Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
What perinatal factors are associated with hypocalcemia in the immediate newborn period?
Prematurity
Asphyxia
Maternal diabetes
Maternal hyperparathyroidism
Transient congenital hypoparathyroidism
Congenital absence or hypoplasia of the parathyroid glands (sporadic or as part of DiGeorge syndrome)
How are calcium levels expected to change in premature infants during the first few days of life?
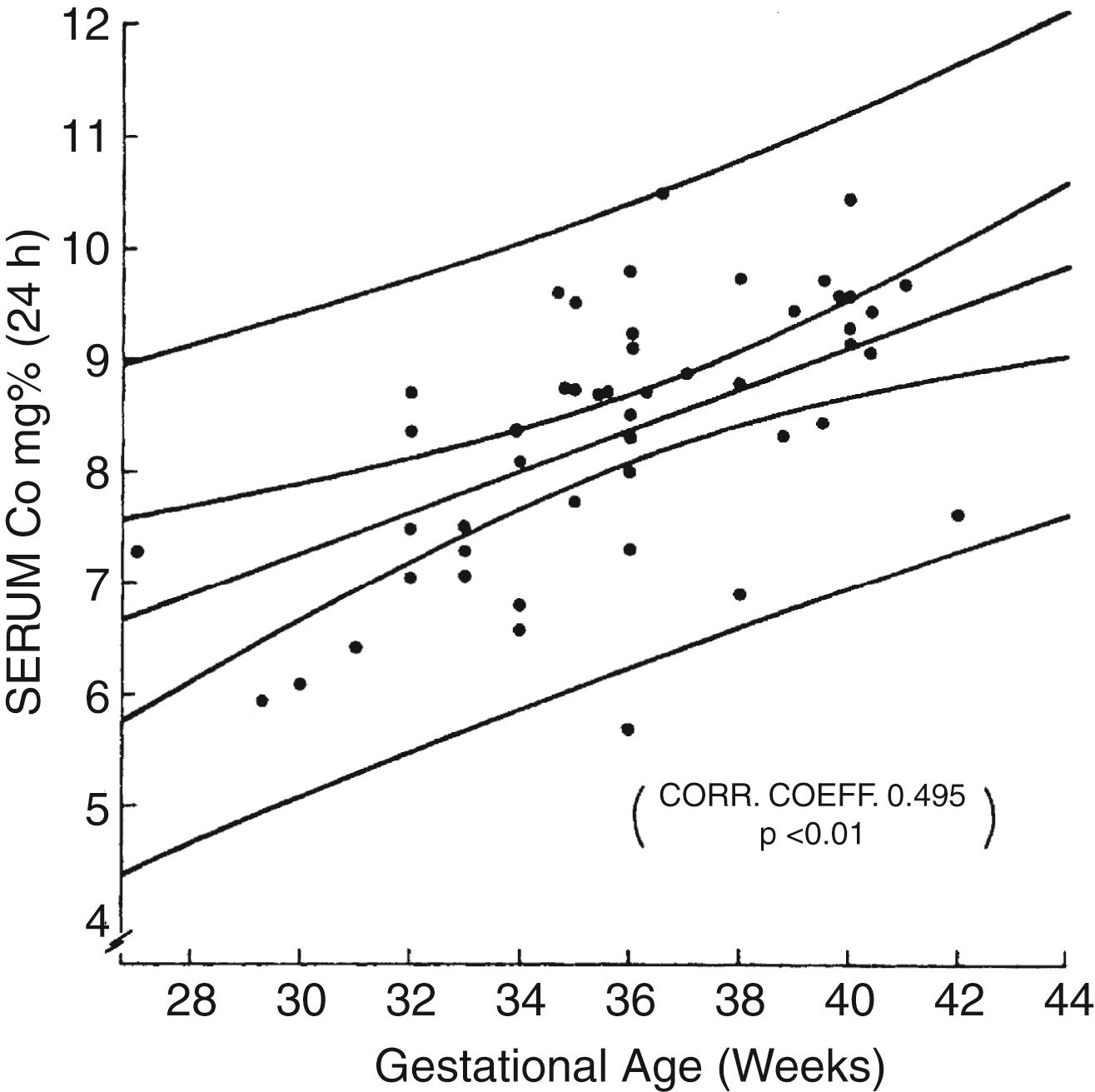
In newborn infants there is a physiologic decline in serum total and ionized calcium during the first 48 hours of life. This decline is exaggerated in preterm infants compared with term infants, with a direct correlation between serum calcium and gestational age ( Fig. 8-1 ). Because no symptoms are specific for early hypocalcemia in preterm infants, the diagnosis is made by demonstrating a serum calcium level below 7 mg/dL (1.75 mmol/L).
