Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The period of organogenesis, also called the embryonic period, spans the third to the eighth week of development. At approximately 15 days after fertilization, invagination and lateral migration of mesodermal cells occur between the ectodermal and endodermal layers of the embryo. At about the sixteenth day of development, the posterior wall of the yolk sac forms a small diverticulum, the allantois, which extends into the connecting stalk. The hindgut undergoes slight dilation to form the cloaca; it receives the allantois ventrally and the two mesonephric ducts laterally. By the seventeenth day of development, the endoderm and ectoderm layers are separated entirely by the mesoderm layer, with the exception of the prochordal plate cephalad and the cloacal plate caudal. The cloacal plate consists of tightly adherent endodermal and ectodermal layers. With ventral bending of the embryo, the connecting stalk and contained allantois, as well as the cloacal membrane, are displaced onto the ventral aspect of the embryo.
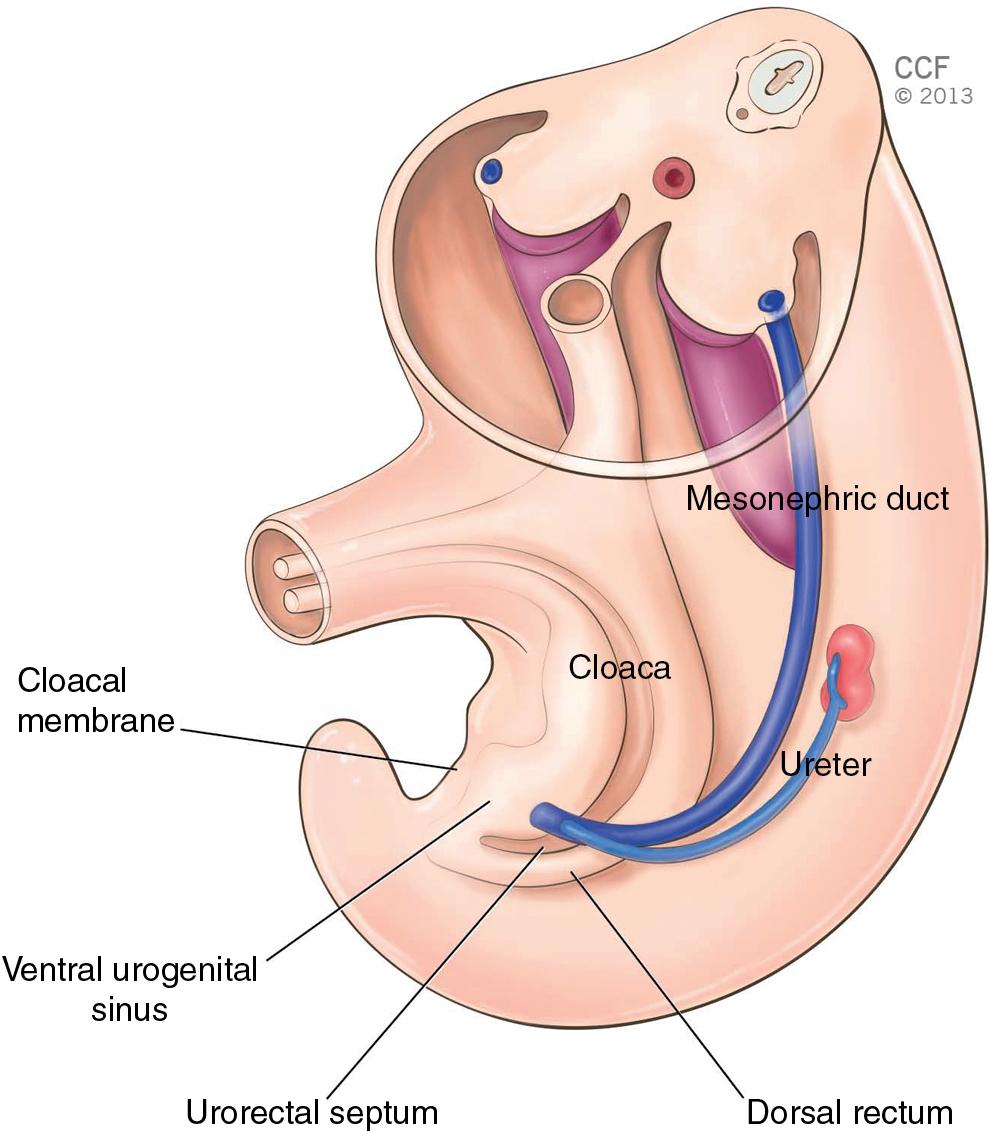
A spur of mesodermal tissue migrates from the base of the allantois toward the cloacal membrane around 28 days after fertilization, forming the urorectal septum ( Fig. 2.1 ). This structure partitions the cloaca into a ventral urogenital sinus and a dorsal rectum. Following this, each of the three germ layers, the endoderm, mesoderm, and ectoderm, give rise to specific tissues and organs. The intermediate mesoderm differentiates into the urogenital structures. Other portions of the mesoderm form multiple structures, including the vascular system, the spleen, the connective tissue, and the wall of the gut tube.
