Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
Discuss the advantages and disadvantages of sonography for the trauma patient
Define the goal of sonography in the assessment of blunt trauma
Describe the protocol for focused assessment with sonography for trauma (FAST)
Describe the sonographic findings for aortic dissection, right upper quadrant pain, free fluid in the abdominopelvic region, acute pelvic pain, and scrotal trauma and torsion
Identify the modalities commonly used to evaluate flank pain
Sonography is well recognized as a powerful and efficient tool for the diagnosis and evaluation of the patient in the emergency department (ED). The development of smaller ultrasound equipment and improvement in transducer technology have enabled the sonographic examination to extend beyond the imaging departments and be especially prevalent in the ED. The implementation of educational curriculum changes in specialized residency programs and specialty practice has facilitated the integration of focused ultrasound into specific emergent settings. In emergent and critical situations, the ED team must be able to efficiently and accurately assess the patient’s problem, and sonography is a tool that allows the team to quickly evaluate the patient.
The most common reasons people go to the ED include trauma, acute chest pain, shortness of breath, hypotensive events, acute abdominal or pelvic pain, syncope, extreme nausea and vomiting, lacerations, and broken bones.
The primary focus of this chapter is to cover the more common emergent abdominal procedures that the sonographer is likely to encounter in a call-back situation from the ED. The ED resident or emergency physician may have already performed a rapid survey of the area of interest and may call for a “formal or complete” ultrasound evaluation if further information is needed. Potential life-threatening emergencies such as abdominal emergencies, internal hemorrhage following blunt trauma, ectopic pregnancy, pericardial tamponade, and ruptured aortic aneurysm may be rapidly assessed with sonography.
The assessment of the abdomen for possible sustained abdominal injury caused by blunt abdominal trauma is a common clinical challenge for physicians and emergency medicine physicians. The physical findings may be unreliable because of the state of patient consciousness, neurologic deficit, medication, or other associated injuries.
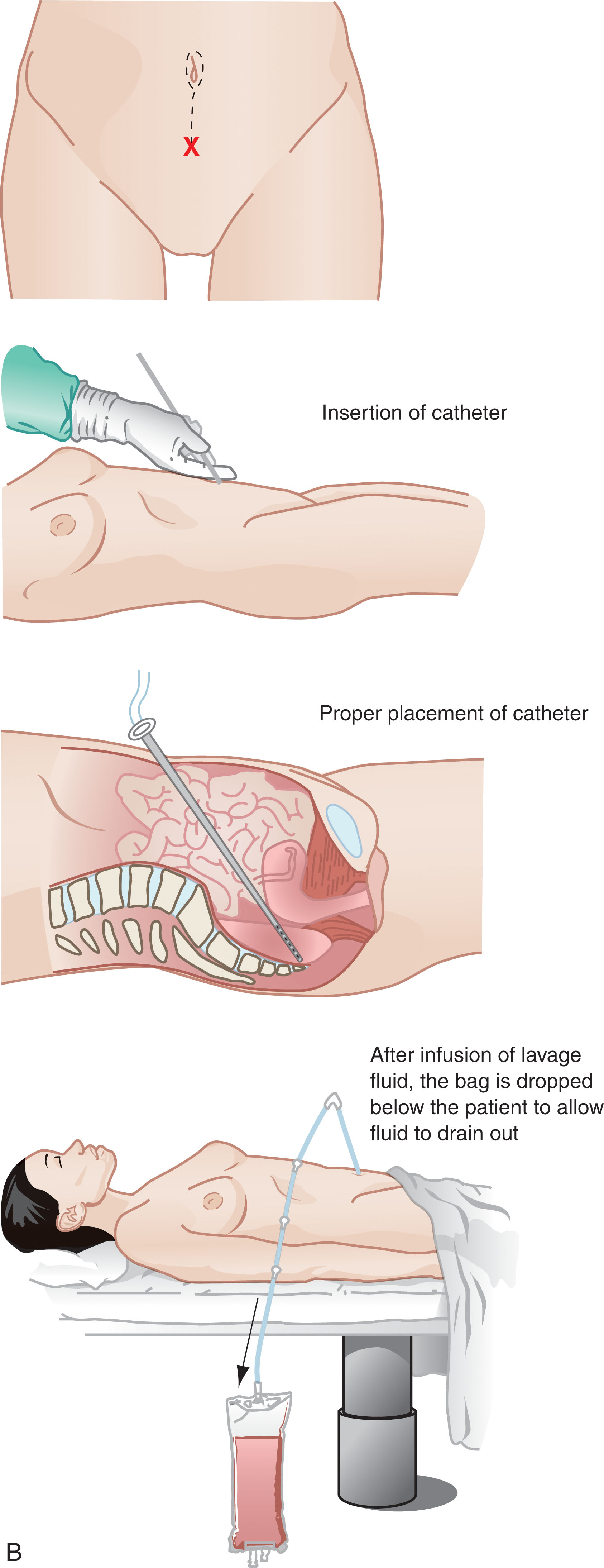
Diagnostic peritoneal lavage (DPL) was used to sample the intraperitoneal space for evidence of damage to the viscera and blood vessels in patients with blunt abdominal trauma to decide which patients needed exploratory laparotomy. For this procedure the patient is placed in the supine position and the urinary bladder is emptied by catheterization. The patient’s stomach is emptied by a nasogastric tube because the distended stomach may extend to the anterior abdominal wall. The skin is anesthetized, and a small vertical incision is made. The incision is made either in the midline or at the paraumbilical site, with multiple layers of tissue penetrated before the parietal peritoneum is located ( Fig. 19.1 ). Although peritoneal lavage has been used successfully to assess abdominal injuries, it is an invasive procedure that takes at least 10 to 15 minutes and that carries a risk of bowel perforation, bladder penetration, vascular laceration, and wound complications. This procedure has been inappropriate for alert patients in stable condition, who represented the majority of patients with blunt abdominal trauma. Peritoneal lavage decreases the specificity of subsequent ultrasonography or computed tomography (CT) because of the introduction of intraperitoneal fluid and air.
