Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Spine injuries in athletic events are uncommon, representing only 9% of the total spine injuries presenting to trauma centers. Spine injuries are potentially catastrophic events for the participants; these injuries can lead to significant morbidity and can alter a life permanently. Although thoracolumbar injuries do occur in athletics, the vast majority are less serious and usually involve repetitive and overuse mechanisms. This chapter will focus on the acute management of cervical spine injuries that present more acutely, requiring immediate skilled intervention and appropriate care at every step to prevent any increase in morbidity.
Athletic spine injuries represent only a small proportion of all spine injuries presenting to trauma centers, and cervical spine injuries make up only a small fraction of all athletic event–related injuries. Despite the relatively low incidence, the potential for permanent disability or complete loss of function from these injuries requires a heightened sense of awareness. A number of databases and scoring systems have been developed over the past several years in an attempt to better quantify and classify the number and types of injuries that occur and the outcomes that result.
In the United States, American football players are at the highest risk for severe cervical spine injuries, averaging approximately eight catastrophic cervical spine injuries each year. These cervical spine injuries can result in incomplete recovery, and approximately six of these eight injuries result in quadriplegia. Other high-risk sports include ice hockey, gymnastics, rugby, diving, and cheerleading. So-called extreme sports and motor sports convey a risk of spine injuries similar to those commonly associated with vehicular trauma and less like those associated with other sports; this includes an increased risk of acute thoracic and lumbar spine injuries. Skiing and snowboarding are also high-risk sports with the potential increased risk for fractures of the thoracic or lumbar spine.
The management of any athlete with a suspected spine injury begins before the event, with pre-event meetings and the development a site-specific emergency action plan (EAP). Team physicians or event physicians for large tournaments should be involved in all stages of planning. These plans must include athletic training staff, emergency medical services (EMS), athletic directors, and event coordinators, as well as any other key participants. The plan should include specific role delineation for equipment management and spinal motion control (see later), with a clear decision pathway and chain of command for transport decisions. Local officials should designate hospitals in the area that have capabilities to manage acute spinal cord injuries. The capabilities include, but are not limited to, advanced radiology imaging, orthopaedic and/or neurosurgical care, and trauma care capability for participants of all ages. Any athletes with potentially serious injuries should be preferentially transported to these predetermined emergency departments (EDs), if needed, with a prearrival call by the event physician.
Pre-event planning also includes the outfitting of athletes in proper protective equipment. Protective equipment varies sport to sport but may include helmets, shoulder pads, protective eyewear, and mouth guards. All members of the medical team should be familiar with the protective equipment that they may encounter and should be familiar with the removal of the equipment in an emergency situation.
Furthermore, pre-event planning can include injury prevention strategies. Examples of such strategies include the following: teaching athletes how to tackle properly in American football, proper checking techniques in ice hockey and lacrosse, proper heading techniques in soccer, and teaching athletes how to minimize the risk of serious injury from falls in gymnastics and cheerleading. The elimination of spear tackling in football—a maneuver that places the cervical spine of the tackler at risk due to a slightly flexed position (a significant axial load)—in 1976 by a National Collegiate Athletic Association (NCAA) rule represented a significant change directed at player safety. So-called heads-up football tackling has led to a significant reduction in the number of cervical spine injuries in the years since the spear-tackling technique was banned. Finally, athletes and coaches should be instructed on what to do if an injury does occur, including not moving a potentially spinal-injured athlete and how to summon assistance from the medical teams in an emergency.
As noted previously, injuries in extreme sports and motor sports tend to mimic vehicular trauma rather than other athletic injuries. For this reason, physicians and other health care professionals providing care at motor sport events should be prepared for this type of traumatic injury. These injuries are best managed according to the basic and advanced trauma life support (BTLS/ATLS) guidelines, with consideration of local trauma center protocols.
When considering the pre-event planning for potential spine injury, roles should be assigned in advance; a chain of command and decision pathways should be established allowing for efficient and effective management when an injury occurs. The specific roles will be outlined later but may need to be adapted for different settings and different numbers of providers. Collegiate and professional teams may have a fully staffed ambulance, several athletic trainers, and several team physicians available, whereas a rural high school team may have none of these resources on site when an injury occurs. An EAP needs to be specific to the team, site, and availability of resources.