At birth, the urogenital system can be divided functionally into two different systems: the urinary system and the genital system. However, embryologically and anatomically they are intimately connected because both develop from a common mesodermal ridge known as the intermediate mesoderm. Both systems share a common origin, with significant interaction between the components of each system during the later stages of development. Epithelial-mesenchymal interactions are primarily responsible for the maintenance and differentiation of many of the structures of the urogenital system. Furthermore, male and female sexual differentiation is dependent on the presence of specific promoting or inhibiting factors.
This chapter will explore the embryology and basic congenital anomalies of the urinary tract, rectum, and anal sphincters. It will detail the embryology of female genital organs and discuss congenital anomalies and their treatments.
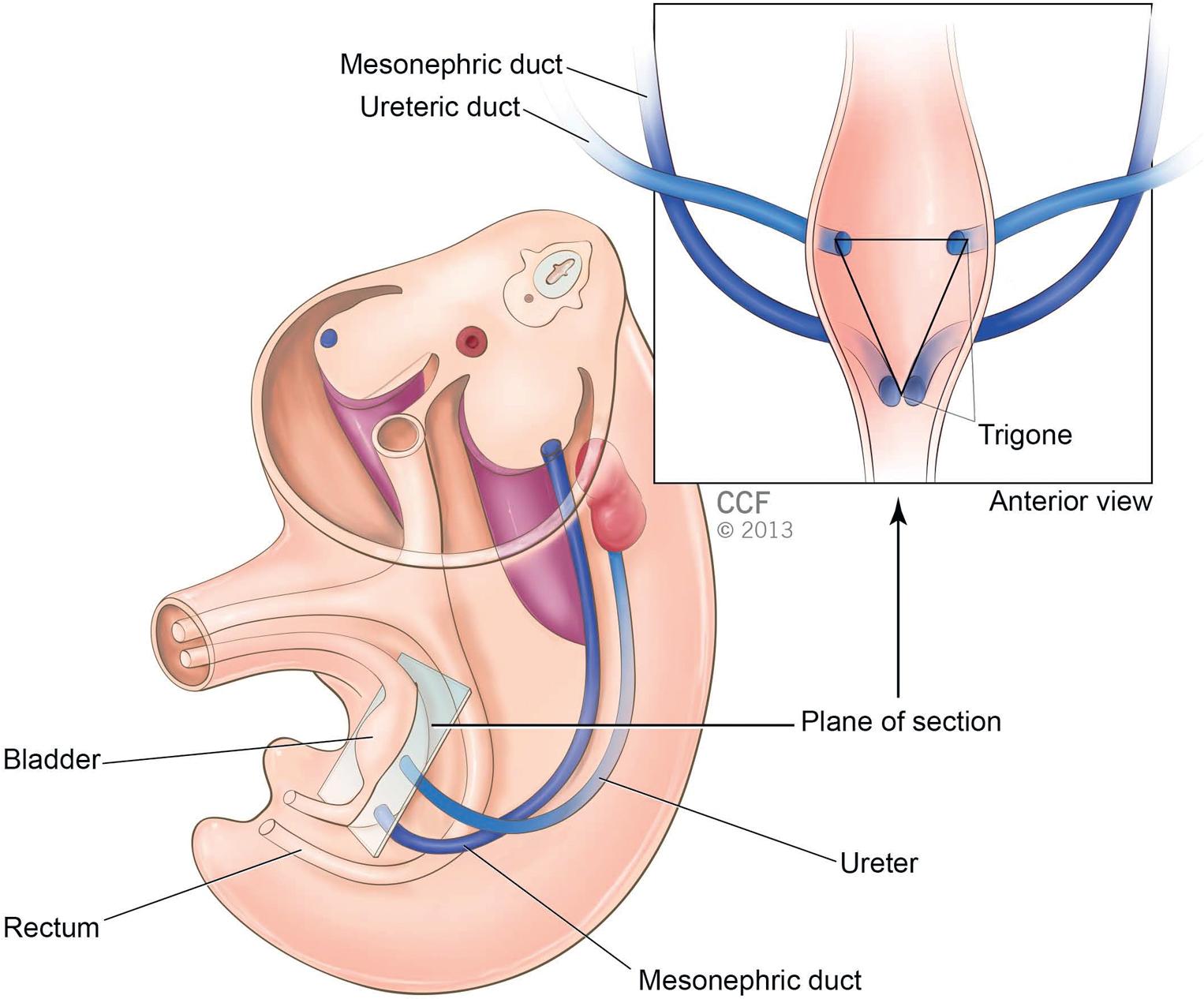
The urinary system begins to take shape before any gonadal development is evident. The kidney exists in three distinct but slightly overlapping forms during development. The first is the pronephros, which is present at approximately 22 days of gestation and is rudimentary and nonfunctioning. The second form, the mesonephros, likely functions for a short time during the early fetal period. The excretory tubules of the mesonephros enter the longitudinal collecting duct (primary nephric duct). These formations go on to form the mesonephric duct, which is crucial in the formation of the male genital system but disappears in the female. By the end of the fourth week, the mesonephric ducts attach to the cloaca, and a continuous lumen is present. The ureteric bud is an epithelial outgrowth of the mesonephric duct near the attachment to the cloaca that penetrates the mesodermal tissue and ultimately forms the renal calyces, ureter, renal pelvis, and collecting tubules. Interactions between the mesoderm and ureteric bud form the third and permanent form of kidney, the metanephros ( Fig. 2.2 ). The excretory units of the kidney develop from the metanephric mesoderm.
