Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Successful management of malignant clival pathology extending into the posterior fossa continues to be a formidable challenge to the skull base surgeon.
Classically, the clivus and posterior fossa have been approached using lateral and/or transoral-transpalatal routes.
These approaches often lead to collateral/bystander damage to functional tissue structures uninvolved with the primary disease and are commonly associated with cranial nerve deficits and other significant morbidities.
The endoscopic endonasal approach to the skull base allows access to the entire clivus and early identification of neurovascular structures within the posterior fossa.
This approach avoids cerebral and brainstem retraction to obviate concern of traction/injury to lower cranial nerves via open access to the entire clivus and early identification of neurovascular structure approaches.
It permits a magnified and highly illuminated view of a typically challenging area, in order to properly visualize the surgical target. Endoscopy allows improved discrimination and verification of tumor borders from normal tissue planes and even edematous/vasogenic brain parenchyma invaded by tumor.
Three-dimensional (depth) appreciation is lost on most two-dimensional monitor systems available today. This can be particularly challenging for neurosurgeons accustomed to the 3-D neuroanatomy seen through use of operating microscopes for intracranial or spine surgery.
Lengthy skull base procedures become confined by narrow nostril size and dimensions when performed in an endonasal manner by two surgeons.
The clival chordoma is a malignant tumor arising from remnant cells of the central notochord neuraxis, representing 0.1% of total skull base tumors, although for all chordomas, 1⁄3 arise at the skull base (compared to the sacrum and general spine).
Patients present with a wide constellation of symptoms based on route of tumor spread: intracranial extension (headaches, seizures, CN VI palsy) versus inferior spread into the nasopharynx, maxillary sinus, and nose (nasal obstruction, otalgia, and proptosis).
Represent low-grade malignancies of 3 subtypes: classic, chondroid, and dedifferentiated.
Classic histologic cell type: physaliferous “soap bubble” cells, which are large cells containing vacuolated cytoplasm.
Specific stains for cytokeratins, epithelial membrane antigen (EMA), brachyury, and MIB-1 can help to discriminate chordoma versus chondrosarcoma.
Primary treatment modality is surgical resection followed by adjuvant radiotherapy.
Although considered a low-grade neoplasm, given its locally aggressive behavior, overall 5-year survival approaches 60% to 70%.
Malignancy arising from endochondral cartilage; at the skull base, this is found at the petroclival sphenopetrosal, spheno-occipital, and petro-occipital synchondroses.
Similar to chordomas, 1⁄3 of chondrosarcomas are noted in association with the clivus.
Patients present with a wide constellation of symptoms related to intracranial and otologic concerns: headaches, seizures, diplopia, otalgia, symptoms associated with eustachian tube dysfunction, and trigeminal cranial neuropathy.
Histologically divided into 4 major subtypes: conventional (graded 1–3), mesenchymal, clear cell, and dedifferentiated. The most common subtype is seen microscopically as malignant cells admixed within abnormal sheets of cartilage.
Primary treatment modality is surgical resection followed by adjuvant radiotherapy, although adjuvant chemotherapy appears to be gaining favor in some institutions.
Five-year survival is reported to be as high as 90%, with a mean survival time of 4.5 years (median 2 years).
The word clivus, meaning “slope” in Latin, is the name used for the slanting depression behind the dorsum sellae formed by the junction of the sphenoid bone and the most anterior portion of the basilar occipital bone ( Fig. 30.1 ).
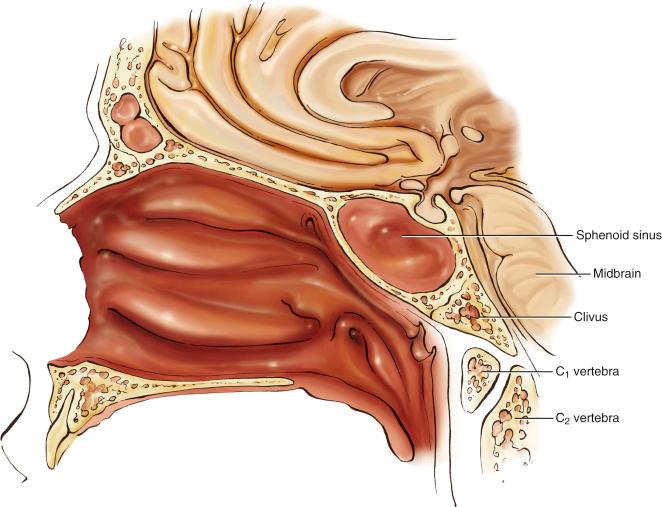
Functionally, the clivus separates the nasopharynx from the brainstem and posterior cranial fossa and serves to support a portion of the pons.
The clivus can be considered regionally: the upper clivus faces the nasopharynx anteriorly, and the superior aspect of the clivus includes the posterior clinoid process and dorsum sellae. This extends to the level of the petrous apex.