CT remains the radiology standard for investigating the injured abdomen but requires patient transfer and inevitable delay (bowel preparation). CT is usually performed in patients in whom intra-abdominal injury is strongly suspected. Other indications for CT include equivocal findings of abdominal examination in stable patients, persistent abdominal pain, and decreasing hematocrit. CT is unsuitable for patients who are clinically unstable. The time required to complete a CT scan is variable; however, the sensitivity and specificity is high to detect fluid collections.
The clinical utilization of sonography in the evaluation of blunt abdominal trauma (BAT) has existed in Europe and Asia since the 1970s ( Box 19.1 ) North America and the United Kingdom did not incorporate its use until the 1990s. The development of smaller ultrasound systems and improved transducer technology have made this application grow. Using sonography as a screening procedure involves many factors that will be fast, accurate, portable, and noninvasive. A rapid survey with sonography may be made in less than 4 minutes. Disadvantages include the presence of subcutaneous or intra-abdominal air and obesity. Sonography is now well established as a noninvasive and easily repeatable tool to image many areas of the body.
Hemodynamically Unstable Patient
Determine if intraperitoneal fluid is present
Exploratory laparotomy is indicated for patients with positive DPL or FAST exam
Consider other sites of blood loss or nonhemorrhagic shock (repeat FAST or DPL)
Hemodynamically Stable Patient
FAST examination to determine presence of intraperitoneal fluid
CT scan
Focused assessment with sonography for trauma (FAST) has become an extension of the physical examination of the trauma patient. This is a focused survey examination of the abdomen, pelvis, and pericardium to evaluate free fluid or pericardial fluid ( Fig. 19.2 ). The FAST exam is performed in the ED by properly trained and credentialed staff. In the context of traumatic injury, the timely diagnosis of potentially life-threatening hemorrhage found during the FAST exam is a decision-making tool to help determine the transfer to the operating room, CT scanner, or angiography suite.
Perihepatic and hepatorenal space (right upper quadrant)
Perisplenic (left upper quadrant)
Pelvis: cul-de-sac (bladder)
Pericardium (cardiac)
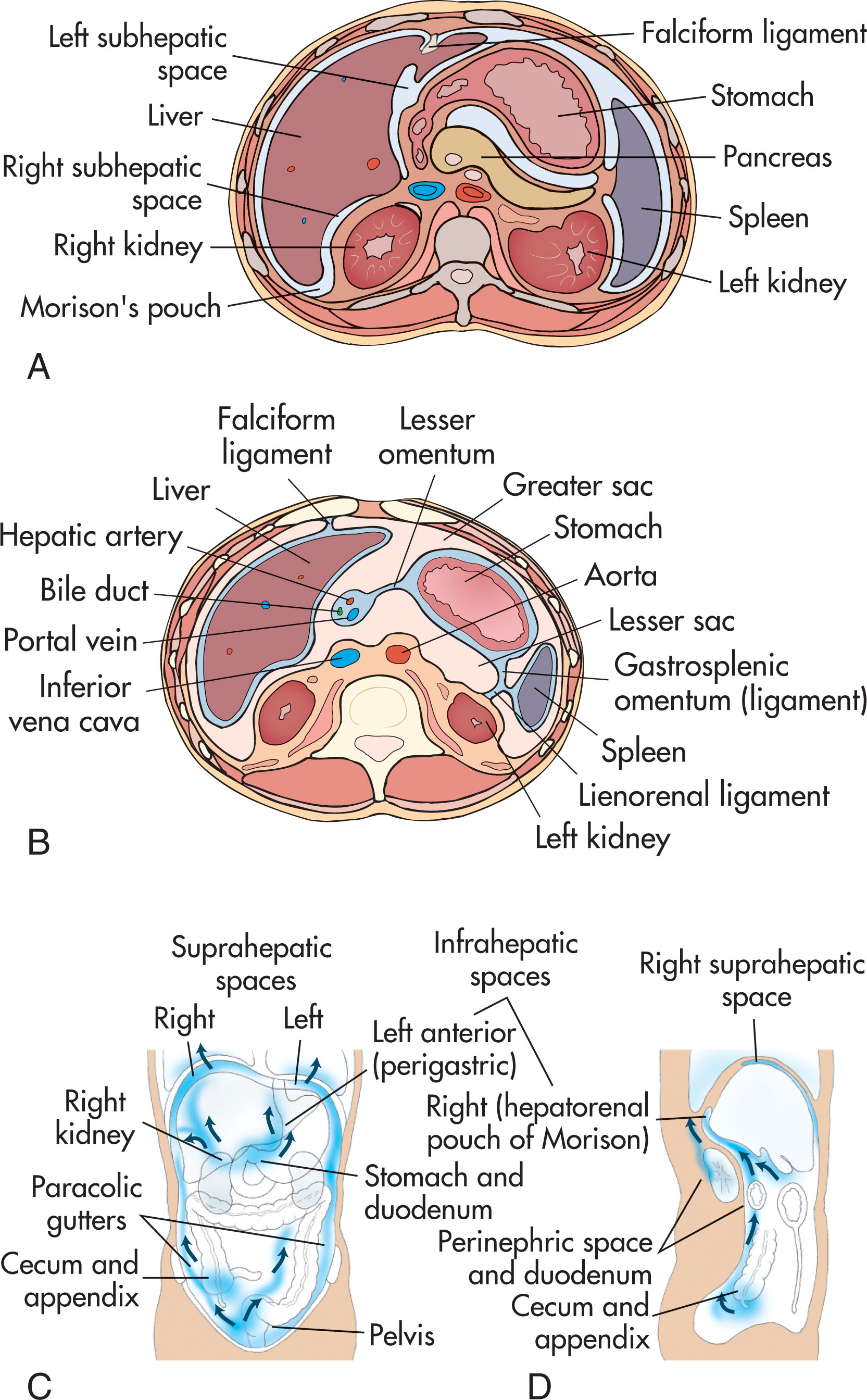
The FAST ultrasound evaluation survey is widespread, extending from the pericardial sac to the urinary bladder and includes the perihepatic area (including Morison’s pouch), perisplenic region (including splenorenal recess), paracolic gutters, and cul-de-sac ( Fig. 19.3 ). The visceral organs are assessed for heterogeneity and evaluated with color Doppler if necessary.
