Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The endoscopic resection of sellar and suprasellar tumors involves access to the sella via dissection through the sphenoid sinus.
These procedures are often done in a combined operation with both a neurosurgeon and otolaryngologist and thus employ a two-surgeon technique.
In this approach, the otolaryngology team provides the “pathway” and the neurosurgery team resects the tumor, with visualization provided by the otolaryngologist.
A wide sphenoidotomy is performed transnasally while preserving nasal structures such as the middle and inferior turbinates.
The sphenoid sinus originates from pneumatization of the sphenoid bone.
There are left and right sinuses, with an intersinus septum.
Each may pneumatize to varying sizes.
The sphenoid intersinus septum also has an unpredictable course. It often attaches off midline adjacent to a carotid artery.
Additional incomplete septa may also be present.
The sinus may pneumatize laterally beyond the vidian canal and foramen rotundum, forming a lateral recess.
A number of important structures are adjacent to the sphenoid sinus.
The sella often makes an impression to a variable extent along the posterior wall of the sphenoid sinus.
The optic nerves lie superolaterally.
The carotid arteries course lateral to the sinus bilaterally.
Both the optic nerves and carotid arteries may indent the sinus, either covered in thin bone or partially dehiscent.
The third, fourth, fifth, and sixth cranial nerves course in the cavernous sinuses situated lateral to the sinuses bilaterally.
The vidian nerve courses inferolaterally and may run within the sinus.
The size of the sella can affect the course of the carotid arteries; for example, a narrower sella is associated with more medially situated carotid arteries.
The superior portion of the sphenoid sinus can be affected by pneumatization of the posterior ethmoid cells when they form Onodi cells.
The degree of sphenoid pneumatization and the relationship of this pneumatization to the sella will affect the surgical time and amount of drilling required.
The postsellar configuration, the most common pattern, is characterized by pneumatization extending under the sella to its posterior portion ( Fig. 28.1A ).
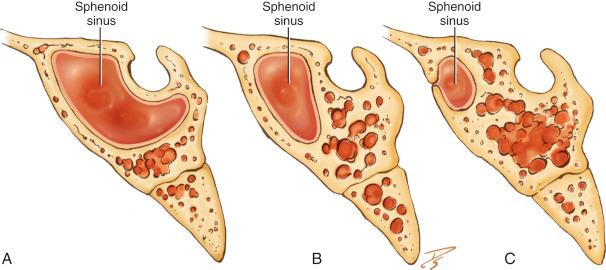
Sphenoid pneumatization occurs to a lesser extent in the sellar configuration; thus, a smaller impression is seen along the posterior sphenoid wall ( Fig. 28.1B ).
In the presellar configuration, the sinus pneumatization does not reach the anterior wall of the sella ( Fig. 28.1C ).
The conchal pattern is the least common pattern, characterized by a lack of sphenoid pneumatization with solid bone anterior and inferior to the sella.
The neurosurgery service is usually the primary service and requests a consultation with the otolaryngology service after a decision for surgery has been made.
An ophthalmologic evaluation is recommended and is often obtained preoperatively given the potential effect on the optic chiasm.
If the patient is not already being seen by an endocrinologist, an endocrinology consultation is also often obtained to evaluate the hormonal functional status of the tumor.
It is the role of the otolaryngologist to evaluate the sinonasal cavities for surgical planning and approach to the sella and parasellar regions.
During the patient’s preoperative visit, any history of sinonasal disease and/or previous surgery is elicited because this can impact the surgical approaches. Chronic rhinitis, rhinosinusitis, and sinonasal polyps should be controlled before surgery.
Nasal endoscopy is performed.
The size of the nasal cavities and the shape and deviation of the septum are noted. A septoplasty is planned for deviations that could hinder exposure of the surgical site and implementation of the two-surgeon technique with its required use of both nasal cavities during surgery.
The status of the sphenoethmoid recess is evaluated. The surgeon notes the ability to visualize the sphenoid ostia.
The location of the sphenoid ostium is noted.
Radiologic studies are obtained for surgical planning.
The presence of a tumor has usually already been diagnosed by magnetic resonance imaging (MRI).
A useful study for surgical planning is a computed tomography (CT) scan with an angiogram. It is recommended that this be done using the image guidance protocol.