In addition to an EAP, an “emergency toolkit” can be prepared and available at all times during practice and competition. The toolkit will vary depending on the sport and site but should include the necessary equipment to remove protective athletic equipment (i.e., facemask) quickly without disruption to spine immobilization and allow for emergent airway intervention or the performance of cardiopulmonary resuscitation (CPR). These tools will be described in further detail later, but it is critical that medical professionals have more than one device available and are familiar with the safety equipment used by their team/league so the providers have the appropriate removal devices immediately available. In addition, splints and equipment for spinal motion control, including a cervical collar, vacuum splint, and/or long spine board, should also be available. If the listed equipment is not present on the sidelines for all practices and competitions, the medical staff, coaches, etc. need to know where to access a first aid kit, automatic external defibrillator, and additional emergency equipment. Most importantly, all staff should be aware of the procedure for activating EMS and must be able to properly provide a dispatcher with information including the practice or competition location; this requires immediate access to a phone to call 911 or other appropriate local EMS resources.
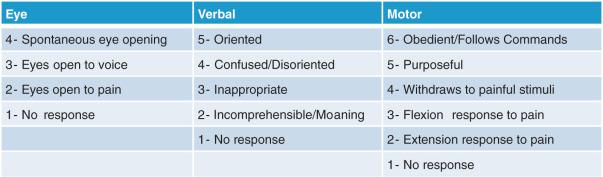
On-field emergencies fall into several categories, and often it is best to think in terms of a flowchart ( Fig. 125.1 ). Consider first the immediate threats to life and assess the athlete's vital functions, using the airway, breathing, circulation, and disabilities (ABCDs) approach to evaluation. This evaluation can be accomplished with a quick assessment of level of consciousness—the awake, alert athlete who is answering questions appropriately meets all criteria and the sideline physician can move on to the next phase of the exam. The Glasgow Coma Scale (GCS; Fig. 125.2 ) is often used in trauma assessment, with lower scores suggesting a higher risk of serious injury. A simpler system, such as the AVPU scale, may be more useful in emergency situations. In this system, the patient's mental status is divided into one of four categories based on their response to stimulation: A—alert; V—verbal, responds to verbal stimuli; P—pain, responds to painful stimuli; and U—unresponsive or unconscious. The AVPU scale is easier to apply in emergency settings while still providing important information about a patient's mental status and medical condition.
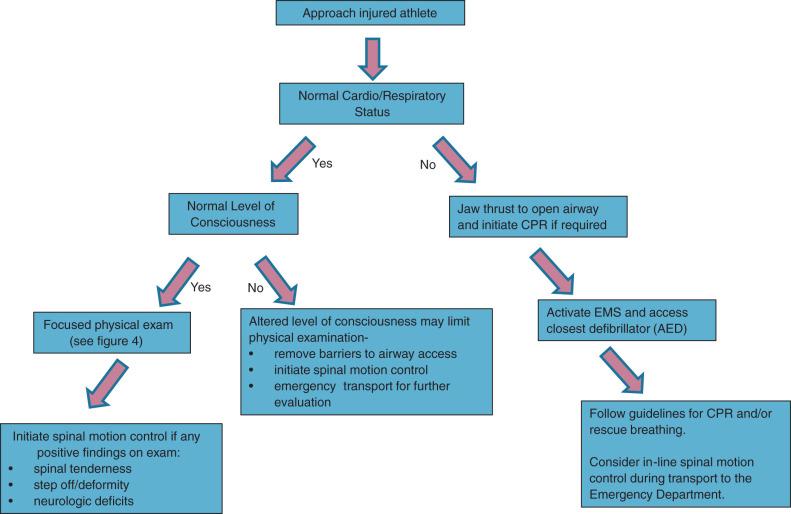
For the unconscious athlete, a pulse check should be performed and adequacy of respirations should be assessed. If either is found to be inadequate, immediately remove any accessory intraoral devices (i.e., mouthguard). However, the clinician should be cautious with the routine removal of other protective equipment without further clinical examination. A jaw thrust should be used to open the airway; the jaw thrust maneuver and placement of an oropharyngeal airway have less effect on cervical spine alignment than does the performance of a “head tilt” maneuver that places the cervical spine in extension. Appropriate ventilation may be maintained with the use of a bag-valve mask ventilation as needed. Additional airway maneuvers and/or CPR should also be initiated immediately if indicated. Protective chest equipment may be removed by cutting through the laces or elastic straps either in the axilla or over the sternum to expose the chest. With these cut, the pads can be opened, allowing access to the chest for compressions and/or the application of cardiac defibrillator pads.