The definitive kidney, formed from the metanephros, begins to function around the twelfth week of development. Urine is passed and mixes with amniotic fluid. The fetus swallows this and recycles it through the kidney. During fetal life, the placenta is responsible for waste excretion, not the kidney.
Initially the kidney is positioned in the pelvic region, but it begins a caudal ascent secondary to lumbar and sacral body growth in the late embryonic and early fetal periods. If a kidney fails to ascend, it remains close to the iliac vessels and is known as a pelvic kidney. Occasionally, the kidneys are so close in proximity that the lower poles fuse, leading to development of a horseshoe kidney. This structure often cannot ascend completely, as it cannot pass the inferior mesenteric artery root.
During the fourth to seventh week of development, the cloaca divides into two separate structures: the urogenital sinus (anteriorly) and the anal canal (posteriorly). These structures are separated by a mesodermal structure, the urorectal septum. The tip of this septum eventually forms the perineal body. The upper and largest portion of the urogenital sinus forms the urinary bladder, which is of endodermal origin. Initially, the bladder is continuous with the allantois (rudimentary structure primarily involved in nutrition and waste excretion in the embryo), but the lumen of the allantois becomes obliterated and forms a fibrous cord called the urachus, which runs from the bladder dome to the umbilicus and is called the median umbilical ligament in the adult. The middle portion of the urogenital sinus forms the prostatic and membranous parts of the urethra, and the distal portion forms the phallic portion.