Is treatment of hypocalcemia necessary in premature infants?
Calcium therapy may block the normal physiologic adaptation to hypocalcemia, which includes increasing serum levels of parathyroid hormone (PTH) and 1,25(OH) 2 vitamin D in the first few days of life.
Further arguments against the need for the treatment of incidentally noted hypocalcemia in the preterm infant are the following:
Hypocalcemia of prematurity is usually asymptomatic.
It resolves spontaneously.
Long-term follow-up studies have shown no benefit with treatment.
Total serum calcium level is a poor predictor of ionized serum calcium in premature infants.
Intravenous (IV) calcium is associated with complications such as cardiac arrhythmias and ulcerations as a result of soft-tissue infiltration of the infusate. ∗ †
∗ Loughead JL, Tsang RC. Neonatal calcium and phosphorus metabolism. In: Cowett RM, editor. Principles of perinatal-neonatal medicine. New York: Springer-Verlag; 1998. p. 879–908.
† Moya, FR, Laughon, M. Common problems of the newborn. In: Reece EA, Hobbins JC, editors. Clinical obstetrics: the fetus and mother. 3rd ed. Massachusetts: Blackwell; 2008. p. 1247.
When is treatment of hypocalcemia recommended in premature infants?
In the absence of additional data, it is conventional to treat all serum calcium levels below 6 mg/dL, even in asymptomatic neonates. The addition of 200 mg/kg/day of 10% calcium gluconate to standard IV solutions provides 20 mg/kg/day of elemental calcium. If symptoms are present (especially cardiac arrhythmia or seizures), a bolus of 100 mg/kg of 10% calcium gluconate (10 mg/kg elemental calcium) may be given intravenously over 10 minutes with careful cardiac monitoring. One should be cautious using a peripheral IV means to administer calcium because calcium can be very irritating to tissues.
Neonatal hypocalcemia is associated with prematurity, asphyxia, maternal diabetes, transient hypoparathyroidism, permanent congenital hypothyroidism, and (rarely) maternal hyperparathyroidism.
The most common reason for hypocalcemia in the newborn period is prematurity.
Breast milk rickets is seen in premature infants because of the relatively low mineral (e.g., calcium and phosphorus) content of breast milk.
Serum calcium levels are frequently elevated in patients with Williams syndrome.
Normal magnesium levels are needed for optimal functioning of the parathyroid glands.
How can the calcium requirements for premature infants be met by oral feedings?
Recent studies in premature infants using stable isotopes of calcium showed a true calcium absorption rate of 50% to 90%. Thus to meet an accretion rate of 100 mg/kg/day with an absorption rate of 75% and an assumed retention rate of 75% (which may be on the high side), oral intake of calcium for growing premature infants should be about 200 mg/kg/day. This large intake in infants with very low birth weight can be achieved only with special formulas for low-birth-weight infants or mineral fortifiers for breast milk–fed preterm infants. ∗
∗ Tsang RC, Lucas A, Uauy R, et al., editors. Nutritional needs of the preterm infant. Baltimore: Williams & Wilkins; 1993.
How can the calcium requirements for premature infants be met by hyperalimentation solutions?
This problem is much more difficult to address, although intestinal absorption is not a factor. In the early weeks of life with fluid intakes of 150 mg/kg/day, it is difficult to exceed an IV calcium intake of 60 mg/kg/day in the smallest premature infants (weight <1000 g) with standard total parenteral nutrition (TPN) solutions. When the concentration of calcium exceeds 60 mg/dL (3 mEq/dL) in TPN solutions, precipitation with phosphate may occur, depending on variables such as temperature, pH, amino acid content, and even the method by which the nutrients are added to the solution.
What is the pathophysiology of “breast milk rickets” in premature infants?
Clinical rickets develops in preterm infants with very low birth weight who are fed human milk not fortified with minerals and vitamins. Typically, the disease presents after 8 weeks of life with severe hypophosphatemia, “relative hypercalcemia,” and hypercalciuria. The x-ray findings mimic those of rickets resulting from vitamin D deficiency. The biochemical findings are the result of low mineral intake. Because human milk is low in both calcium and phosphorus, the very low phosphorus intake (about 50% of calcium intake) severely limits deposition of calcium in bone.
Caution: Because treatment with phosphorus alone can result in severe hypocalcemia, supplements of both minerals are imperative.
What is the differential diagnosis of the etiology of a hypocalcemic seizure in a 14-day-old term infant?