Accessibility and speed of performance are critical in the trauma setting. Onsite personnel who are educated in performing the ultrasound examination provide the highest success rate. Limitations of ultrasound include its dependence on operator skill and patient body habitus, which becomes particularly important if surgeons or emergency physicians with limited training perform the studies. Although CT remains the standard of reference for intraperitoneal and retroperitoneal assessment, this application is not available at the bedside.
Ultrasound of the abdomen and pelvis is performed simultaneously with the physical assessment, resuscitation, and stabilization of the trauma patient. The examination usually takes less than 4 minutes. The goal is to scan the four quadrants, pericardial sac, and cul-de-sac for the presence of free fluid or hemoperitoneum . Ultrasound has been found to be highly sensitive for the detection of free intraperitoneal fluid, but it is not sensitive for the identification of organ injuries. If the patient is hemodynamically stable, the value of ultrasound is limited by the large percentage of organ injuries that are not associated with free fluid.
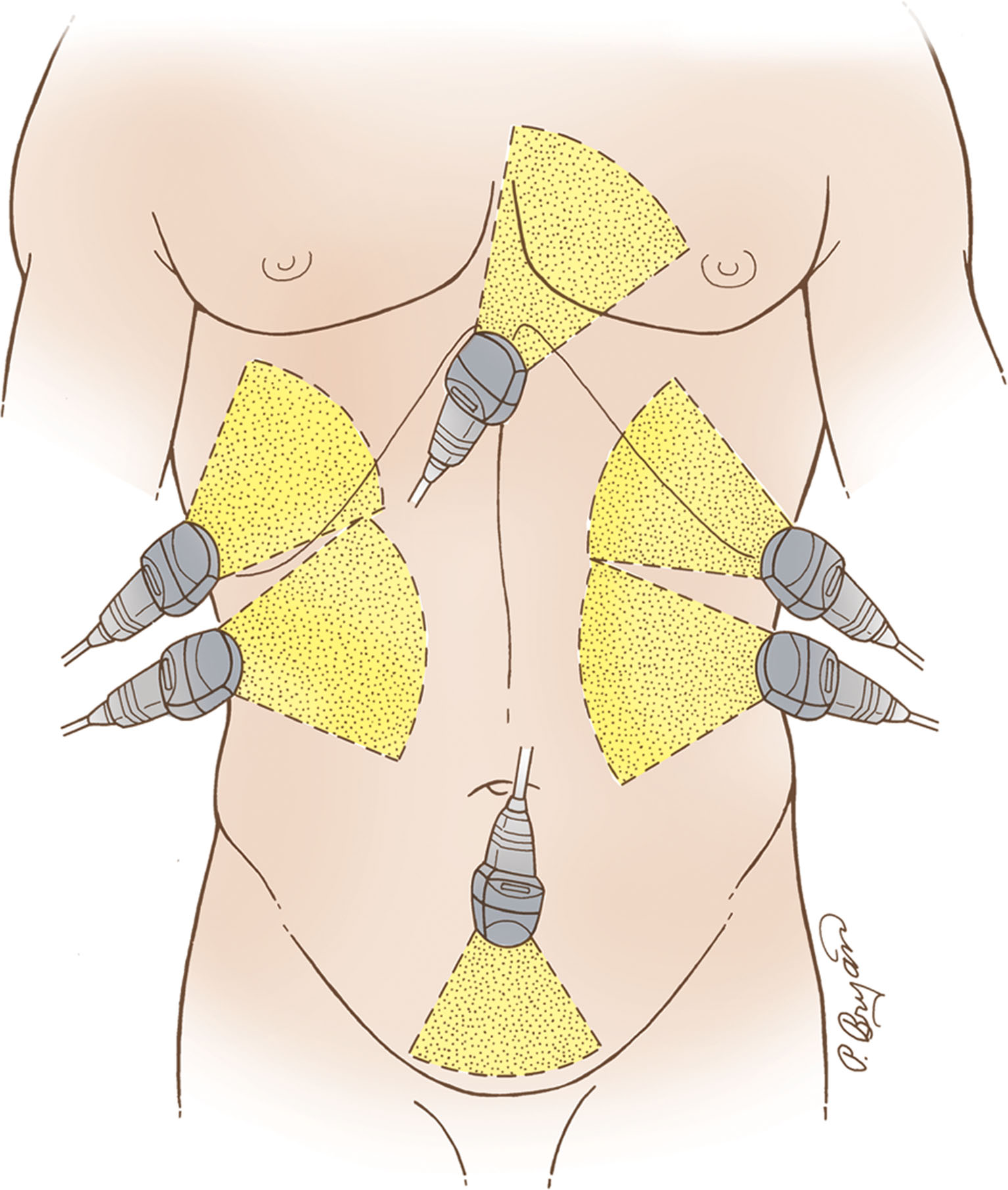
The ultrasound examination is performed with the proper transducer selection according to the patient size. The patient is usually in the supine position. The right and left upper quadrants of the abdomen, epigastrium, paracolic gutters, retroperitoneal space, and pelvis are evaluated with ultrasound ( Box 19.2 ). If there is no contraindication to catheterization, the empty bladder is filled with 200 to 300 mL of sterile saline through a Foley catheter to ensure bladder distention to allow adequate visualization of the pelvic cavity. The examination is focused to look for the presence of free fluid, the texture of the visceral organs, and the pericardial sac around the heart.