The expanding wall of the bladder grows and incorporates the mesonephric ducts and ureteric buds, forming the bladder trigone. This structure provides a mesodermal contribution to the endodermal wall of the vesicourethral canal. At about 42 days after fertilization, the trigone may be defined as the region of the vesicourethral canal lying between the ureteric orifices and the termination of the mesonephric ducts (see Fig. 2.2 ). The caudal portion of the vesicourethral canal remains narrow and forms the entire urethra. The urethra consists of epithelium that is derived from endoderm, whereas the surrounding connective tissue and smooth muscle are mesodermal in origin. In females, the cranial portion of the urethra gives rise to the urethral and paraurethral glands. A timetable and schematic representation of the embryologic contributions of the various structures of the urogenital system are shown in Table 2.1 and Fig. 2.3 , respectively.
| Time After Fertilization | Event |
|---|---|
| 15 days | Ingrowth of intraembryonic mesoderm |
| 16–17 days | Allantois appears |
| 17 days 22 days 28 days |
Cloacal plate forms Pronephros present Mesonephric duct reaches cloaca; ureteric bud appears |
| 28–49 days | Partitioning of cloaca by urorectal septum |
| 30–37 days | Ureteric bud initiates formation of metanephros (permanent kidney) |
| 41 days | Lumen of urethra is discrete; genital tubercles prominent |
| 42–44 days | Urogenital sinus separates from rectum; mesonephric ducts and ureters drain separately into urogenital sinus, defining boundaries of trigone |
| 51–52 days | Kidneys in lumbar region; glomeruli appear in kidney |
| 12 weeks | Renal function initiates |
| 13 weeks | Bladder becomes muscularized |
| 20–40 weeks | Further growth and development complete the urogenital organs |
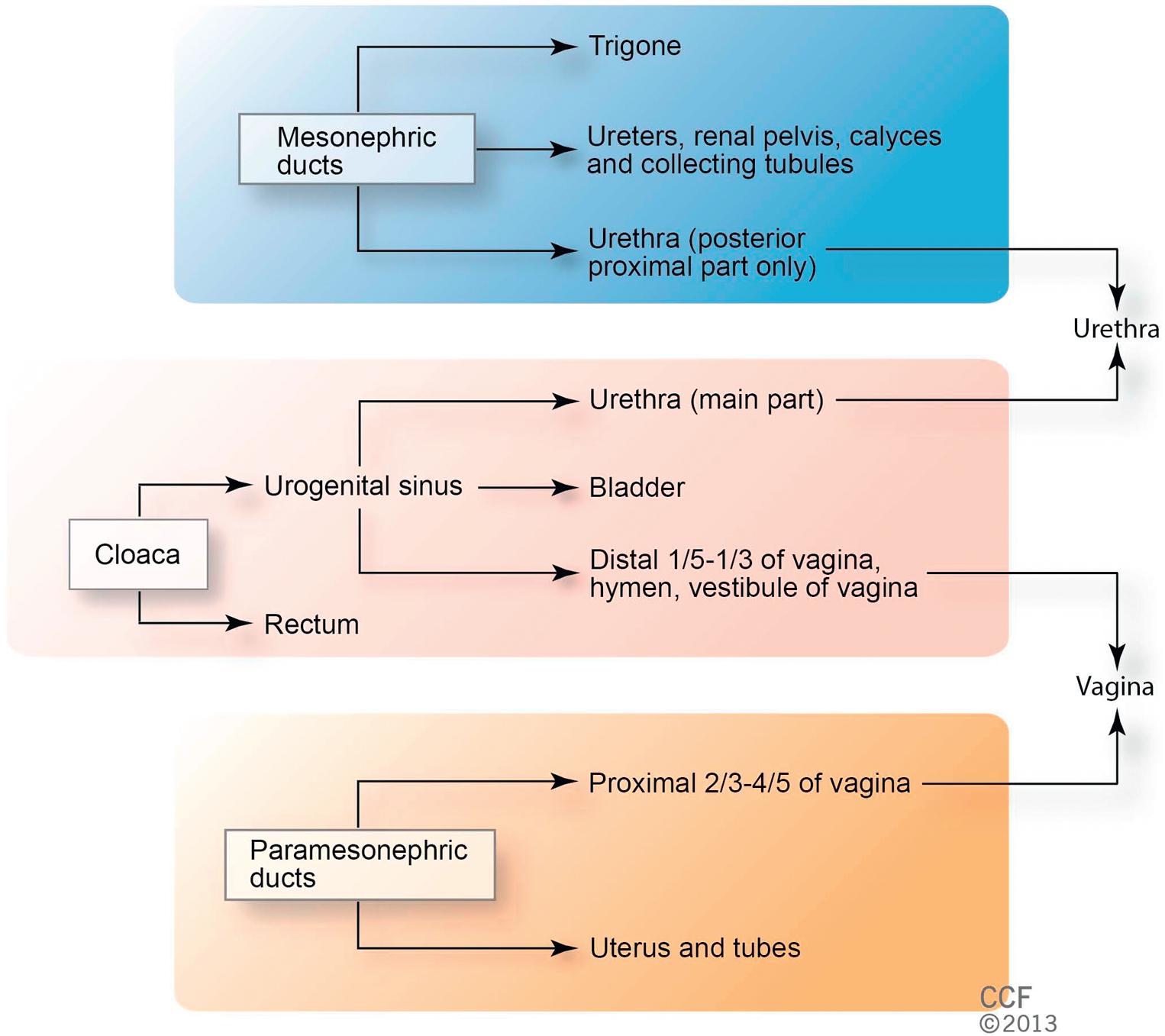
