Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Preoperative imaging
Intraoperative imaging
Postoperative imaging
Non-invasive evaluation of the heart is an essential part of the assessment of patients undergoing cardiac surgery. Echocardiography is the commonly used non-invasive imaging modality. Preoperatively, it is an essential part of the decision-making process to identify patients suitable for surgery, guide the type of surgical intervention and predict outcomes. Intra- and postoperatively, it is used to assess anatomy and function, and to detect early complications. This chapter provides a review of the echocardiographic anatomy of the heart from a surgical perspective.
Echocardiography uses ultrasound (US) waves to image tissues of various densities within the body. US is generated when the piezoelectric crystals housed within the transducer are stimulated by an electrical current. They propagate through the tissues as mechanical vibrations; when these strike structures with different acoustic densities, such as myocardium and blood, part of the energy is reflected back. The reflected signal is received by the transducer, converted to electrical energy and used for image creation. The location of the structure within the body is determined by the time taken by the US wave to travel back and forth from the transducer, and the brightness is dependent on its acoustic impedance.
There are several imaging modes – A mode, B mode, M mode, 2D, Doppler and 3D – and a comprehensive examination uses all the appropriate modalities to arrive at a conclusion. M mode echocardiography provides a single-dimensional view using a narrow beam of US across a small section of the heart. The motion of the structures within the US beam is displayed against time at a high temporal resolution. Two-dimensional echocardiography (2DE) uses multiple scan lines across a sector, producing a tomographic view corresponding to an anatomical section of the heart. Doppler echocardiography utilizes the change in frequency shift of a moving object to calculate velocity. Pressure (P) can be derived from velocity (V) using the modified Bernoulli equation ΔP = 4 V 2 .
Penetration of the sound wave and resolution of images depend on the frequency of US wave: lower frequencies achieve better penetration at the expense of reduced resolution and vice versa . Echocardiography uses US transducers with frequencies ranging from 2 to 7.5 MHz and the selection of transducer is based on the type of examination.
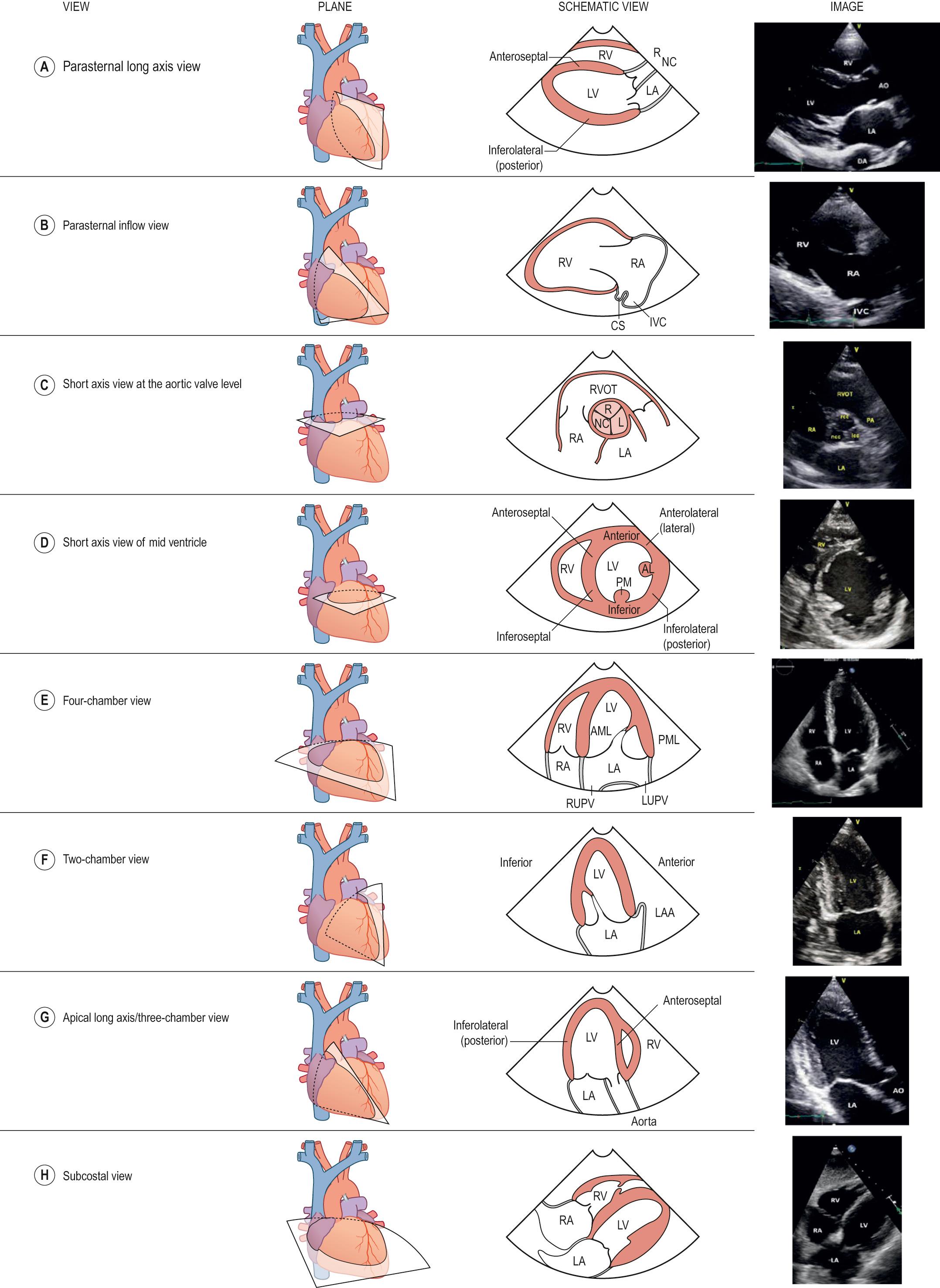
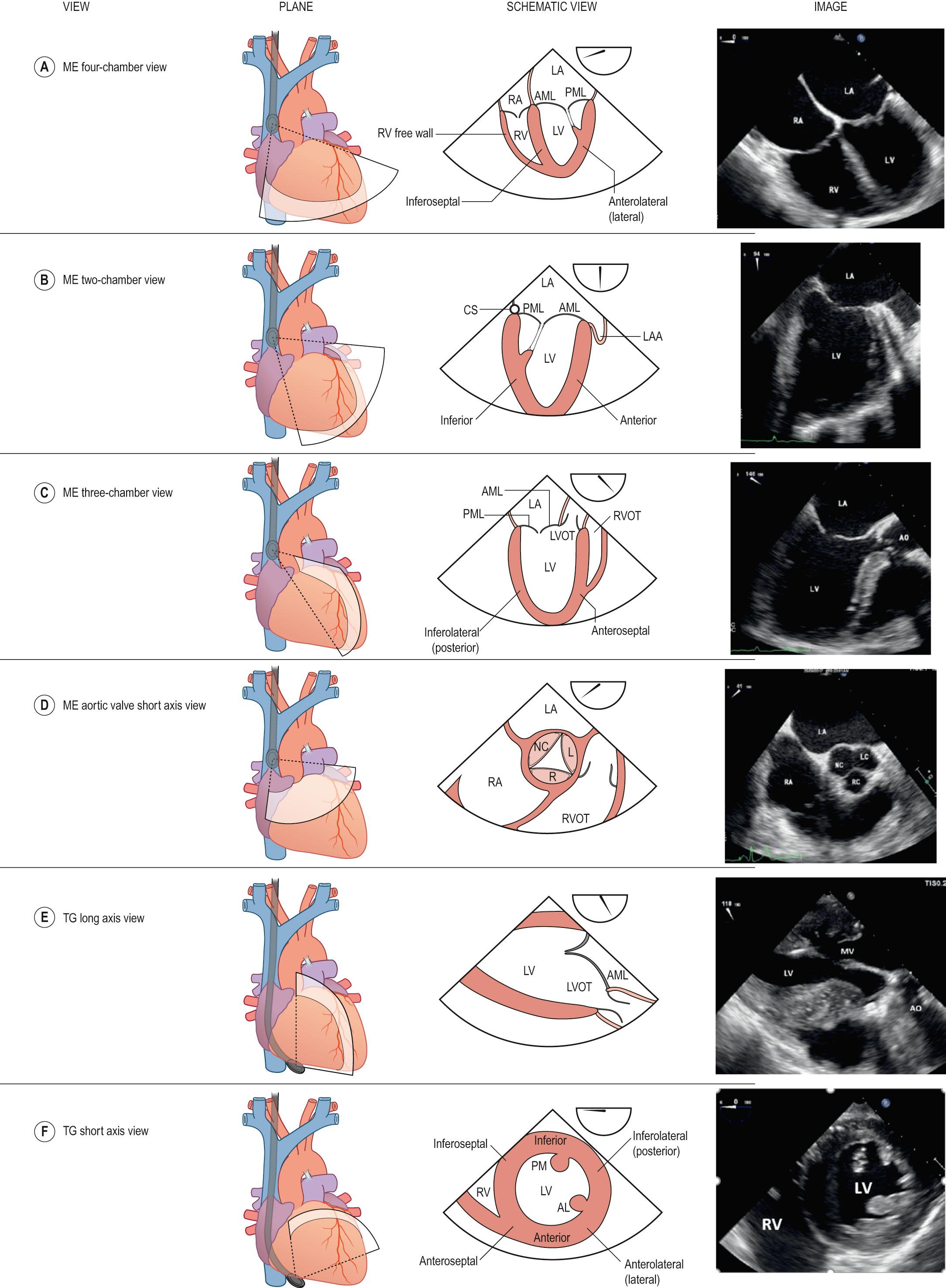
There are two types of examinations: transthoracic (TTE) and transoesophageal (TOE). The echocardiographic windows and planes ( Table 50.1 ; Figs 50.1 and 50.2 ) are different for both techniques but the basic principles of assessment remain the same. The choice of examination depends on the information required and the clinical setting. In general, a TOE examination is carried out in situations where the results of TTE are non-diagnostic, and commonly include evaluation of posteriorly located structures, the left atrial appendage, prosthetic valves and cardiac masses. TOE is also increasingly used to guide and monitor specific procedures, such as valve surgery and percutaneous intervention.
