Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The transport of combat casualties by air parallels the history of military aviation. Although many texts cite balloon transport during the Franco-Prussian War (1870) as the first instance of aeromedical evacuation (AE), the true initiation of AE awaited the successful development of the fixed wing aircraft. During World War I (1914–1918) British, French, German, and American forces all utilized fixed wing evacuation on a limited basis. These first AEs provided the opportunity to overcome the “tyranny of distance” facing the movement of a casualty. The introduction of flight evacuation during World War I offered the advantage of speed and time while avoiding the arduous, and often dangerous, task of ground evacuation via carriage or the rudimentary gas-powered vehicles of the era.
During World War II (1939–1945), more than 1 million injured combatants would be evacuated by British, American, and German aircraft. AE at this time was largely reserved for stable or ambulatory casualties, those previously managed for weeks to months following injury at established rear hospital facilities who were sufficiently recovered enough to sustain (and survive) the rigorous transport process in unpressurized aircraft.
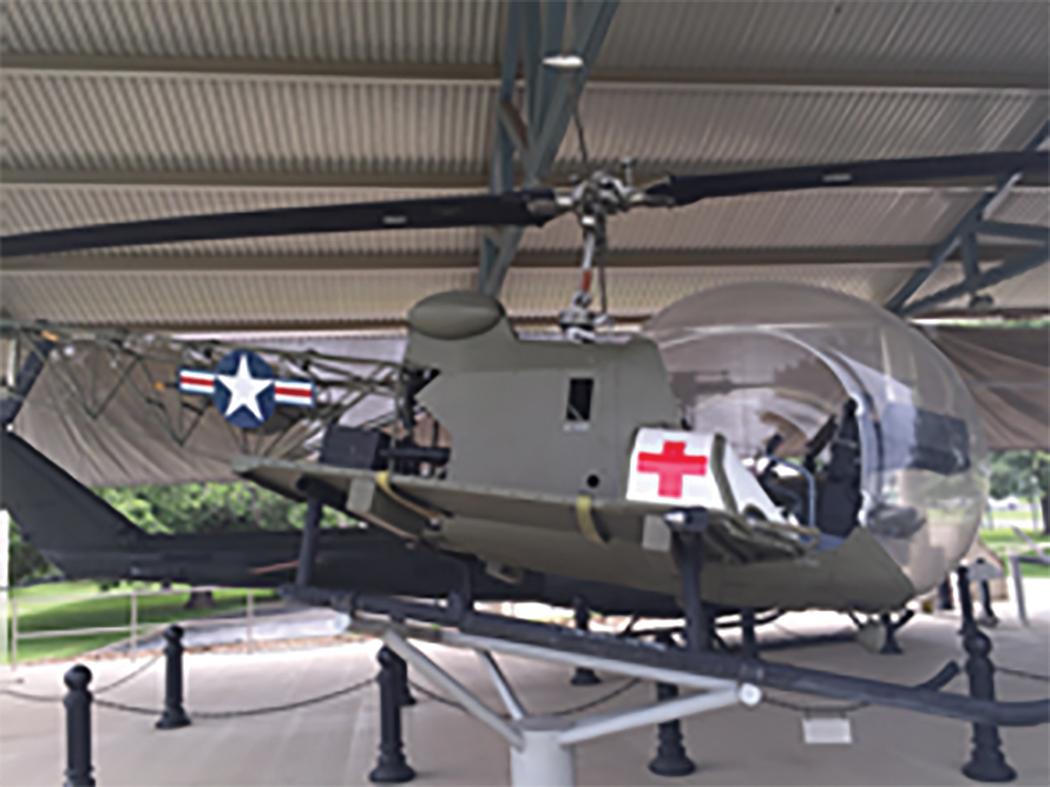
The Korean War (1950–1953) was the first to demonstrate the advantages of rotary wing evacuation and its ability to clear casualties from the forward area of battle. The introduction of helicopter evacuation expanded the utility of aeromedical care into the far-forward prehospital care and expedited the clearance of casualties from battle. The venerable OH-13 Sioux helicopter ( Fig. 1 ) proved to be an invaluable resource, evacuating wounded soldiers over the inhospitable and mountainous terrain of Korea. Combat casualties were delivered to nearby mobile army surgical hospital units within minutes of injury rather than hours or days. In this first-generation MEDEVAC platform, the patient was loaded on a litter outside the cockpit, attached to either of the landing skids. There was no opportunity for en route care and the intent was to only facilitate the rapid evacuation of the casualty.