The separate development of the trigone and bladder may explain why the muscle laminae of the trigone are contiguous with the muscle of the ureter, but not with the detrusor muscle of the bladder. This separate development also may account for pharmacologic responses of the musculature of the bladder neck and trigone, which differ partially from those of the detrusor. Because of its embryonic origins (mesonephric ducts and ureters), initially the bladder mucosa is mesodermal, but with time this lining is replaced by endodermal epithelium from the hindgut.
Anomalies of the urinary system are common (3%–4% of live births). Knowledge of the embryology of the genitourinary system is necessary for understanding the causes of the multiple congenital anomalies of the upper and lower urinary tracts. Selected congenital anomalies of the urinary tract and their embryologic causes are shown in Table 2.2 .
| Condition | Embryologic Cause |
|---|---|
| Renal agenesis | Faulty interaction between the ureteric bud and metanephrogenic mesenchyme |
| Pelvic kidney | Failure of kidney to ascend to the lumbar region |
| Horseshoe kidney | Fusion of lower poles of both kidneys; ascent to lumbar region prevented by root of inferior mesenteric artery |
| Urachal fistula, cyst, sinus | Variable persistence of the intraembryonic portion of allantois, from bladder to umbilicus |
| Double ureter | Early splitting of the ureteric bud |
| Ectopic ureter | Two ureteric buds develop from one mesonephric duct. One bud is in normal position; the abnormal bud moves downward with the mesonephric duct to enter into the urethra, vagina, vestibule, or uterus |
| Bladder exstrophy | Insufficiency of mesoderm of the ventral abdominal wall leading to abdominal ectodermal breakdown and degeneration of the anterior bladder wall; the bladder opens broadly onto the abdominal wall |
In the early embryo, the caudal portion of the primitive gut forms the hindgut. The hindgut extends from the posterior intestinal portal to the cloacal membrane and gives rise to the distal third of the transverse colon, the descending colon, the sigmoid, the rectum, and the upper part of the anal canal. The terminal portion of the hindgut enters into the cloaca, an endoderm-lined cavity that is in direct contact with the surface ectoderm. This boundary between the endoderm and ectoderm forms the cloacal membrane.