Choosing the optimal technique for definitive emergency airway management is often perceived as a clinical dilemma, and many clinicians believe that orotracheal intubation is hazardous in the presence of a known or potential cervical spine injury. However, several studies have shown that operator skill and comfort in performing a specific airway technique should guide the selection of a particular method. Several authors have concluded that orotracheal intubation is safe and effective when performed with in-line cervical stabilization. Using a cadaver model, Gerling et al. showed no significant vertebral body movement during orotracheal intubation with manual in-line stabilization. With the relatively recent advent of video-assisted laryngoscopy (VAL), many have questioned whether this technique improves patient safety versus direct laryngoscopy. There appears to be general consensus that VAL does provide significantly better glottic visualization. Turkstra et al. also found that cervical spine motion was reduced by 50% at the C2–C5 levels when VAL was used. These findings were opposed by Robitaille et al., who concluded that there was no significant difference found between direct laryngoscopy and VAL at any cervical level in regard to motion. The use of a supraglottic airway device may also be considered, because these may be placed with minimal movement of the cervical spine and provide an airway for less-advanced providers. Supraglottic devices are not considered definitive airway protection. The current ATLS guidelines state orotracheal intubation with in-line manual cervical spine stabilization is the definitive airway procedure in the apneic patient. Finally, physicians must be prepared to perform a surgical airway in trauma patients with potential cervical spine injuries who cannot be intubated orally or nasally.
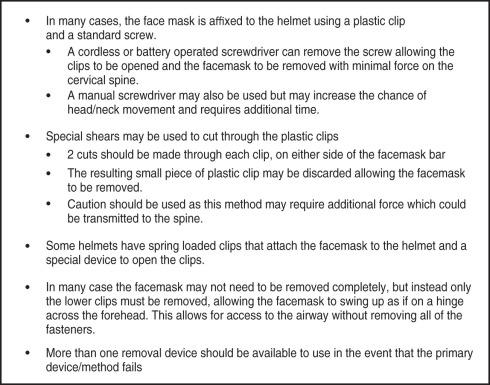
In athletes wearing protective equipment with facemasks, the facemask will need to be removed prior to invasive airway maneuvers. In fact, the facemask should be removed regardless of whether airway maneuvers are required at the time of initial evaluation on the field. This is performed for the purposes of ongoing monitoring of the airway and allows for immediate interventions if deterioration occurs. Athletic trainers and physicians who work with athletes in sports that use protective equipment (hockey, lacrosse, football, motorsports, etc.) should be familiar with the brand/type of equipment worn by their athletes and should possess the necessary tools to assist in the removal of equipment in an emergent case. The facemask is generally attached by several retention clips. These clips are typically made of soft plastic material and fastened to the helmet by screws or spring-loaded fasteners. In the latter case, special devices are provided by the manufacturer that depress the center of the clip, activating the spring and causing the clip to fall apart, releasing the bar of the facemask. In facemask equipment where the clips are connected with screws, a manual or electric-powered screwdriver may be used to remove the screw. In studies, a power screwdriver has proven to be faster and easier to use than devices designed to cut through the plastic clips. The electric drivers deliver the least force and movement to the head during helmet removal. Manual screw drivers may be used as a “back-up” method. Tools that cut through the plastic clips themselves, while producing somewhat more force and movement, are also an alternate method of accessing the airway if electronic and manual methods fail ( Fig. 125.3 ).
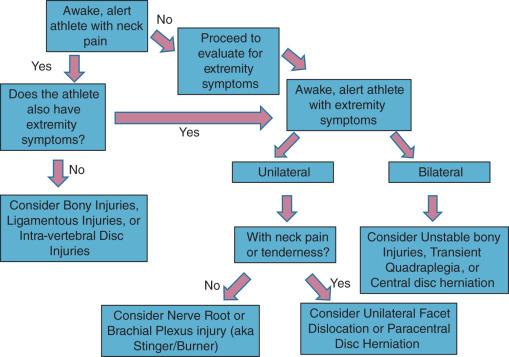
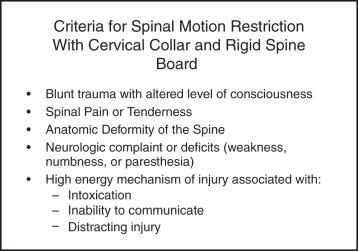
If the ABCs are intact and the patient is awake and answering questions appropriately, then the clinician may move on to a focused physical examination ( Fig. 125.4 ). The examination should include an assessment for pain and/or tenderness, as well as strength, sensation, and reflexes. Examination findings that suggest spine injury may include: midline neck pain, step-offs, palpable deformities, tenderness on palpation, weakness in the extremities, or persistent and/or bilateral numbness and tingling. When these signs/symptoms are present, care should be taken to minimize the movement of the spine while preparing the athlete for transport for definitive care ( Fig. 125.5 ). In the absence of neck pain, evaluation of active and passive range of motion (ROM) should be performed. Serial examinations are important to assess for progression or resolution of symptoms.