Seizures secondary to hypocalcemia are very unlikely in a previously healthy term infant at 2 weeks of age. The differential diagnosis includes late infantile tetany associated with high phosphate load (e.g., feedings with cow milk), acid–base disturbances caused by diarrhea treated with alkali therapy, and congenital hypomagnesemia (rare).
What is the appropriate therapy for a hypocalcemic seizure in a 14-day-old term infant?
Treatment of hypocalcemic seizures is the same for both premature and term infants. In general, 10% calcium gluconate containing 9.4 mg/mL of elemental calcium is the drug of choice. The usual dose of 2 mL/kg body weight (18 mg/kg of elemental calcium). Infusion should occur slowly over the course of 10 minutes with heart rate monitoring. Make sure the line is patent before infusing calcium.
How many fractions of calcium are found in the serum? Which can be measured in the clinical laboratory?
There are three fractions of calcium in serum: ionized calcium (50%), calcium bound to serum proteins (40%), and calcium complexed to serum anions (10%). Ionized calcium and total calcium can be measured in most hospital laboratories.
What are the normal serum calcium values in term infants?
Normal values (in milligrams per deciliter, expressed as mean± standard deviation and range) depend on chronologic age and laboratory variation (to a lesser degree):
Cord: 10.2 +/− 0.6 (9.3–11.7)
2 hours: 9.7 +/− 0.6 (8.8–11.3)
24 hours: 9 +/−0.6 (7.8–10) ∗
∗ Loughead JL, Mimouni F, Tsang RC. Serum ionized calcium concentrations in normal neonates. Am J Dis Child 1988;142:516–18.
What are the normal serum values in preterm infants?
Normal values (in milligrams per deciliter, expressed as mean ± standard deviation and range) depend on gestational age:
23–27 weeks: 10.0 +/−1.0 (8.1–11.9)
28–31 weeks: 10.2 +/−1.2 (8–12.5)
32–34 weeks: 10.5 +/−1 (8.6–12.4)
35–36 weeks:10.4 +/−1.1 (8.3–12.5)
>36 weeks: 10.9 +/−0.5 (9.8–11.9) ∗
∗ Fenton TR, Lyon AW, Rose MS. Cord blood calcium, phosphate, magnesium, and alkaline phosphatase gestational age-specific reference intervals for preterm infants. BMC Pediatr 2011;11:76.
List the manifestations of hypercalcemia in neonates.
Lethargy
Irritability
Polyuria
Vomiting
Constipation
Failure to thrive
What values “define” hypercalcemia in newborn infants?
Total serum calcium above 10.8 mg/dL or ionized serum calcium above 5.4 mg/dL.
What are some of the causes of hypercalcemia in neonates?
Iatrogenic hypercalcemia
Subcutaneous fat necrosis
Idiopathic infantile hypercalcemia
Williams syndrome
Hyperparathyroidism (primary and secondary)
PTH-related peptide tumor
Hyperprostaglandin E syndrome
Hypophosphatasia
Familial hypercalciuric hypercalcemia
Blue diaper syndrome
Thyrotoxicosis
Vitamin A intoxication
Chronic thiazide toxicity
Excessive maternal intake of vitamin D
How is acute hypercalcemia managed in newborn infants?
Promote diuresis by administering IV fluids (normal saline).
Administer furosemide, and monitor serum electrolytes carefully only after adequate hydration is given.
Hydrocortisone (1 mg/kg every 6 hours) is of value only in chronic situations to reduce intestinal absorption of calcium.
In severe cases dialysis may be required to lower calcium levels while the patient is awaiting definitive treatment of the underlying cause. ∗
∗ Bachrach LK, Lum CK. Etidronate in subcutaneous fat necrosis of the newborn. J Pediatr 1999;135:530–1.
A 3-day-old infant born small for gestational age at term has a total serum calcium level of 13.2 mg/dL. She was delivered by emergency cesarean section and was diagnosed with supravalvular aortic stenosis. What is the likely diagnosis?
Williams syndrome is the likely diagnosis in an infant with hypercalcemia and supravalvular stenosis who was born small for gestational age. It results from a deletion of the elastin gene on 7q11.23. Affected infants are often described as having “elfin” faces. ∗
∗ Pohlenz J, Van Vliet G. Developmental abnormalities of the thyroid. In: Weiss RE, Refetoff S, editors. Genetic diagnosis of endocrine disorders. Amsterdam: Academic Press/Elsevier; 2010. p.101.
A term infant is incidentally noted to have a calcium level of 12.2 mg/dL at 4 days of age. Family history reveals that the father has also been evaluated for elevated calcium levels. What would you expect to find on measurement of the infant’s urinary calcium level? What is the most likely diagnosis? What is the appropriate therapy?