Fill urinary bladder
Scan subxiphoid to look for pericardial effusion
Evaluate RUQ: diaphragm, subhepatic space/Morison’s pouch, right kidney, right flank
Evaluate liver for texture abnormalities
Evaluate epigastrium
Evaluate LUQ: diaphragm, spleen, left kidney, left flank
Evaluate RLQ
Evaluate LLQ
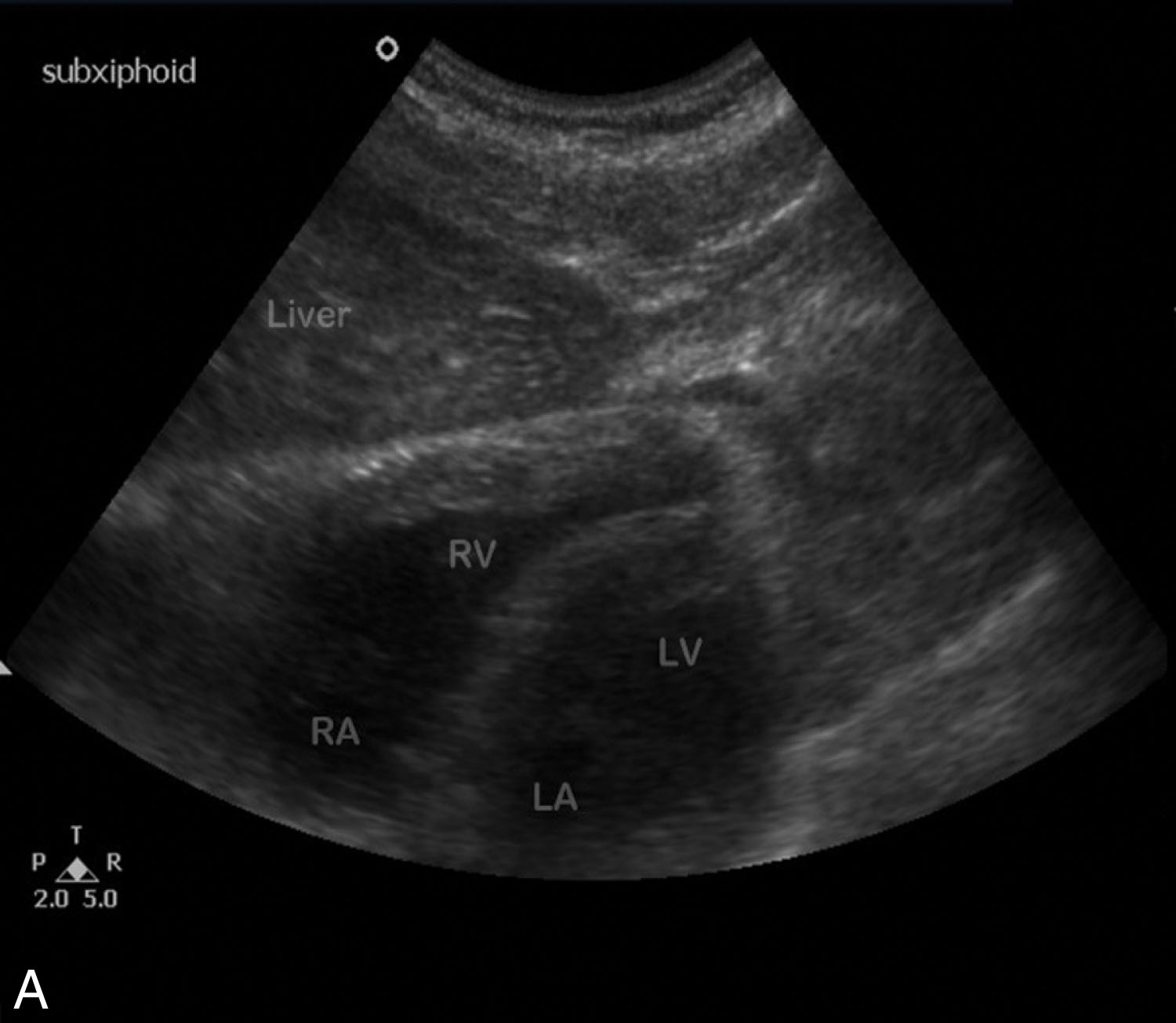
The initial survey is directed in the subcostal plane with the transducer angled in a cephalic direction toward the four-chamber view of the heart to image the pericardial sac ( Fig. 19.4 ). The right upper quadrant is then evaluated, including the diaphragm, dome of the liver, subhepatic space (Morison’s pouch), right kidney, and right flank ( Fig. 19.5 ). The liver is quickly scanned to look for free fluid or hematoma. The epigastrium is briefly examined. The transducer is then moved to the left upper quadrant to observe the diaphragm, spleen, left kidney, and left flank and to search for the presence of fluid ( Fig. 19.6 ). The pelvic cavity (with the bladder distended) is evaluated for the presence of free fluid in the cul-de-sac ( Fig. 19.7 ).