These images can be used on the image guidance planning station to view the operative area in three planes—axial, coronal, and sagittal—for preoperative evaluation and surgical planning.
In addition, image guidance is often used during surgery to aid in confirming location during the dissection.
The teams must review a plan for reconstruction of the skull base once the tumor has been resected. This can often be accomplished with the use of free grafts (e.g., fascia or fat from the abdomen) in an underlay and/or overlay fashion. An additional option is the use of a nasoseptal flap, particularly in the presence of a cerebrospinal fluid (CSF) leak.
When the surgery is discussed with the patient, the role of each service is described in detail.
The risks of surgery are outlined, including orbital injury, vision loss, intracranial injury, CSF leakage, septal perforation, and decreased sense of smell.
The MRI best shows the tumor involvement and suprasellar extension as well as the relationship of the tumor to the pituitary gland and optic chiasm and involvement of the cavernous sinus and/or carotid arteries.
A CT scan of the sinuses is imperative for evaluation of the sinuses and for surgical planning. As mentioned previously, an invaluable step is review of the images in three planes using the image guidance planning station.
With these views, the sphenoid anatomy and pneumatization pattern are seen. The size of the sphenoid sinus on each side and the relationship of the sinus to the sella is evaluated.
The sella configuration—whether presellar, sellar, postsellar, or conchal—is easily seen in the sagittal views.
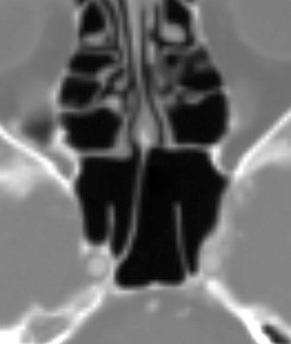
The site of the sphenoid ostia is determined. This is best identified in the axial views ( Fig. 28.2 ); then, the relationship of the ostia to the skull base is correlated in the sagittal views. This is an important anatomic landmark for orientation during the surgery. Ostia location is also crucial to identifying the location of the branch of the sphenopalatine artery when the plan is to use a nasoseptal flap for skull base reconstruction.
As mentioned earlier, the intersinus septum rarely courses in the midline; rather, it usually attaches off the midline adjacent to the carotid artery.
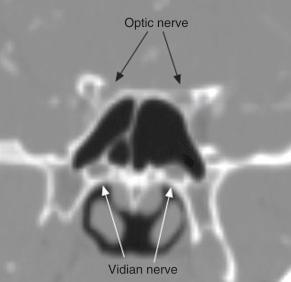
If the CT scans are done with angiography, the location and course of the carotid arteries are followed in all three planes. In particular, the relationship of the arteries to the sella is reviewed ( Fig. 28.3 ). The presence of any bony dehiscences is also noted.

The location of the optic nerves and their bony coverings is reviewed in the axial and coronal views. The presence of Onodi cells is recognized and planned for during surgery.
The relationship of the tumor to the carotid arteries and optic nerves is noted for surgical planning and can be confirmed intraoperatively ( Fig. 28.4 ).
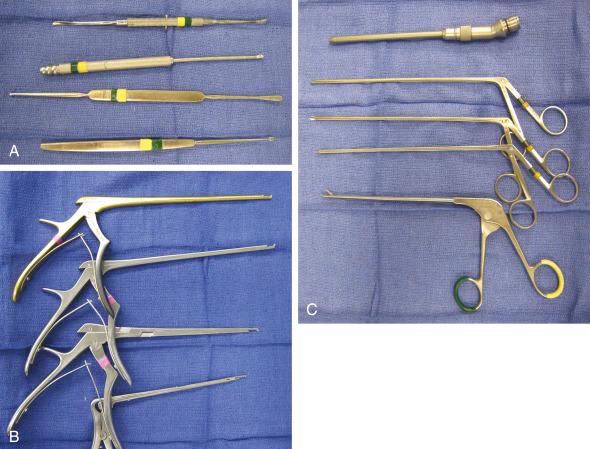
0-degree 2.7- and 4-mm endoscopes
Lens washer, for example, Endo-Scrub (Medtronic ENT, Jacksonville, Florida)
Straight 2.9- and 4.0-mm microdébrider blades
Cottle and Freer elevators
Straight-cutting and noncutting forceps
Kerrison punches, mushroom punch
Drill for thick bone (e.g., sphenoid rostrum)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here