The role of rotary wing evacuation become even more preeminent during the U.S. combat role in the Vietnam War (1954–1975). The widely visible success of the US Army’s MEDEVAC units (call sign DUSTOFF) in clearing casualties and providing rapid delivery to definitive trauma care hospitals would be widely copied by the civilian trauma system then developing in the United States (1970–1980). The Vietnam DUSTOFF era is also recognized as the first time when rudimentary medical care (hemorrhage control and fluid administration) was delivered by medics while en route from the point of wounding to first level of surgical care. At this time, the algorithm for fluid resuscitation emphasized only crystalloid administration in the transport process as a result of misinterpreted research data from the 1960s.
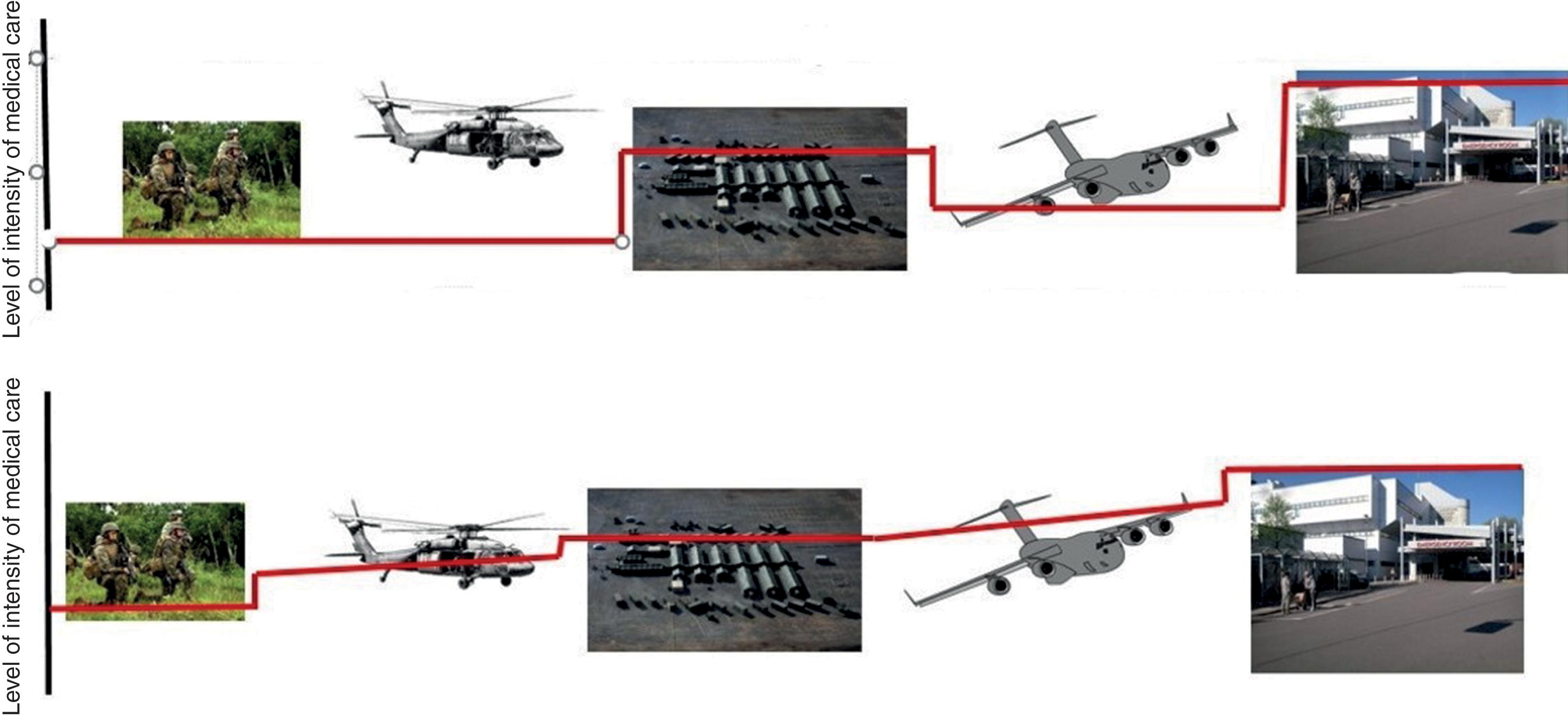
The model of AE developed following Korea through the First Gulf War (1990–1991) consisted of a dichotomous, two-step process. The first step of AE entailed forward (tactical) evacuation of casualties from the point of injury to an established surgical unit and was accomplished via rotary wing transport. The focus of this initial phase was rapid transport out of a hostile/combat environment. En route care was not a primary objective and was rudimentary at best. After arriving at more established facilities (mobile or theater surgical facility), the casualties would undergo treatment and would recover until sufficiently stable to tolerate the second phase of the process. This second phase of AE (strategic evacuation) consisted of transport of the wounded over much greater distances using fixed wing aircraft.