During further development, a transverse ridge called the urorectal septum arises from mesoderm between the allantois and the hindgut. This septum gradually grows caudad, thereby dividing the cloaca into an anterior portion, the primitive urogenital sinus, and a posterior portion, the anorectal canal. The primitive perineum is formed when the urorectal septum reaches the cloacal membrane when the embryo is 7 weeks old. At this time, the cloacal membrane ruptures, creating an anal opening for the hindgut and a ventral opening for the urogenital sinus.
Ectoderm on the surface portion of the cloaca proliferates and invaginates to create the anal pit. Degeneration of the anal membrane (formerly cloacal membrane) establishes continuity between the upper and lower anal canal. The upper part of the anal canal is thus endodermal in origin; the lower third of the anal canal is ectodermal. The junction between these regions is delineated by the pectinate line. The embryologic origin of the anus explains the differing blood and nerve supplies and epithelial cell types of the upper and lower anal canal.
The external anal sphincter appears in human embryos at approximately 7 to 8 weeks. This sphincter, together with the levator ani, is believed to originate from hypaxial myotomes. Although the anal sphincter and levator ani may arise from distinct primordia, their relationship is very close.
Imperforate anus is one of the more common abnormalities of the hindgut. In simple cases, the anal canal ends blindly at the anal membrane, which then forms a diaphragm between the endodermal and ectodermal portions of the anal canal. This occurs when the anal membrane fails to break down. In more severe