When preparing the athlete for transport, the clinician must start the assessment with a high regard to the initial positioning in which the athlete is found at the end of the play. Athletes generally either land prone, supine, or side-laying. Fig. 125.6 depicts the key steps for management of athletes in each position. Depending on the sport, conditions such as weather, surface (ice hockey or ski slopes), barricades or walls (ice hockey, arena football), and other hazards (motocross motorcycle racing) must also be considered when attempting extrication of the athlete.
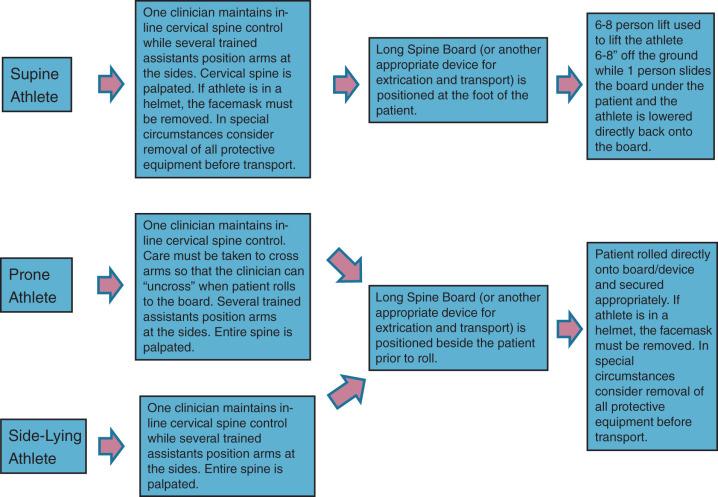
After manual in-line stabilization of the cervical spine has been achieved by a single clinician (usually the first clinician to reach the injured athlete) and the airway secured, as previously described if needed, attention should be turned toward managing equipment. In a 2001 position statement, the Inter-Association Task Force for the Care of the Spine Injured Athlete published recommendations stating that football helmets and shoulder pads should remain in place (with the facemasks removed) during transport to the hospital. These guidelines recommend limiting spinal motion with a rigid immobilization device and suggest that protective equipment may be removed in the hospital. However, it should be noted that equipment in other sports such as hockey, lacrosse, and motor sports may not keep the spine in a neutral position and may need to be removed or padded in a way to maintain neutral spinal alignment during transport. Furthermore, the guidelines from the Inter-Association Task Force are under revision at the time of the writing of this text, and there may be a move to offer clinicians in the field the discretion to consider the removal of equipment prior to transport. Athletic trainers and team physicians have more familiarity with athletic equipment and with the proper equipment removal procedures that require a number of trained providers and several specific deliberate steps ( Fig. 125.7 ).