This chapter examines the continued evolution of AE process over the last two decades, throughout the Global War on Terror (2001–present), Operation Iraqi Freedom (OIF) (2003–2011), Operation Enduring Freedom (OEF) (2001–2014), and beyond. This evolution has transformed AE from a strictly transportation-focused process to a process that weighs provision of critical care and rapid transport equally and strives to perform them simultaneously. The ideal system sought is a continuum of care beginning at the point of injury coupled with precipitous movement capabilities, delivering casualties to increasingly capable facilities across echelons of care. There is a continued movement to change the lexicon from the various terms such as MEDEVAC/CASEVAC/TACEVAC to a more inclusive description such as en route care. The concept of en route care embraces the totality of patient movement from the forward edge of battle through the continuum of theater care and onward to return to the continental United States and finally, reintegration into stateside hospitals. En route care encompasses the movement of the injured through time and space via various means of conveyance (air, ground, and sea). The challenge to be met is to ensure that the provision of medical care to the injured soldier remains continuous and comparable to the ground-based combat medical treatment facilities. In the past the movement of a casualty often meant that the intensity of care and observation fell while in transport. Today’s military concept of en route care endorses the delivery of care equal to, or exceeding, that of the sending facility while moving the casualty to the next locus of care. The ability to provide high-intensity and continuous monitoring and care while in the challenging and austere movement space is the crux of the mission ( Fig. 2 ).
Review of medical care delivery during the First Gulf War resulted in a focused assessment of the ability of the Military Health Service to provide medical support for combat operations. Following the Vietnam War and up until the First Gulf War, the Military Health Service had reverted to a large and bulky footprint of forward medical care based upon a projected conflict in the European theater. Large combat support hospitals required significant air cargo support and often took weeks to months to assemble. Medical assets positioned to support the advance of soldiers into Kuwait rapidly found themselves out of reach of the rapidly advancing mechanized infantry. Analysis of the medical support to Desert Storm recognized that medical doctrine had failed to remain abreast of asymmetrical warfare and the rapid employment of mobile fighting forces. There was a call to return to the lessons manifested in every previous battle; namely, that the medic must remain in close proximity to the soldier they support.
The need for restructuring of AE into a more sophisticated and continuous process of en route critical care was highlighted during the peacekeeping mission in Mogadishu (“Black Hawk Down”—October 1993). A critically injured soldier required strategic evacuation to the military medical facility in Germany. However, at this time, the U.S. Air Force (USAF) and its AE policy had not yet adapted to the movement of critically ill combat casualties. This capability shortfall was recognized on the tarmac of the airfield by the Army surgeons accompanying their patient to the airfield, requiring one of the surgeons from the Army facility to accompany the patient to Germany. Shortly after this mission departed Mogadishu, the 75th Ranger regiment became engaged in a firefight that resulted in 18 deaths and 73 wounded, while one of the three surgeons assigned to the Army’s Mogadishu Forward Surgical Team was en route to Germany, resulting in medical facility that was understaffed during a mass casualty. This review was presented to the Military Health Service and the USAF and gave rise to two key principles in the foundation of modern military en route care. First, that an AE team could provide en route critical care to a surgically temporized but not necessarily stabilized patient. Second, that the en route care team had to be self-sustaining with respect to personnel and equipment, so as to not strip critical elements of manpower or equipment from the far-forward surgical resuscitation teams.
Over the ensuing decade of the 1990s medical doctrine was realigned to emphasize mobility and proximity of surgical support to an increasingly agile and mobile fighting force. The realignment emphasized a return to small, mobile surgical teams capable of rapidly following the front and providing means of surgical stabilization in far-forward and austere settings. During the early phases of OIF and OEF, the proximity and capabilities of these robust surgical support teams (U.S. Army Forward Surgical Team, US Navy Forward Resuscitative Surgery Service, U.S. Air Force Mobile Forward Surgical Team) resulted in the salvage of critically injured soldiers with practices such as whole blood transfusion, permissive hypotension, and damage control surgery. However, this initial resuscitation and intervention created a new kind of patient—one whose injuries had been surgically temporized but was far from medically stable for traditional evacuation. These were patients who would have previously died at the point of injury, succumbed while en route, or died at a far-forward battalion aid station. Supporting these critically ill, surgically stabilized patients necessitated either moving intensive care unit (ICU) resources and facilities to every far-flung resuscitation team (a notion not logistically or practically possible) or formulating a proficient method of moving critically ill patients through time and space in a combat theater of operation. En route care and the USAF’s Critical Care Air Transport Teams (CCATs) were the solution to this dilemma.