Intracranially, the upper 2⁄3 of the clivus bone is opposite the pons.
The inferior limit of the clivus is the foramen magnum.
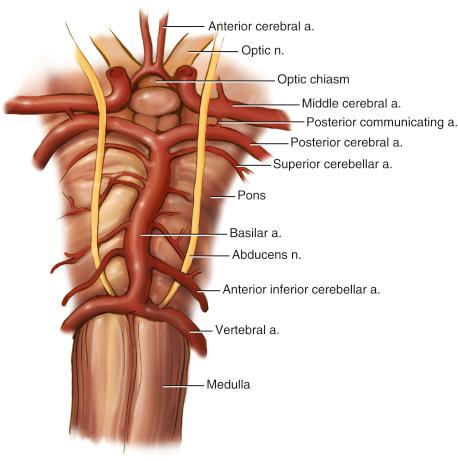
The clival periosteum is closely adherent to the ventral dura overlying the pons (superiorly) and medulla (inferiorly). Between the outer and inner layers of dura are the basilar venous plexus and the abducens nerves (CN VI), both of which are at significant risk during clival procedures.
The abducens nerve arises medially at the vertebrobasilar junction, then courses laterally before entering the dural plane of the clivus at the Dorello canal, and subsequently passes through the cavernous sinus.
Several important neurovascular structures lie just deep to the inner (intracranial) layer of clival dura. The basilar artery extends along the midline of the pons and arborizes into multiple paired feeder branches, including the superior cerebellar arteries, anterior inferior cerebellar arteries, and posterior cerebral arteries ( Fig. 30.2 ). Laterally, the intradural portions of cranial nerves III, IV, V, and VI can frequently be visualized.
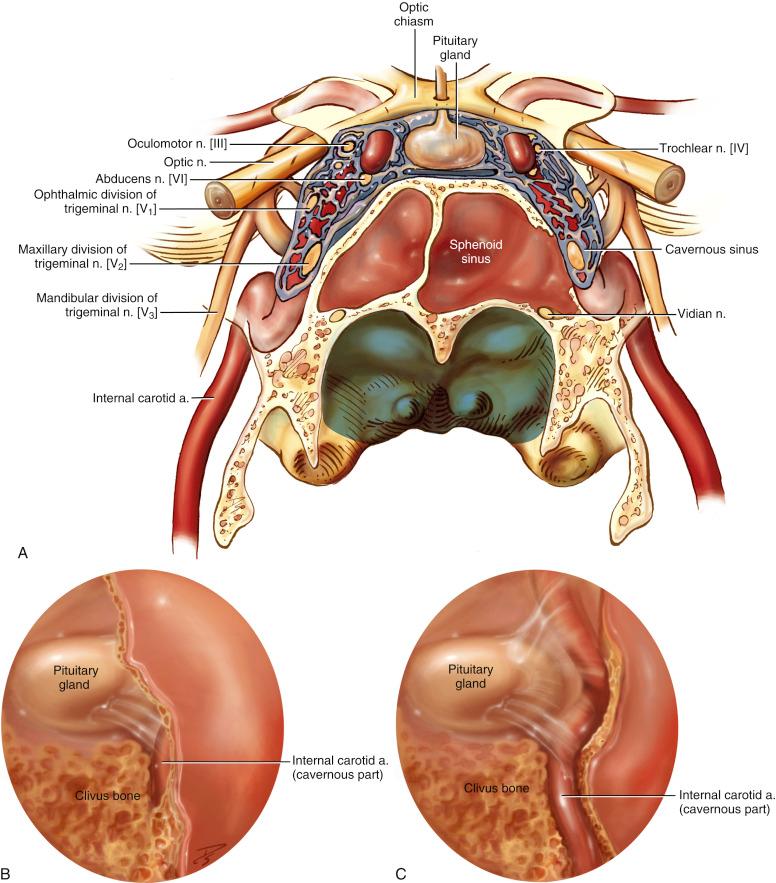
The endoscopic surgeon should be familiar with the full course of the internal carotid artery (ICA). The ICA cervical segment extends superiorly from the common carotid takeoff until it enters the carotid canal anterolateral to the jugular foramen and just medial to the styloid process. This petrous portion of the artery then courses along the temporal bone, where it has both a short vertical segment and a longer horizontal segment as the artery courses medially toward the petrous apex. The petrous ICA then passes the superior aspect of the foramen lacerum and gives rise to the vidian artery before the petrolingual ligament, which demarcates the start of the cavernous portion of the carotid. The ICA cavernous segment is quite tortuous as it winds between the dural linings of the cavernous sinus and can be seen endoscopically coursing along the posterolateral wall of the sphenoid sinus. After exiting the cavernous sinus, the ICA courses along the medial aspect of the anterior clinoid process, traverses the dura, and enters the intracranial vault ( Fig. 30.3 ).