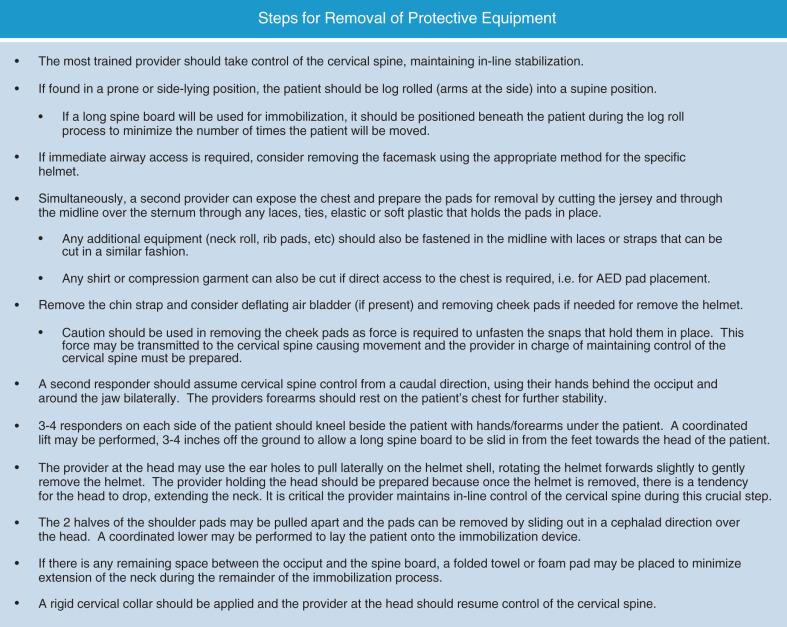
Once the decision has been made to transport, with or without equipment in place, a coordinated response between team medical staff and EMS is required. The term “spinal immobilization” is somewhat of a misnomer because it is impossible to completely immobilize all the spinal levels during transport. It is still reasonable and appropriate to attempt to minimize any and all spinal motion during evaluation and transport. The awake, alert athlete with pain and without significant motor deficits may be able to “self-splint,” allowing for transport on a stretcher in a semirecumbent position. For athletes with neurologic deficits, a greater level of protection is obviously required. Although their value in minimizing movement and further injury has not been proven, the application of a rigid cervical collar may help to minimize movement of the cervical spine during transport, especially in the athlete with altered mental status. However, a cervical collar may not fit on an athlete wearing certain protective equipment. In these cases, foam head blocks and tape or similar devices may be used to minimize head movement during transport. A scoop stretcher, full-body vacuum splint, or rigid spine board all may be appropriate devices for spinal motion control. These devices should be used for extrication from the field of play and, depending on local protocols and transport times, may be continued during transport to the ED.
In the hemodynamically unstable patient, ED evaluation should proceed according to appropriate trauma guidelines. The ED specialist must first prioritize acute life threats while protecting the spine. Some studies have shown that protective athletic equipment interferes with adequate imaging and should be removed before any imaging is obtained. In the hemodynamically stable patient, protective equipment may be removed using the systematic process outlined previously. In addition to the method described in the figure, Horodyski et al. reported decreased cervical spinal motion while removing equipment in a cadaver model by elevating the torso approximately 30 degrees prior to the removal of shoulder pads. However, this method requires an additional provider and may exacerbate thoracic and lumbar injuries if present.
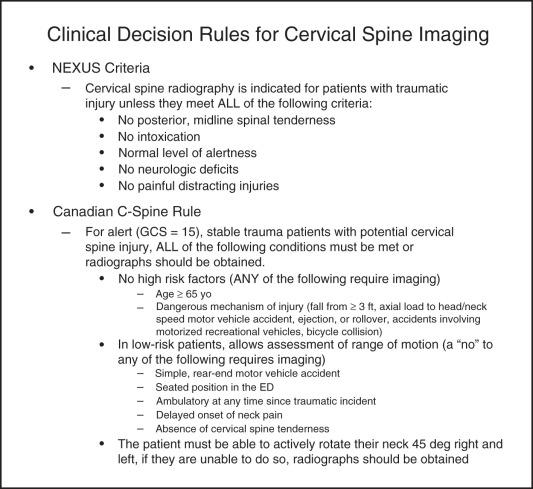
The National Emergency X-Radiography Utilization Group criteria and the Canadian C-spine rules ( Fig. 125.8 ) provide a clinical decision support tool for the evidence-based requisite for imaging. Athletes who have already met criteria for EMS activation and transport to the ED will often meet these criteria. Standard diagnostic imaging has historically included plain radiographs including anteroposterior, lateral, and odontoid views. Particular attention should be directed to the odontoid-C1 and the C7-T1 junctions. However, many centers are moving towards computed tomography (CT) as the primary mode for imaging of the spine in trauma because it is more efficient and has a higher sensitivity and specificity compared with plain radiographs. Providers are cautioned to exercise conservative clinical judgment when considering the possibility of a spine (or other significant) injury; the clinical decision tools assist with decision-making but do not make decisions for the clinician.
CT and plain-film radiographs are the best imaging modalities for evaluating bony injuries. Magnetic resonance imaging (MRI) is a superior modality when evaluating soft tissue injuries and is the only imaging modality that evaluates the spinal cord directly. MRI can be used to evaluate ligamentous and disk pathology, as well as to provide evaluation of marrow edema within bony structures. Selective use of MRI is appropriate in certain cases, such as persistent neurologic deficit or when vascular or nerve root injuries are suspected. However, MRI is time consuming, not ubiquitously available, resource intensive, and expensive. These considerations make MRI imaging impractical for most athletes and trauma patients.
