Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Microscopic transcortical or transcallosal approaches may be associated with brain injury and/or retraction that can result in seizures, focal neurologic deficits and cognitive impairment. Endoscopic approaches for the management of intraventricular lesions are intended to be minimally invasive with less brain retraction while providing direct visualization of the lesion.
MRI is preferred over CT to assess ventricular caliber, tumor characteristics and vascular anatomy to plan the approach and surgical strategy.
Benefits of the endoscopic approach to intraventricular tumors:
Excellent lighting allows close imaging of the lesion.
Since most intraventricular tumors cause hydrocephalus, the endoscopic approach can also be used to create CSF diversion through endoscopic third ventriculostomy and/or septal fenestration in addition to tumor debulking if needed.
Laterality of the approach is determined based on a preoperative MRI with emphasis on the relative size of the frontal horns of the lateral ventricles, the dimensions of the foramen of Monro and the asymmetric lateralization of the lesion. If feasible, the right lateral ventricle is preferred to avoid potential complications to the dominant hemisphere.
Neuroendoscopic resection of intraventricular tumors may be limited by the instrumentation available for use in the endoscopic working channel and the minimal maneuverability. Some instruments are already available to work through the working channel, including forceps, cautery, aspiration and side-cutting aspiration devices.
Intraventricular tumors include an extensive range of pathology. This includes, but is not limited to, ependymomas, choroid plexus papillomas, colloid cysts, meningiomas, epidermoid cyst, hemangioblastomas (especially associated with von Hippel–Lindau disease), neurocytomas, metastases and intra-axial tumors with an intraventricular exophytic component (e.g. astrocytomas, giant pituitary adenomas, craniopharyngiomas).
The endoscopic approach may be preferred as a minimally invasive technique for:
Small intraventricular tumors in the frontal horn of the lateral ventricles.
Lesions at the third ventricle protruding trough the foramen of Monro such as colloid cysts (especially when hydrocephalus is present and the ventricles are enlarged).
Endoscopic biopsy.
The success of endoscopic tumor removal is dependent upon the tumor characteristics including size, density and vascularity, as well as the caliber of the ventricular system.
Large tumors in the third ventricle may be better approached by a transcallosal approach.
Large tumors in the temporal horn or atrium are possibly better approached by a transcortical approach, either purely microscopic or endoscopically assisted.
In lesions at the posterior third ventricle the lateral ventricle may not be enlarged if the foramen of Monro is not obstructed, and therefore may lead to unnecessary and severe injury to the fornix. Furthermore, the lesion may be difficult to view with the use of a rigid endoscope. In these cases, a microscopic transcortical or transcallosal approach may be preferable (see Chapter 14 ).
The use of tubular retractors may facilitate the microscopic transcortical approach, allowing bimanual dissection, good visualization of the surrounding structures and a non-collapsible working channel with minimal disruption of the cortex (see Chapter 13 ).
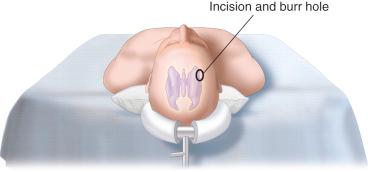
The patient is placed in the supine position and the head is stabilized in a 3-pin Mayfield fixation device allowing for neutral positioning of the head ( Figure 16.1 ).
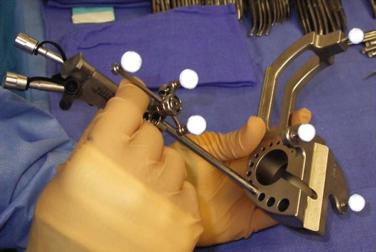
The tip of the endoscope and endoscopic working channel are registered with the neuronavigation system ( Figure 16.2 ).
A 2-cm frontal vertical incision is made 3 cm lateral to the midline (about the midpupillary line) anterior to the coronal suture. A more anterior trajectory is typically preferred for third ventricular lesions.
The entry site can also be selected by stereotactic guidance and marked on the skin surface. If the target is the third ventricle, because the intent is to work below the ipsilateral column of the fornix, the ideal trajectory passes just above the floor of the anterior horn, through the foramen of Monro, and below the roof of the third ventricle. In an axial and coronal plane, a trajectory is selected that passes between the head of the caudate and the column of the fornix into the foramen of Monro ( Table 16.1 ).
| Location | Position | Direction | Length of insertion | |
|---|---|---|---|---|
| Kocher's point | Frontal | 2–3 cm lateral to midline Approx. mid-pupillary line 1 cm anterior coronal suture |
Towards ipsilateral inner canthus Towards external auditory meatus |
5–6 cm |
| Frazier's point | Occipital | 3–4 cm lateral to midline 6 cm above the inion |
Perpendicular to cortex | 7–9 cm |
Regardless of the entry site, a linear or curvilinear incision is planned behind the hairline with a variable length depending upon the anterior location of the planned burr hole.
The skin incision (2–3 cm) is made down to the pericranium, and scalp hemostasis is ensured.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here