cases, a thick layer of connective tissue may be found between the terminal end of the rectum and the surface because of either a failure of the anal pit to develop or atresia of the rectal ampulla. Vascular accidents in this region are the likely cause of rectoanal atresias. These vary greatly and present as a fibrous remnant or loss of a segment of the rectum or anus.
Rectourethral and rectovaginal fistulas are likely caused by abnormalities in the formation of the cloaca or urorectal septum. If the urorectal septum does not extend far enough caudally or shifts anteriorly, then the hindgut opens into the urethra or vagina, creating a fistula.
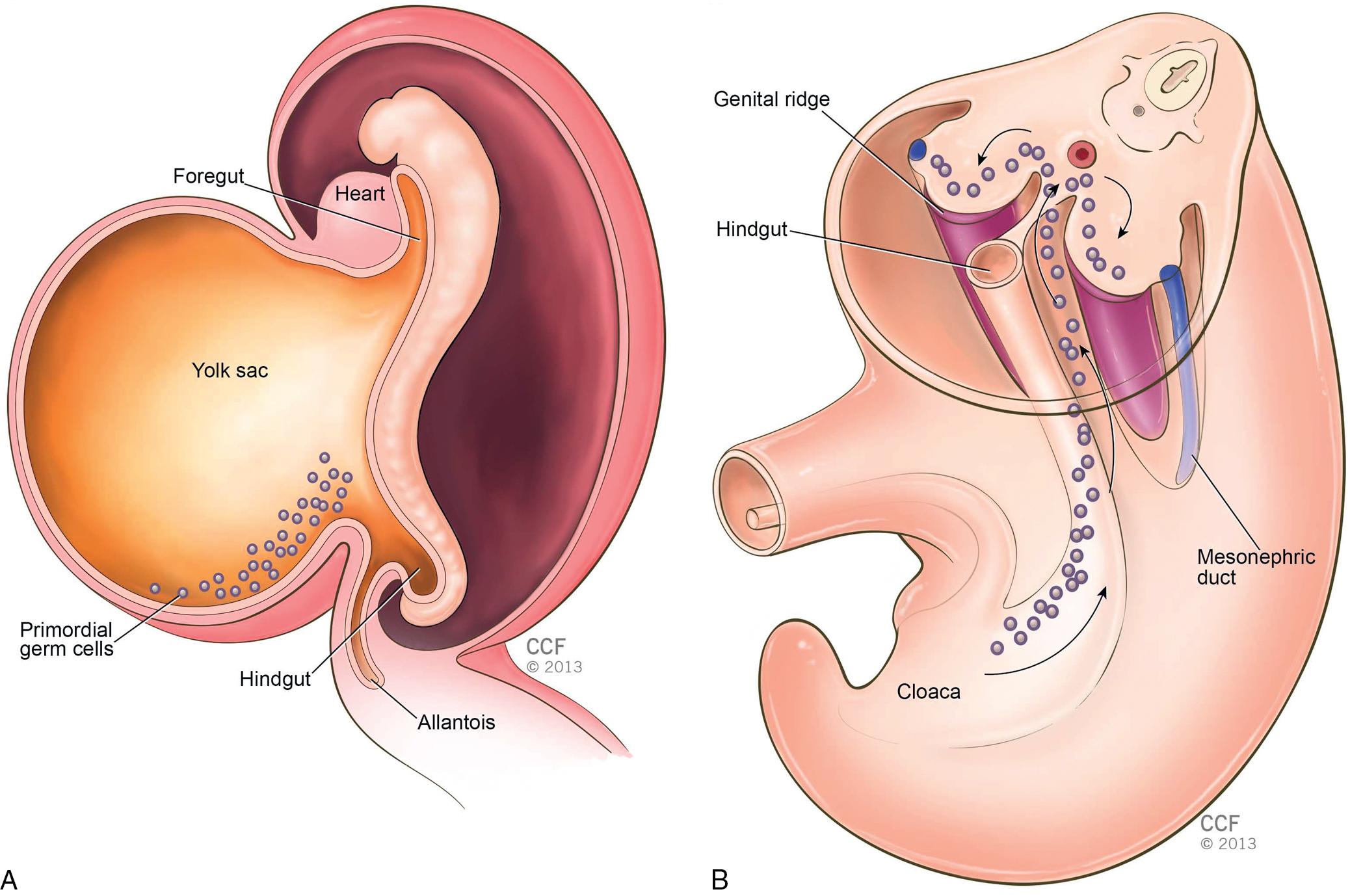
Gonads appear in early development as a pair of longitudinal ridges of steroidogenic mesoderm called the genital or gonadal ridges, which are formed by proliferation of the epithelium and condensation of the underlying mesenchyme. These initially do not contain germ cells. Primordial germ cells originate in the epiblast, migrate through the primitive streak, and by the third week reside in the posterior wall of the yolk sac ( Fig. 2.4 ). They then migrate along the dorsal mesentery of the hindgut and arrive at the primitive gonads at the beginning of the fifth week and invade the genital ridges in the sixth week. Approximately 1000 to 2000 primordial germ cells enter the genital ridges. If the primordial germ cells fail to reach the genital ridge, the gonads do not develop. In the female, once the primordial germ cells reach the genital ridge, they are called oogonia. Oogonia begin to proliferate at this stage and continue into the fourth month. Once these cells proliferate via mitosis, they are called oocytes.