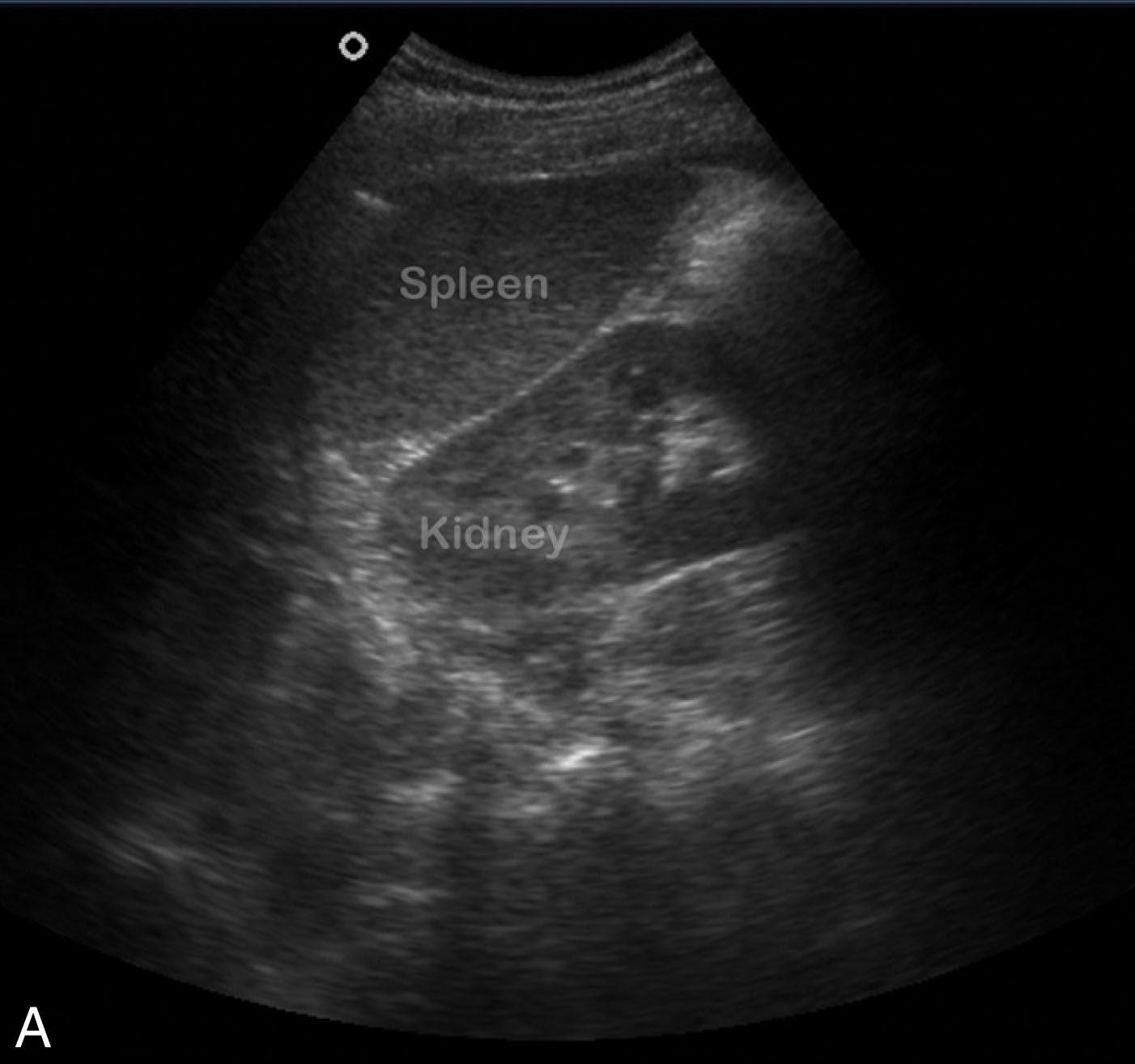
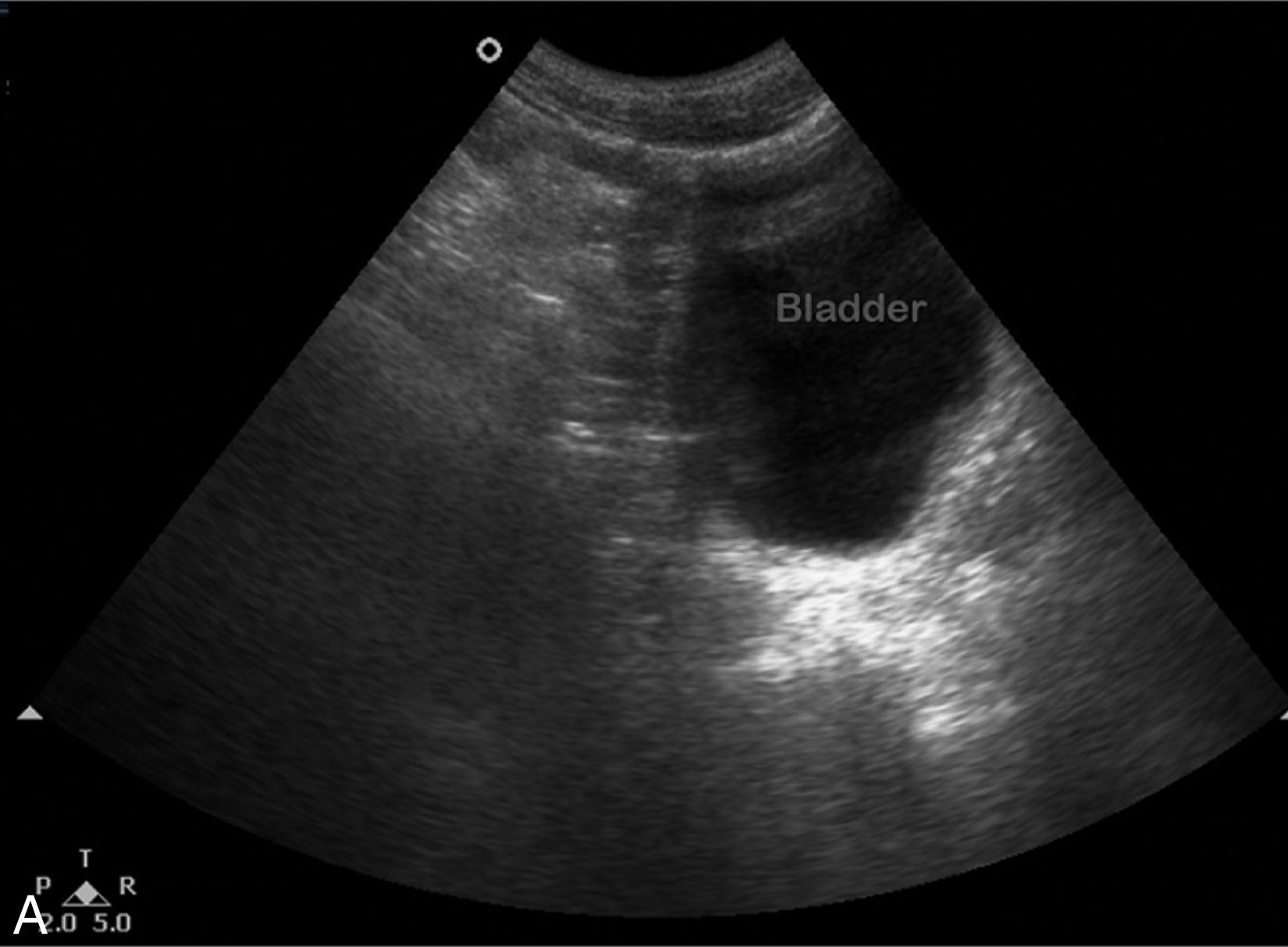
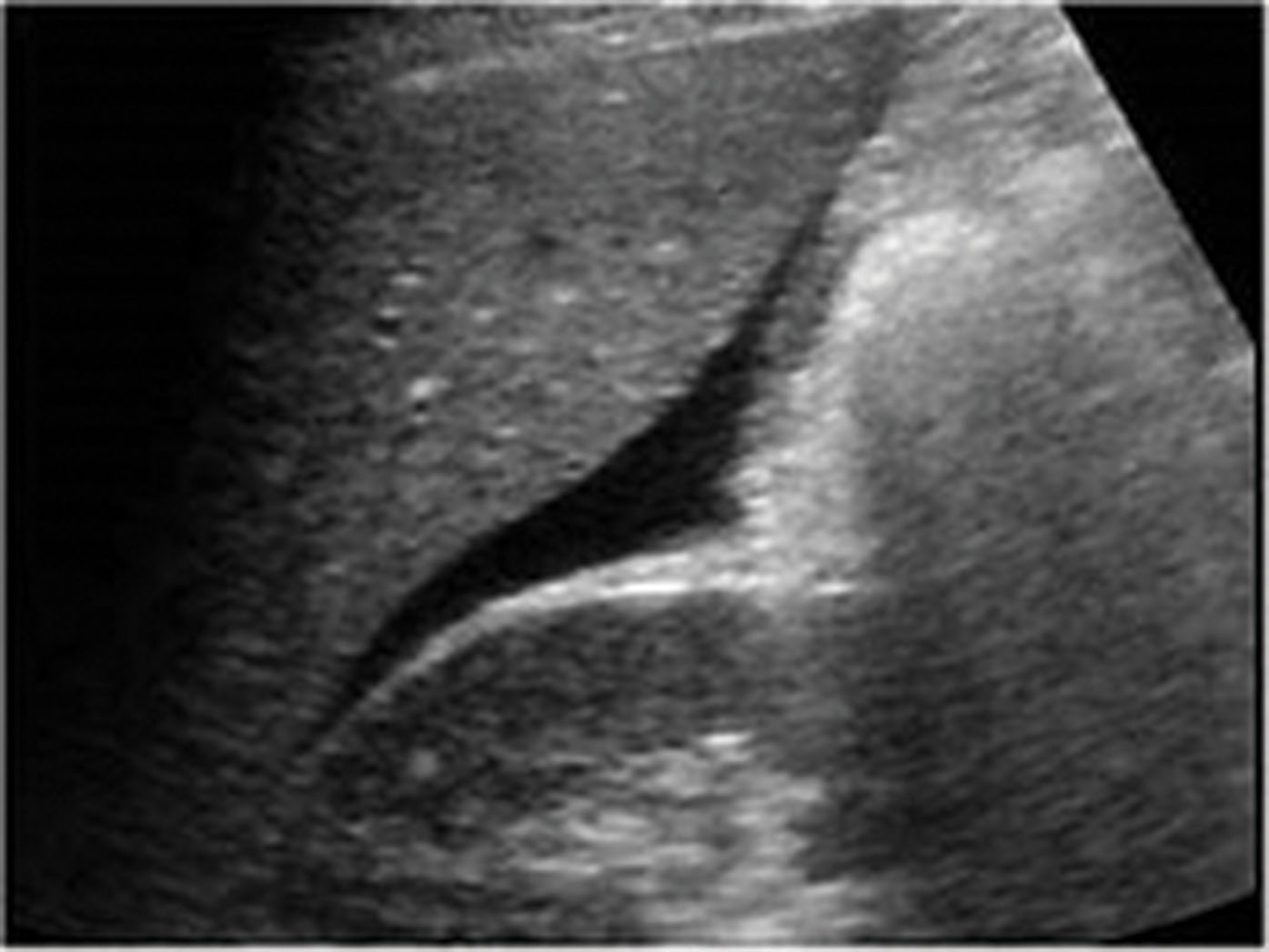
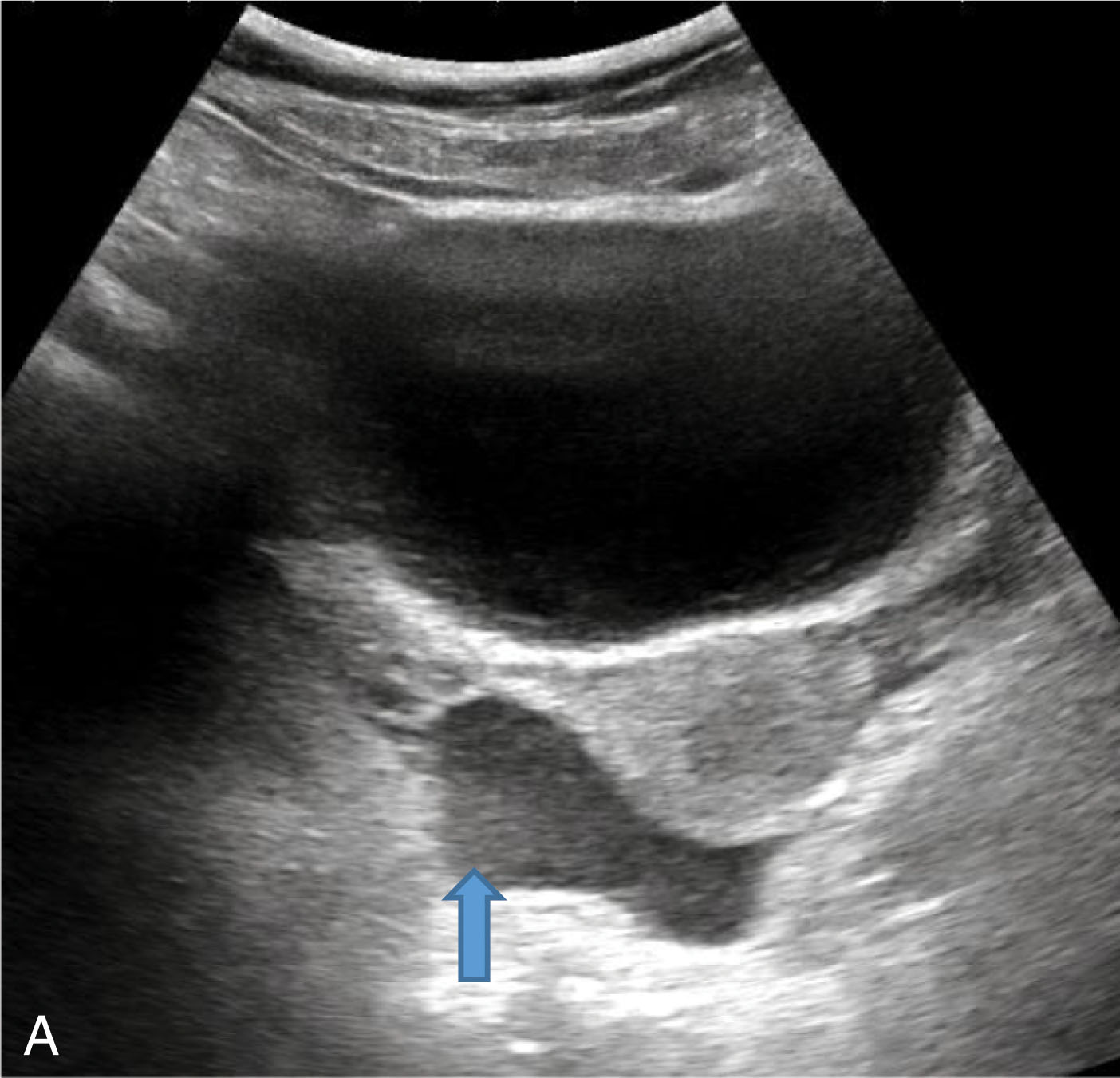
In the trauma setting, free fluid usually represents hemoperitoneum, although it may also represent bowel, urine, bile, or ascitic fluid. Hemorrhage in the peritoneal cavity collects in the most dependent area of the abdomen. The fluid is usually hypoechoic or hyperechoic, with scattered internal echoes representing the blood, and conforms to the anatomic site it occupies ( Fig. 19.8 ). The most common site of fluid accumulation is the subhepatic space (Morison’s pouch), regardless of the site of the injury ( Fig. 19.9 ). The next most common space is the