As with other endoscopic endonasal skull base procedures, operations on clival lesions can typically be addressed by the otolaryngologist/head and neck surgeon with experience and advanced instrumentation in endoscopic skull base procedures. Certain complex lesions and virtually all with intracranial extension will necessitate the involvement of an endoneurosurgeon as well. The two-nostril technique is generally used to allow one or both surgeons to operate through a central corridor.
Appropriate case selection and angle of approach are paramount. A complex relationship between clival tumors and the ICA or vertebrobasilar system may place the patient at significant risk that might be avoided through the use of a lateral or subtemporal approach. Transdural, intracranial extension is rarely a contraindication to the endonasal approach, although it does increase the risks and complexity of the case considerably.
Monitoring cranial nerves and/or somatosensory evoked potentials (SSEPs) can be helpful; neurophysiologic monitoring use is based on the extent and location of the lesion and surgeon preference.
Navigation systems have become an essential component of endoscopic skull base procedures. The use of intraoperative navigation guided by fine-cut computed tomographic (CT) or magnetic resonance imaging (MRI) scans allows the surgeon to confirm their localization in the often partially distorted and hemorrhagic operative bed.
Preoperative placement of a lumbar drain is sometimes indicated, guided primarily by the anticipated size of the dural defect. Intrathecal fluorescein can be administered upon drain placement for intraoperative detection of cerebrospinal fluid (CSF) leaks.
If a CSF leak is anticipated on tumor extirpation, early in the case, there should be low threshold for elevation and protection of a pedicled intranasal rotational flap (such as the nasoseptal flap) to prevent damage or inadvertent resection of this reconstructive tissue source.
CT in combination with MRI are the radiographic studies of choice for evaluating most clival and skull base pathologic processes.
High-resolution CT scans can be used to evaluate bony erosion and/or confirm involvement of skull base foramina.
The use of MRIs best assists in differentiating chordoma and chondrosarcoma borders from nasopharyngeal mucosa, dura, or other soft tissue structures.
The clivus is best assessed via midline sagittal T1-weighted, unenhanced MRIs. The appearance of the clivus changes predictably with patient age, due to increasing proportions of fat-replaced marrow with age ( Fig. 30.4 ). This is important when diagnosing abnormal lesions of the clivus.
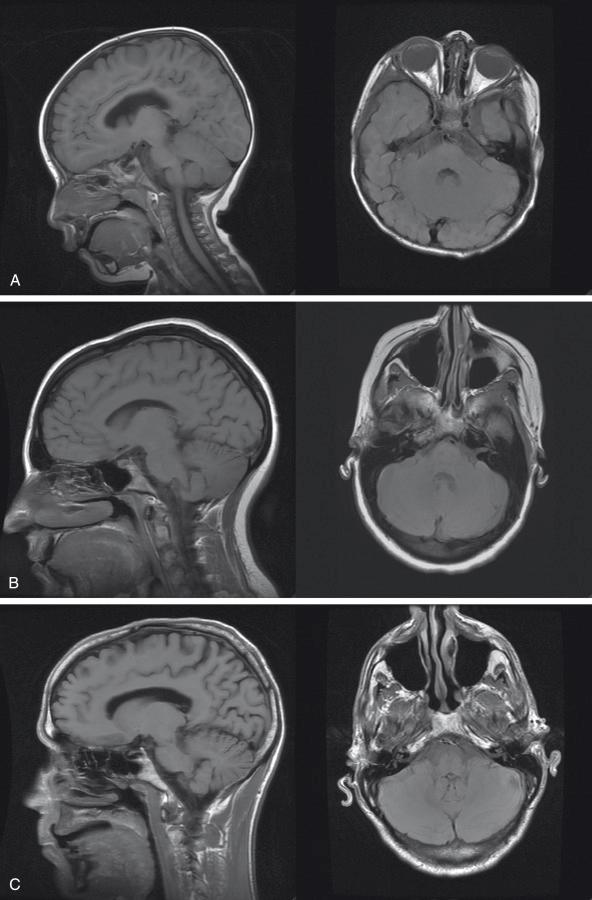
Many skull base neoplasms can be differentiated based on their appearance on CT and T1- and T2-weighted MRIs.
The course of the ICAs should be closely examined preoperatively. In rare cases, the ICA is situated in a medialized position and is at significant risk during a clival approach.
Any lateral extension of tumor should be identified early. Significant lateral extension can require additional surgical steps for adequate access, including resection of the medial and lateral pterygoid plates, transpterygoid access, or a cross-court approach. In some cases, far lateral tumor extent may require an alternative surgical approach entirely.
Some of the more common/classic lesions involving the clivus include:
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here