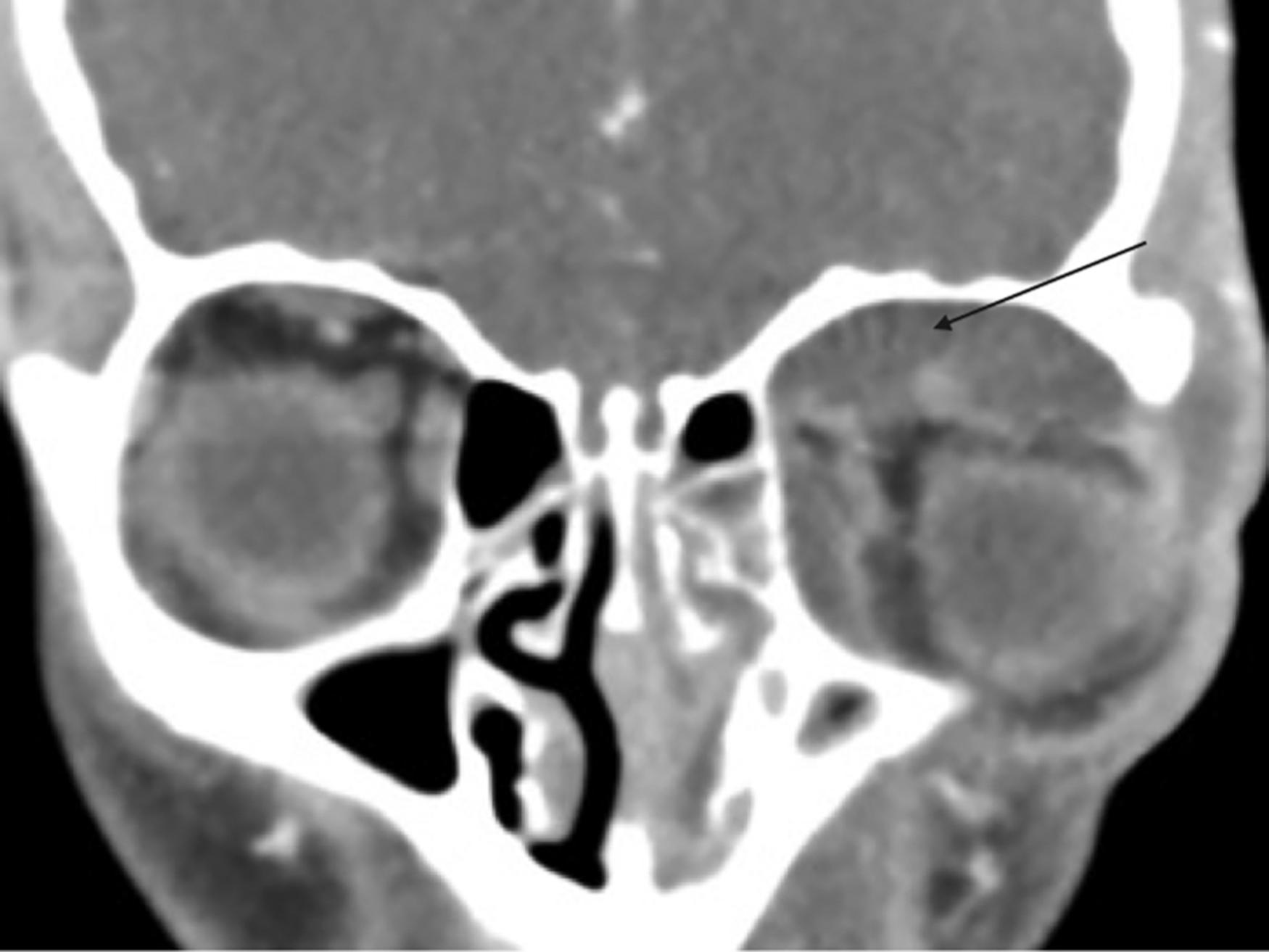
The initial workup includes a full ophthalmologic evaluation including assessment of the pupil, retina, intraocular pressure (IOP), extent of proptosis, and presence of chemosis. Laboratory tests, including complete blood count, basic metabolic panel, and inflammatory markers, are useful to establish baseline values and trends in cases that are observed or do not quickly resolve. If there is a concern for an orbital complication beyond preseptal cellulitis, computed tomography (CT) of the sinuses, preferably with contrast, is the investigation of choice. It is useful for preoperative planning to determine the extent of infection and specifically to exclude involvement of the cavernous sinus. A CT scan is quick and readily available, does not normally require sedation, and defines the bony and soft-tissue anatomy well. Many authors advocate broad-spectrum intravenous antibiotics for 24 to 48 hours and a CT scan only if there is worsening or no improvement. If there is concern for intracranial complications or invasive fungal sinusitis, magnetic resonance imaging (MRI) should be performed. However, MRI is not indicated for routine workup for orbital complications of ARS. Figs. 30.1 and 30.2 illustrate examples of SPAs.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here