The USAF set about the process of formulating a solution that would address the evolving AE requirements, as the USAF is doctrinally responsible for the strategic movement of wounded combatants of all branches. The CCAT was developed as a solution to the identified capability gaps brought about by the changing nature of conflict in the 21st century. In past conflicts AE movement was a process of providing transport with concomitant basic medical support for casualties. The new paradigm challenge facing the CCAT process was to prepare, and assume responsibility for, the provision of uninterrupted intensive care for critically ill soldiers from the furthest forward and austere location to the rearward area(s). It was no longer acceptable to simply ensure the safe transport of the casualty to the next point of care. The challenge was to ensure that the acuity of care did not suffer as a result of the transport process or environment. The goal was to match the intensity and capability of the far-forward resuscitation surgical teams and continue the process of stabilization and intensive medical care while simultaneously moving the patient across distances small or great. ICU care was no longer the sole domain of ground-based theater facilities. Now CCAT teams were charged with ensuring the uninterrupted provision of critical care and patient optimization throughout the continuum from point of injury to return to the continental United States.
The original concept and first CCAT teams were developed in the early 1990s at Wilford Hall Medical Center, San Antonio, Texas. The original intent of the teams was to provide effective and capable means of transporting care-eligible active duty, dependent, and retirees from outside civilian ICUs throughout the United States back to Wilford Hall Medical Center. The opportunity to evolve these teams as a key element of the concomitant reengineering of combat medical care capability was recognized by Lieutenant General P.K. Carlton Jr. (USAF/SG retired). Over the next decade, the CCAT process would grow from concept to accepted doctrine under the vigilant leadership of Lieutenant General Carlton (17th Surgeon General of the USAF) along with a handful of young AF Medical Service officers.
By September 11, 2001, the CCAT mission was a recognized component of the larger AE movement process but still largely an untested concept. Combat operations following 9/11 were the first large-scale tests of the CCAT operations. The initial years of combat casualty care (2001–2004) provided many challenges, and the program evolved to meet the needs of combat medical operations as they came to light. Medical facilities in the combat zone(s) of Iraq and Afghanistan were varied in size and shape and were frequently relocating to remain in close proximity to the combat units they were supporting. Initially deployed CCAT teams were positioned at major air hubs to include Landstuhl Regional Medical Center (Germany) or Al Udeid Air Base (Qatar). CCAT teams would fly “downrange” into theater onboard strategic cargo aircraft and assume responsibility for the stabilization and subsequent return transfer of patients from the forward deployed facilities to larger hospitals. As numbers of casualties increased and theater medical facilities matured, CCAT teams were eventually forward embedded at the location of major medical facilities in the theater of operations (Balad Air Base Iraq, Bagram Air Base Afghanistan, and the Navy hospital in Kandahar). By 2005, a significant number of CCAT teams were deployed to these various facilities within the theater of operations. The forward positioning of CCAT teams provided the advantage of additional critical care personnel at the theater medical facilities as well as a knowledge base of how to prepare and position a critically ill patient in anticipation of a long-range CCAT transport.
The challenge for the CCAT teams was to sustain the high level and intensity of medical care that was being delivered in the forward facilities throughout the transport process. In some cases, this meant the provision of critical care for a relatively short time (1–2 hours) during an intratheater transport onboard a C-130 Hercules cargo plane ( Fig. 3 A and B). In most cases it meant providing critical care throughout strategic, overnight, intercontinental flights from theater in Iraq or Afghanistan to Landstuhl Regional Medical Center in Germany (8–12 hours). The CCAT missions were flown onboard various cargo aircraft such as the C-141 (now retired from inventory), the C-130, the C-17, or the KC-135 tanker. Over the course of combat operations, the time window to CCAT movement would be increasingly shortened as experience was gained. By 2006 it was common for a wounded casualty to undergo one to two surgical stabilization procedures in theater and subsequently be transported to Germany within 30 to 36 hours.