pelvis. The blood in the pelvis may collect centrally in the pouch of Douglas or laterally in the paravesical space ( Fig. 19.10 ). When fluid is present, the poorly visualized loops of bowel are separated by triangular collections of fluid. If there is a massive hemoperitoneum, the intraperitoneal organs will float in the surrounding fluid.
If the collection of fluid is small, the surgeon may not want to do an immediate laparotomy. Close monitoring of the patient with either ultrasound or CT imaging may help to define the further extent of the injury after the patient stabilizes.
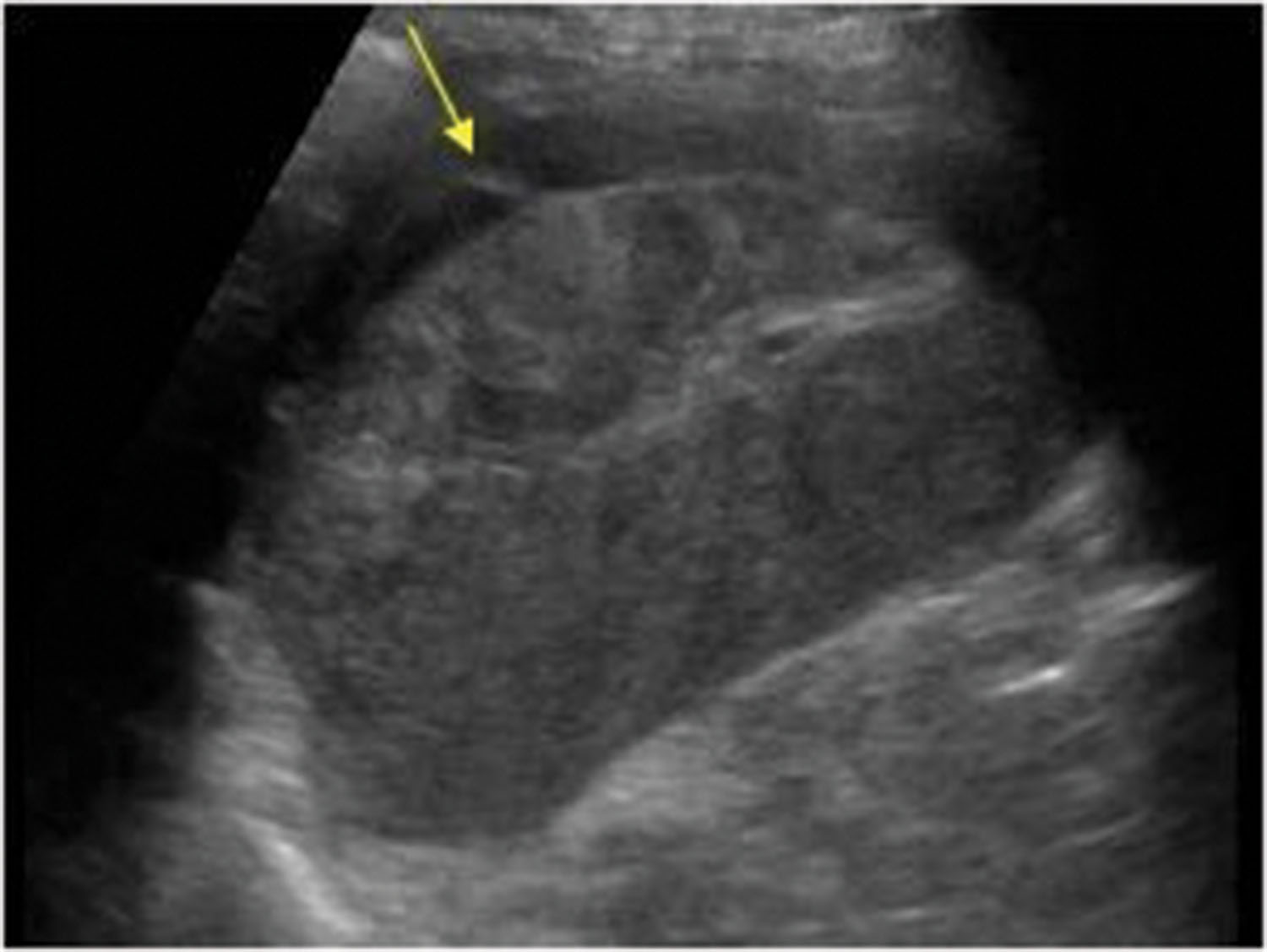
The ultrasound appearance of hepatic and splenic injury will vary with both the type and time of injury. Liver lacerations or contusions are more easily detected with ultrasound than any other visceral abdominal injury ( Fig. 19.11 ). Such injuries appear as heterogeneous or hyperechoic. Hematomas and localized lacerations will appear initially hypoechoic with low-level echoes generated from the red blood cells, or echogenic, as the blood begins to coagulate, which over time will become more anechoic with the onset of hemolysis. Pitfalls of abdominal ultrasound include failure to show contained solid-organ injuries; injuries to the diaphragm, pancreas, and adrenal gland; and some bowel injuries. Therefore a negative ultrasound does not exclude an intraperitoneal injury, and close clinical observation or CT is warranted.