A condition known as spinal cord injury without radiography abnormality, or SCIWORA, is used in older literature to describe persistent neurologic deficits in cases where bony and ligamentous injuries were not found on plain radiographs or CT scans. Due to the increasing use of MRI, the incidence of SCIWORA has decreased because it is now possible to identify more soft tissue etiologies for symptoms. The term SCIWORA is still used to describe a patient with a neurologic injury pattern that is suspicious for spinal cord injury but in whom plain radiographs and CT scan do not identify an etiology. MRI is the next logical step in the evaluation and treatment of such injuries.
Acute spinal injuries are separated into several broad categories, including bony injuries, disc herniations, stingers/burners, and transient quadriplegia; bony injuries and disc herniations can occur with and without neurologic compromise.
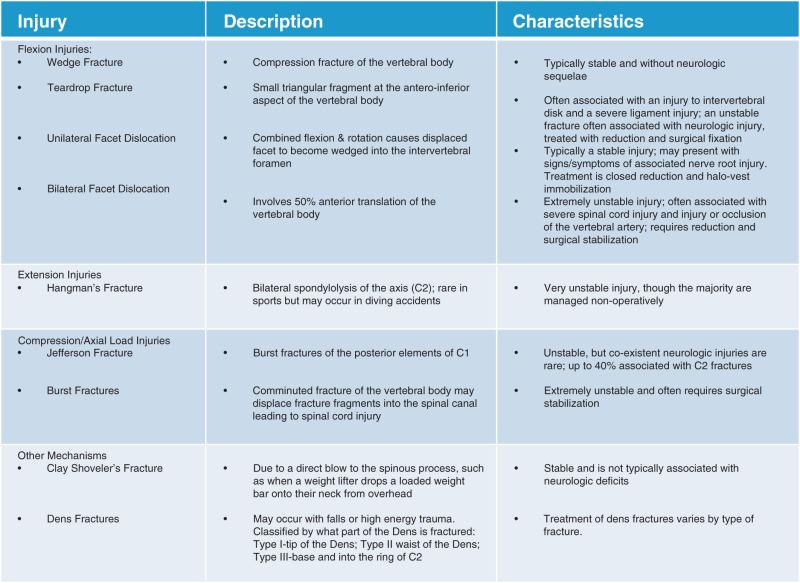
Bony injuries related to acute fractures and dislocations are among the most common and potentially catastrophic of spinal cord injuries in athletes, along with concomitant soft tissue injuries. Injuries to the high cervical spine are rare in sports but may be seen with high-energy mechanisms or diving injuries. In the lower cervical spine, C5 is the most commonly injured vertebrae, with C5 on C6 as the most common site of spinal subluxation. A narrower diameter of the cervical cord in the lower cervical spine may lead to an increased incidence of neurologic injury at these levels. See Fig. 125.9 for a list of common bony injuries of the cervical spine.
Transient tetraplegia, also called spinal cord neurapraxia or cervical cord neurapraxia, is a term describing a spectrum of injuries. The spectrum of transient tetraplegia ranges from simple weakness to brief, self-limited paralysis without abnormalities on routine imaging, including MRI. This injury most often occurs after a mechanism that combines slight neck flexion with axial loading. Athletes with transient neurapraxia often present with motor weakness and sensory changes without neck pain or tenderness. These athletes will maintain full ROM on examination. The neurologic deficits and dangerous mechanism warrant radiographic imaging to rule out more serious injury.
Stingers/burners are common injuries in contact and collision athletic events. Approximately half of NCAA college football players report experiencing this type of injury each year. Stingers/burners are the result of compression of the neural foramen with associated stretch on the contra lateral brachial plexus and/or nerve roots. The mechanism involves forced lateral neck flexion associated with mild extension. These forces result in transient unilateral dysesthesias and numbness in the affected limb that may also be associated with some degree of motor weakness. These athletes usually have full ROM and no neck pain or spinal tenderness. The injury is usually self-limited with symptoms resolving in 24 to 48 hours and do not require imaging. Persistent symptoms beyond 48 hours should necessitate further diagnostic studies.
Acute traumatic disc herniations may also occur in athletics. These injuries may lead to a range of symptoms, including pain, paresthesias, and/or weakness in a dermatomal distribution. The motor/sensory dermatome will guide imaging recommendations for the level of neuroforaminal stenosis. In the acute setting, neurologic deficits indicate a need for urgent imaging, with MRI clearly the modality of choice.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here