In effort to understand the primary mission profile of CCAT teams in patient movement during recent conflicts in Iraq (OIF) and Afghanistan (OEF), one must first describe how patients transition through five defined “roles” of care at the military treatment facility beginning at the point of injury. They are listed as:
Role I—self-aid and buddy care
Role II—battalion aid station or forward surgical team
Role III—combat support hospital
Role IV—established military treatment facility outside of the Theatre of Operations (Landstuhl)
Role V—military treatment facility in the United States (Walter Reed National Military Medical Center, Brooke Army Medical Center)
As described, CCAT teams were designed to care for the “stabilized” (but not necessarily stable) patient. Patients were “stabilized” at the Role II and Role III facilities as defined by four specific criteria. The casualty must have a stable or definitive airway, all fractures immobilized, active hemorrhage controlled, and resuscitation initiated. CCAT teams were deployed to the role III hospitals within the theater of operations so that they could be quickly activated in the event that patients required movement through the AE system. With the robust trauma system present in OEF/OIF, CCAT teams could obtain resources from the Role III hospital before prolonged intertheater transport including medications from the pharmacy as well as blood products to increase their capabilities beyond the base allowance standard. Standard missions of CCAT teams included:
Intratheater Role II to Role III missions, primarily on C-130s by teams based at the deployed Role III;
Intertheater Role III to Role IV missions, primarily on C-17s by teams either based at the deployed Role III or teams located at the Role IV;
Intertheater Role IV to Role V missions, primarily on C-17s by teams based at the Role IV hospital.
The composition of a CCAT team includes a physician, a nurse, and a respiratory therapist. This three-person team can be tasked with caring for up to six spontaneously breathing critically ill patients or up to three mechanically ventilated critically ill patients. Although members of the team come from various medical education backgrounds, emphasis is placed on learning and understanding all roles. This includes mastery of all equipment and a baseline fund of knowledge to ensure redundant training within the group. Each member of the team is expected to possess the ability to function independently, across the entire spectrum of care to guarantee the safe movement of the patient. This unique cross-functional capability is a reflection of operational realities that may require the team to split for periods of the transport when moving multiple patients. Overall, a well-constructed team includes a mix of skill, strong team dynamics, and a high level of situational awareness.
The physician functions as team leader, assuming medical responsibility for each patient being transported. The CCAT physician role requires critical care competencies and can include physicians trained in the specialties of emergency medicine, anesthesia, pulmonary critical care, cardiology, or general surgery. Regardless of background training, clinical currency in the care of critically ill patients remains essential to provide the degree of support necessary to establish stabilization prior to transport and to perform critical interventions while en route (see training requirements described later). In addition to the baseline medical knowledge required, the physician must also maintain operational and situational awareness to anticipate and reduce the occurrence of clinical incidents in an austere and ever-changing environment of care.
The CCAT nurse fills a vital role in the transport team, continually assessing the patients, performing diagnostic tests, administering treatments, and assisting the physician or respiratory therapist with any invasive procedures. The majority of CCAT nurses are registered nurses with critical care training that have experience caring for critically ill patients on a daily basis. However, this role can also be filled by advanced registered nurse practitioners and certified registered nurse anesthetists. The nurse must be current in Advanced Cardiac Life Support; have worked in a critical care or special care unit, emergency department, or postanesthesia care unit within 2 years of selection; and have a minimum of 1 year of experience. Trauma Nursing Core Course is highly encouraged but not required.
The CCAT respiratory therapist fills the final essential role on the team assessing the pulmonary function of patients and determining appropriate therapy or treatment options. For mechanically ventilated patients, the CCAT respiratory therapist manages the transport ventilator and is responsible for knowing all aspects of its functions and operations. In addition, the respiratory therapist functions as the “medical mechanic” for the team, with a thorough understanding of all the equipment and the ability to troubleshoot malfunctions smoothly during transport. In order to be selected, this member must have 1 year of critical care experience, must receive annual training in an ICU, and must have worked with ventilated patients within the past year.
CCAT training begins with the assumption that the provider entering the training pipeline is clinically current and competent in the environment and delivery of critical care. The goal of the course is not to develop the existing critical care skill set of the team member, but rather to teach providers how to adapt their clinical skills to the en route care environment. This requires understanding that CCAT is an austere environment where resources and therefore capabilities are limited, sensory stimuli normally relied upon in hospital settings are nonexistent thanks to noise and poor lightning, and physiologic changes can occur in patients secondary to altitude. The impacts of these limitations must be recognized, understood, and compensated for by the provider to ensure seamless care for the casualty (see environmental considerations, discussed later).