| Structure | TTE views | TOE views |
|---|---|---|
| Left ventricle | PS – LAX, SAX Apical views – 4C, 2C, 3C 3D echocardiography |
ME – 4C, 2C, 3C TG – SAX, LAX |
| Right ventricle | PS – LAX, SAX Apical – 4C (RV focused) Subcostal |
ME – 4C, RV inflow/outflow TG – SAX |
| Mitral valve | PS – LAX, SAX Apical – 4C, 2C, 3C 3D echocardiography |
ME – 4C, 2C, 3C, BCs TG – SAX, LAX |
| Left atrium and pulmonary veins | PS – LAX Apical – 4C |
ME – 0–120°, BC |
| Right atrium | Apical – 4C | ME – 4C, BC |
| Tricuspid valve | PS – LAX in flow view, SAX Apical 4C Subcostal |
ME – 4C, inflow/outflow, BC TG – SAX, LAX |
| Aortic valve | PS – LAX, SAX Apical 3C, 5C |
ME – 4C, 3C TG – SAX, LAX |
| Aorta | PS – LAX Apical – 3C Suprasternal |
ME – 3C TG – SAX, LAX |
The left ventricle (LV) has three components without clear anatomical boundaries. These are inlet and outlet portions separated by the mitral valve (MV), and a trabeculated apex. The interventricular septum (IVS) forms the medial wall of the LV and the other walls are referred to as anterior, inferior, inferolateral and anterolateral, based on their relation to the chest wall. In the anatomically normal heart, the LV is ellipsoid in shape; its base is attached to the mitral valve and its apex tapers to a conical cap. Myocardial wall thickness varies between 0.6 and 1.0 cm, being thickest at the base and thin towards the apex. The endocardium is normally irregular and trabeculated towards the apex.
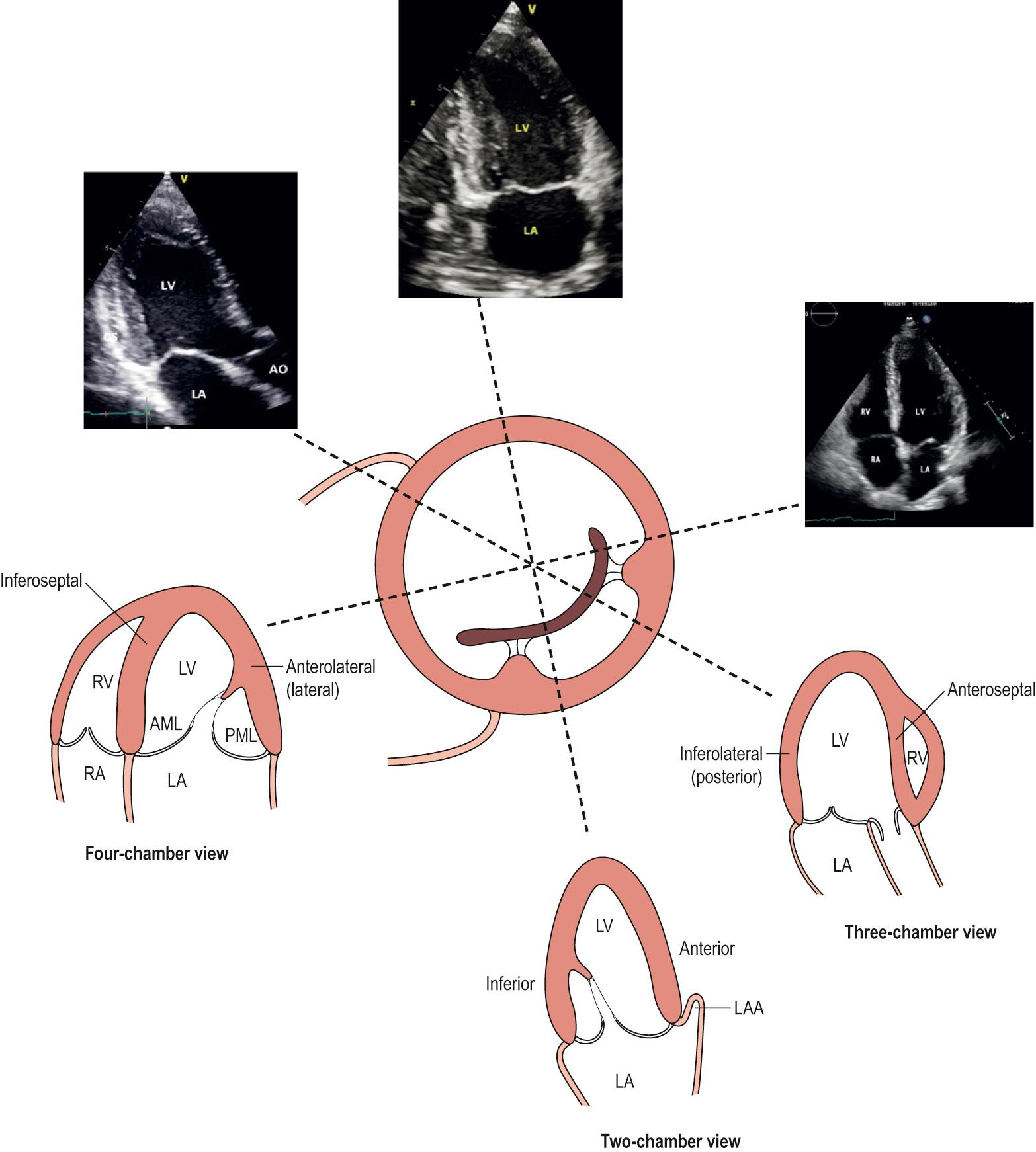
Echocardiographic imaging of the LV is usually done by TTE. TOE is rarely used to assess the LV alone, except during surgery or in the early postoperative period. Using 2DE, imaging is performed from long and short axis, apical and subcostal windows (see Table 50.1 ; Figs 50.1 and 50.2 ). The echocardiographic planes and the regional anatomy are shown in Fig. 50.3 . Comprehensive evaluation of the LV should include assessment of its geometry, size and regional and global function.
Alteration of LV morphology is seen in various disease states. With global dilation, the ventricle becomes more spherical, which results in reduced systolic performance and displacement of papillary muscles, causing functional mitral regurgitation. This is commonly seen in primary myocardial disease and volume overload conditions, whereas pressure overload states, such as aortic stenosis and hypertension, result in increased wall thickness, leading to concentric LV hypertrophy.