The most likely diagnosis is an autosomal dominant mutation of the calcium-sensing receptor, or “hypocalciuric hypercalcemia.” The infant’s urinary calcium level will be inappropriately low for the serum calcium. In the heterozygous state this is generally thought to be a benign condition, and treatment is not indicated. Rare cases of homozygous mutations result in severe neonatal hyperparathyroidism, which is a life-threatening disorder. ∗
∗ Hsu SC, Levine MA. Perinatal calcium metabolism: physiology and pathophysiology. Semin Neonatol 2004;9:23–36.
Why is the diaper blue in blue diaper syndrome?
A defect in the intestinal transport of tryptophan causes excretion of blue, water-insoluble tryptophan metabolites. The reason that these children have high calcium levels is not well understood.
How are millimoles (mmol) of magnesium converted to milliequivalents (mEq) and milligrams (mg)?
What two types of magnesium reactions are important in human physiology?
Intracellular and extracellular types of magnesium reactions are important.
What is the role of magnesium in intracellular reactions?
Magnesium is the second most abundant intracellular cation after potassium and helps to regulate cellular metabolism. As part of the magnesium-adenosine triphosphate complex, it is essential for all biosynthetic processes, including glycolysis, formation of cyclic adenosine monophosphate, and transmission of the genetic code. In addition, any reaction that uses or produces energy requires magnesium.
What are the extracellular reactions that involve magnesium?
Only 1% of magnesium is contained in extracellular fluid. However, extracellular concentrations are critical for maintenance of electric potentials of nerve and muscle membranes and for the transmission of impulses across the neuromuscular junction. Magnesium and calcium may act synergistically or antagonistically in many of these processes.
What causes magnesium depletion in neonates?
Maternal diabetes
Maternal magnesium deficiency
Renal losses of magnesium in acidotic states
Use of nutrient solutions containing insufficient amounts of magnesium
Renal tubular defects
Intestinal wasting of magnesium (rare X-linked condition)
Gastrointestinal losses (through emesis, nasogastric suctioning, and diarrhea)
Prematurity, which increases the risk for magnesium deficiency
Intrauterine growth retardation ∗
∗ Rubin LP. Neonatal disorders of serum magnesium. In: Taeusch HW, Ballard RA, editors. Avery’s diseases of the newborn. 7th ed. Philadelphia: Saunders; 1998. p. 1189–1206.
What are the signs and symptoms of magnesium deficiency in neonates?
Most infants are asymptomatic. On rare occasions the following signs and symptoms may be seen:
Color: pallor, cyanosis, or duskiness
Affect: out of touch with surroundings, apathetic, irritable when disturbed, restless
Eyes: staring with infrequent blinking, oculogyric crises
Heart: tachycardia (bradycardia during apneic episodes)
Respiration: brief apnea, sometimes followed by tachypnea
Neuromuscular system: motor weakness, transient spasticity, abnormal reflexes; if hypocalcemia develops (discussed later), the infant may show signs associated with calcium deficiency, including seizures
What are the effects of hypomagnesemia on calcium homeostasis?
Hypomagnesemia usually increases the secretion of PTH, thereby increasing calcium levels. In chronic magnesium-deficient states, however, secretion of PTH is reduced. In such circumstances hypomagnesemia may induce hypocalcemia. ∗
∗ Spiegel, DM. Normal and abnormal magnesium metabolism. In: Schrier RW, editor. Renal and electrolyte disorders. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2010. p. 240.
What causes hypermagnesemia in neonates?
Maternal treatment with magnesium (for preeclampsia or tocolysis)
Excessive magnesium administration to neonate (e.g., TPN, antacids, treatment of pulmonary hypertension)
How should hypomagnesemia be treated parenterally?
Hypomagnesemia usually is treated intravenously or intramuscularly with a 50% solution of magnesium sulfate.
One milliliter of a 50% solution contains 4 mEq of elemental magnesium. The usual dose is 0.1 to 0.25 mL/kg/day.
Serum magnesium levels should be monitored every 12 hours.
What are the signs of hypermagnesemia in neonates?
Flaccidity
Unresponsiveness
Respiratory insufficiency
Apnea (especially when aminoglycoside antibiotics are used concurrently)
Ileus
Delayed passage of meconium
In extreme cases cardiorespiratory function ceases, and death ensues.
How is hypermagnesemia treated?
Stop the administration of magnesium.
Make sure the infant is well hydrated.
Consider diuretic therapy.
In severe cases exchange transfusion (with acid-citrate-dextrose solution) is effective.
The effects of calcium salts are equivocal.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here