Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The respiratory system consists of conducting and gas exchange components, with the bifurcating airways and accompanying pulmonary arteries (PAs) bringing air and blood to peripheral capillary-lined airspaces for gas exchange. In understanding and evaluating pulmonary pathologic processes, it is useful to view the lung as consisting of multiple sets of branching trees including airways, arterial and venous pulmonary vasculature, systemic vasculature, and lymphatics. This chapter reviews the developmental biology, clinical anatomy, and pathophysiology of the respiratory system. Medical lung diseases in the neonate are used as illustrative examples, although the relevance of the discussion extends to the entire pediatric age group and beyond.
There are a large number of causes of newborn respiratory distress. They have been classified as congenital and acquired, medical versus surgical, and intrapulmonary versus extrapulmonary/extrathoracic. Chest radiographic findings are often nonspecific ( Table 48.1 ); close clinical correlation is needed for intelligent interpretation. This chapter will not exhaustively review neonatal lung disorders but rather selected conditions not covered elsewhere in this book that are relevant to the anatomy/physiology discussed.
| Pattern | Lung Disease * |
|---|---|
| Hazy granular |
|
| Confluent alveolar |
|
| Patchy opacities |
|
| Streaky interstitial |
|
* RDS, CHF, and TTN tend to be symmetric. Aspiration and hemorrhage tend to be asymmetric. Pneumonia can mimic almost all patterns.
The larynx, trachea, and bronchi develop from a ventromedial diverticulum of the foregut known as the laryngotracheal groove. Proliferation of the laryngeal mesenchyme produces arytenoid swellings that grow toward the tongue, converting the primordial glottis into a T -shaped laryngeal inlet. In the infant, the larynx is high in location, with its inferior border located at the C4 level. During childhood, the larynx descends and eventually reaches its adult location at the C6–C7 level by age 15 years. Functions of the larynx include breathing, phonation, and protection of the lower airway against aspiration.
The laryngotracheal groove grows caudally, forming the trachea. It lies ventral and parallel to the dorsal foregut, which becomes the esophagus. The separation of the trachea and esophagus progresses cranially and is complete by 6 weeks' gestation. The endodermal lining will produce the epithelium and glandular structures of the trachea, whereas the connective tissue, cartilage, and smooth muscle come from the surrounding splanchnic mesenchyme. Faulty separation of the trachea and esophagus gives rise to esophageal atresia/tracheoesophageal fistula (see Chapter 96 ). Disproportionate growth of the esophagus at the expense of the trachea may give rise to tracheal stenosis or, in the most severe form, tracheal agenesis (see Chapter 52 ).
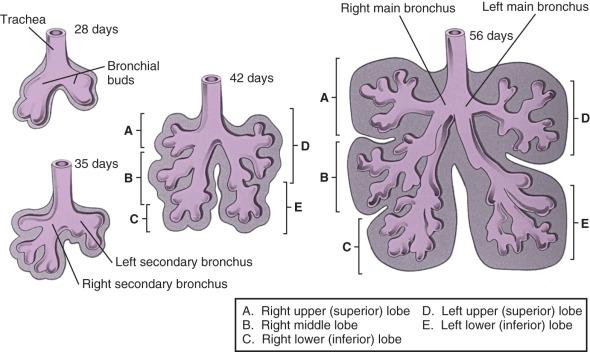
The lung bud arises from the caudal end of the laryngotracheal groove by the end of the fourth week and soon divides into two bronchial buds. The bronchial buds grow laterally into the pericardioperitoneal canals. Early in the fifth week, the connection of the bronchial buds to the trachea enlarges to form the mainstem bronchi. The right main stem bronchus bifurcates into a superior secondary bronchus, supplying the right upper lobe and an inferior secondary bronchus that subdivides into two bronchi, supplying the right middle and lower lobes. The left main stem bronchus divides into two secondary bronchi that supply the upper and lower lobes of the left lung. The bronchi continue to divide, and all airway divisions are complete by 16 weeks' gestation ( Fig. 48.1 ). Cartilage appears at 10 weeks in the trachea and is found in the segmental bronchi by 16 weeks. Unequal growth of the lung buds can lead to the development of unilateral pulmonary agenesis or hypoplasia. Prolonged oligohydramnios, space-occupying thoracic or abdominal lesions that compress one or both hemithoraces, chest wall deformities, neuromuscular disorders, and conditions producing PA hypoperfusion are associated with pulmonary hypoplasia.
Lung development has been divided into five stages ( Table 48.2 ). After completion of tracheobronchial and peripheral airway branching during the embryonic (26–52 days) and pseudoglandular (52 days–16 weeks) stages, the bronchi and terminal bronchioles enlarge during the canalicular stage (17–28 weeks). The capillary bed begins to approximate the future air spaces, and gas exchange is possible. Type I and type II pneumocytes can be identified in the fetal lung by 20 to 22 weeks, but the capillary-alveolar interface is not adequate for extrauterine survival until 23 to 24 weeks of gestation.
| Phase | Time of Occurrence | Significance |
|---|---|---|
| Embryonic | 26–52 days | Development of trachea and major bronchi |
| Pseudoglandular | 52 days to 16 wk | Development of remaining conducting airways |
| Canalicular | 17–28 wk | Development of vascular bed, framework of acinus; flattening of epithelium |
| Saccular | 29–36 wk | Increased complexity of saccules |
| Alveolar | 36 wk to term | Presence and development of alveoli |
The saccular stage (29–36 weeks) is characterized by the development of terminal air sacs with flattening of the epithelium in the distal air spaces. The type II pneumocytes produce surfactant, which is stored as lamellar bodies. During the alveolar stage (36 weeks to infancy), the size and number of alveoli increase. When birth occurs at full term, it is estimated that 50 million alveoli are present. Alveolar formation continues postnatally until about 8 years, with most development in the first 2 years of life. The mature human lung ultimately has 300 million alveoli. Further lung growth occurs via enlargement of existing lung components ( Table 48.3 ).
| 30 Weeks' Gestation | Full Term | Adult | Fold Increase After Birth | |
|---|---|---|---|---|
| Lung volume | 25 mL | 150–200 mL | 5 L | 23 |
| Lung weight | 20–25 g | 50 g | 800 g | 16 |
| Alveolar number | — | 50 m | 300 m | 6 |
| Surface area | 0.3 m 2 | 3–4 m 2 | 75–100 m 2 | 23 |
| Surface area/kg | 0.4 m 2 | 1 m 2 | 2.5 | |
| Alveolar diameter | 32 µm | 150 µm | 300 µm | 22 |
| No. of airways | 24 | 23–24 | 22–24 | 22 |
| Tracheal length | 26 mm | 184 mm | 7 | |
| Main bronchi length | 26 mm | 254 | 10 |
Acinar or alveolar dysplasia and alveolar capillary dysplasia (ACD) are rare, usually lethal disorders with early lung developmental arrest with lack of normal formation of terminal air spaces and distal vessels resulting in markedly impaired gas exchange. In ACD, there is often misalignment of the pulmonary veins centrally adjacent to pulmonary arterioles and bronchioles instead of their normal peripheral interlobular location (see Chapter 56 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here