CCAT training starts with selection of the team members from the various clinical specialties. Members selected are commissioned officers and enlisted personnel from Active Duty, Air National Guard, or Air Force Reserve Command components of the USAF. Once chosen, the member must successfully complete two separate training courses prior to receiving the qualification to fly operational CCAT missions. All CCAT providers go through an identical training pipeline allowing members to be interchangeable between teams as operational circumstances dictate. While maintaining a consistent three-member team throughout a deployment is ideal, the ability to spontaneously replace a member of the team when necessary (i.e., in illness or unanticipated emergencies) allows for operational flexibility.
The CCAT Initial Course is a 10-day curriculum designed to prepare CCAT providers to meet the wartime and peacetime missions of caring for critically ill and injured patients in flight. The course takes place at the U.S. Air Force School of Aerospace Medicine located at Wright-Patterson Air Force Base in Ohio. The focus of the initial course is the AE mission, environment, aircraft, equipment, and an introduction to altitude physiology including familiarization with hypobaric medicine and dives in a hypobaric chamber. The curriculum also focuses on developing an ingrained familiarity with the allowance standard (soft goods and medications) and patient movement items (equipment). Emphasis is placed upon patient preparation and the ability to anticipate and intervene in physiologic events that may occur as a result of the patient’s preexisting condition or secondary to the rigors of the en route movement. Extensive simulations scenarios in aircraft fuselages augment familiarity with the mission and environment. Members also receive an introduction to the Joint Trauma System Clinical Practice Guidelines and receive training on how to adapt their baseline clinical skills to both the deployed as well as en route environment.
The second course is the CCAT Advanced Course held at the University of Cincinnati Medical Center in Cincinnati Ohio, home to USAF Cincinnati CSTARS (Center for Sustainment of Trauma and Readiness Skills) and one of five designated Military-Civilian Partnership facilities. The advanced course builds on the concepts introduced during the CCAT Initial Course and emphasizes core critical care principles routinely encountered in the deployed environment, delivery of care, and understanding the treatment goals within the context of the Clinical Practice Guidelines. The CCAT Advanced Course is unique among military courses in terms of its flexibility and ability to rapidly adjust course content to real-world operations. A significant effort is devoted to teaching lessons learned from current real-world CCAT missions. Students and instructors join in on the weekly video teleconference call from the theater to maintain situational awareness of current operational challenges. To ensure timely and relevant mission scenarios, the instructor cadre stationed at the university program routinely deploy into theater as part of a continuous deployment model. As a clinically focused course, cadres have the discretion to adjust course material to ensure it is reflective of current operations with the aim of optimally preparing students for down range. These efforts make the CCAT Advanced Course is unique among military courses in terms of its flexibility and ability to rapidly adjust course content to real-world operations.
The hallmark of the CCAT Advanced Course is the application of high-fidelity simulation, immersing teams in training into real-world patient care scenarios. High-fidelity mannequins reside in a training center designed to replicate the cabin of a C-130, complete with low light and deafening aircraft noise. The simulator center and scenarios are intended to provide a realistic and lifelike training environment where the provider team must effectively manage challenging clinical scenarios. Over the 2-week period of the advanced course, CCAT student teams will spend over 10 hours in simulated flights and medical scenarios that emphasize not only medical management but also crew resource management. During the second week, students and their instructors will participate in a full-day scenario that includes transportation of simulated patients by ambulance bus to a nearby airport. Once at the airport the teams continue to monitor and prepare their patients for fixed wing evacuation. An Air Force C-130 Hercules from the Kentucky Air Guard meets the teams at the airport and enplanes the teams and their instructors for a flight modeling a realistic mission profile ( Figs. 4 and 5 ).


The CCAT Advanced Course teams are evaluated in their ability to provide safe and effective care during these high-fidelity simulated clinical scenarios. Providers who are unable to demonstrate the ability to effectively deliver care in the austere en route environment do not validate the course and are not eligible for deployment as a CCAT provider. Students are given recommendations on opportunities to further develop their skill set and offered the opportunity to participate in a future advanced course. Recurrent training is required to remain qualified for CCAT deployment and each member is required to attend and validate the CCAT Advanced Course every 36 months. Overall, the rigorous selection and training process ensure that only the most qualified health care professionals are tasked with the responsibility of transporting our wounded soldiers, sailors, airmen, and marines.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here