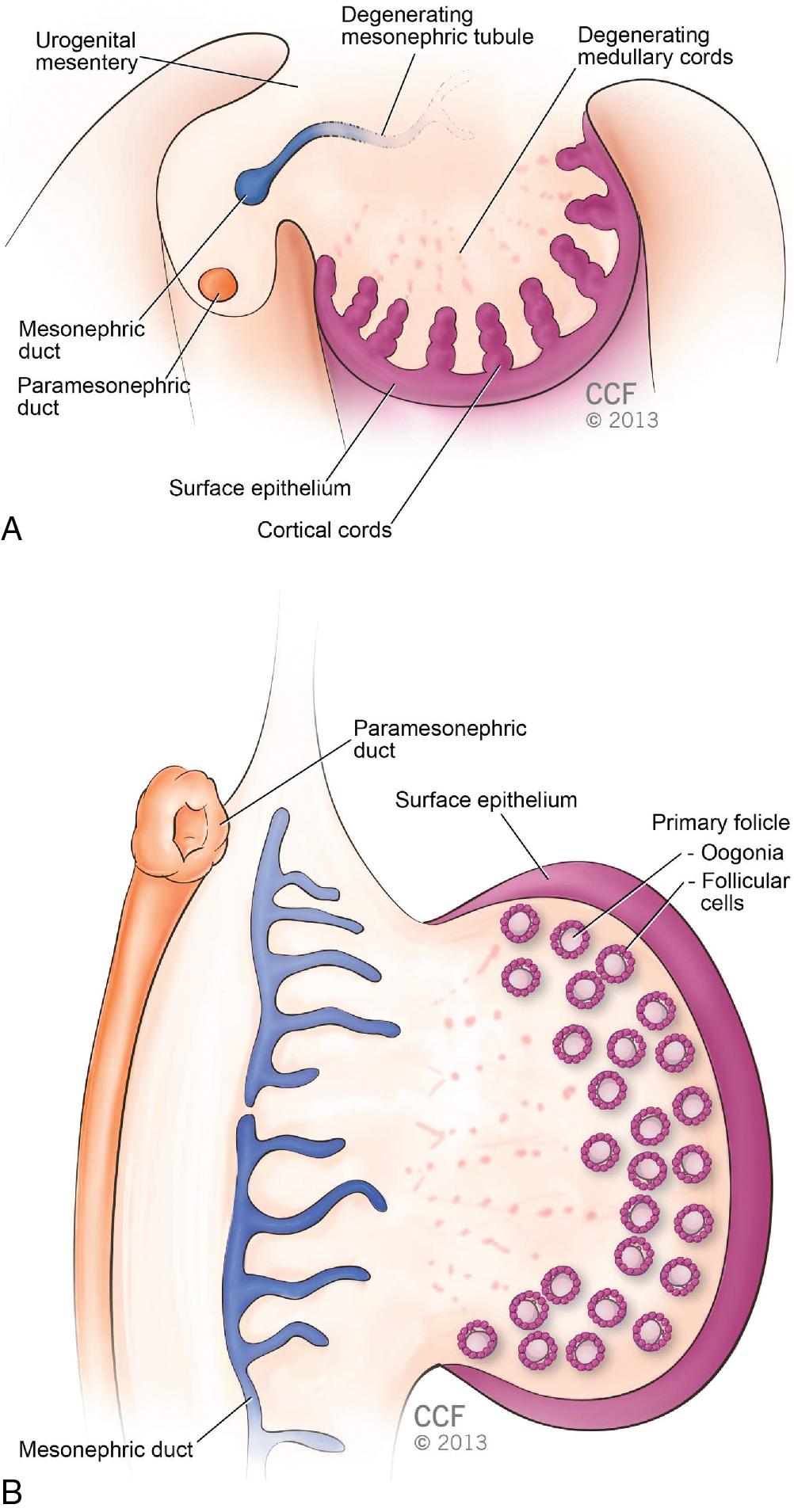
In the absence of the Y chromosome (XX or XO) and in the presence of the appropriate somatic cell environment, primitive sex cords (medullary cords) regress ( Fig. 2.5 A). However, the surface epithelium continues to proliferate and develops a second generation of cords called cortical cords. Cells in these cords surround each oocyte with a layer of epithelial cells called follicular cells. Together, the oocyte and follicular cells constitute a primary follicle ( Fig. 2.5 B). These enter meiosis until prophase I, when meiosis is arrested. The oocytes remain in this phase until ovulation, which may occur up to 50 years later.
As in gonadal development, the embryo genital ducts go through a sexually indifferent stage. Until approximately 8 weeks, both male and female embryos contain two pairs of genital ducts: paramesonephric (Müllerian) ducts and mesonephric (Wolffian) ducts. The paramesonephric ducts are a longitudinal invagination of the epithelium of the urogenital ridge. The ducts open cranially into the intraabdominal cavity and extend caudally. The paramesonephric ducts travel lateral to the mesonephric ducts and move medially, crossing the mesonephric ducts ventrally and coming into close contact in the midline. The paired paramesonephric ducts initially are separated by a septum but later fuse to form the uterine canal. Once these ducts are combined, the fused tip projects into the posterior wall of the urogenital sinus, where it causes a small swelling called the paramesonephric tubule. The mesonephric ducts open into the urogenital sinus on either side of this tubercle.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here