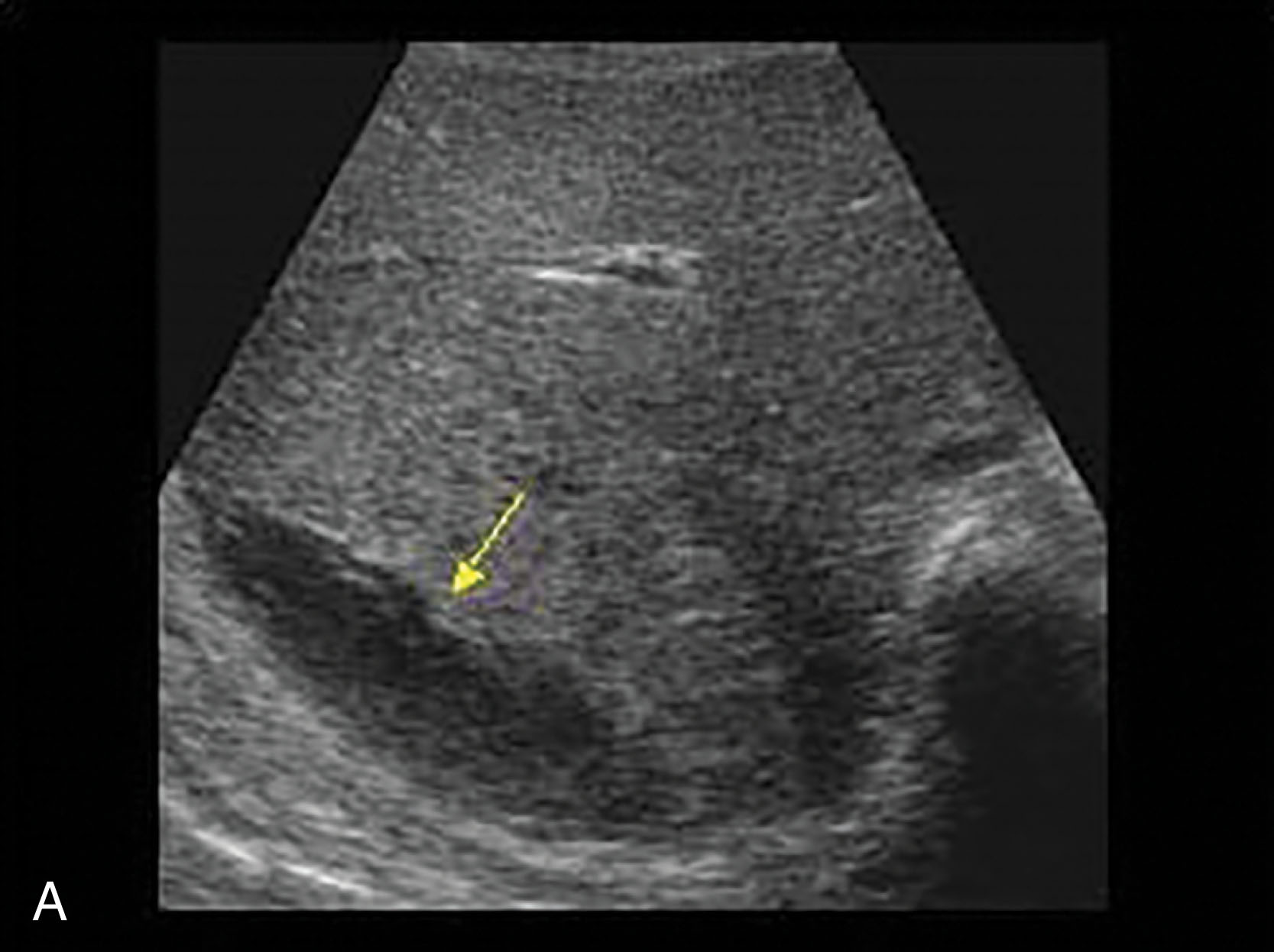
A brisk intraparenchymal hemorrhage may be identified as an anechoic region within the abnormal parenchyma, whereas a global parenchymal injury may project in the liver as a widespread architectural disruption with absence of the normal vascular pattern. An extensive splenic injury presents as a diffusely heterogeneous parenchymal pattern with both hyperechoic and hypoechoic regions.
The early diagnosis of parenchymal injury can affect patient treatment. The clinically stable patient with a hemoperitoneum and an obvious splenic injury seen on ultrasound can be taken directly to surgery. However, if extensive hepatic disruption is demonstrated, the surgeon may want further investigation with CT or even angiography before the surgery is performed.
In female patients of reproductive age with trauma, free fluid isolated to the cul-de-sac is likely physiologic and clinical follow-up should suffice. Female patients with fluid elsewhere usually have a clinically important injury and require further evaluation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here