LV size is assessed by linear dimensions from the long axis views or volumes derived from apical views, and values are indexed to body surface area to define normality. Regional function is assessed using a 17-segment model that reflects different coronary artery territories. Each segment is analysed in systole and diastole for regional wall motion abnormality. Depending on the extent and severity of disease, myocardial segments can show reduced thickening, scarring or aneurysm formation. Acute transmural myocardial infarction can also result in rupture of the LV free wall, IVS or papillary muscle, causing cardiac tamponade, ventricular septal defect or acute mitral regurgitation. Rarely, rupture of the free wall can be contained by the pericardium, resulting in the formation of a pseudo-aneurysm. Various echocardiographic features can be used to differentiate between true and pseudo-aneurysm.
Global systolic function is assessed by calculating ejection fraction (EF), the percentage of chamber volume ejected in systole. Although three-dimensional echocardiography (3DE) is a superior technique for calculating volumes, 2DE is still the commonly used modality. Using 2DE, LV volumes are derived in end-systolic volume (ESV) and end-diastolic volume (EDV) by the biplane method of disks summation (modified Simpson's rule) from the apical windows, and EF is calculated by the following formula: EF = EDV−ESV/EDV.
Apical foreshortening and geometric assumptions limit the reproducibility of 2D in assessing volumes and function. 3DE is the recommended method for assessment of volume and function.
Fibromuscular bands called false tendons can be seen in the apical third of the LV cavity in certain patients. These are anatomical variants and should not be mistaken for thrombus or hypertrophy.
Regional dysfunction is a typical feature of coronary artery disease but can also be seen in other conditions.
Compared to the LV, the right ventricle (RV) has a more complex shape, with three distinct anatomical parts (inlet, apical and outlet) that are wrapped around the LV. The segmental nomenclature and coronary distribution are shown in Fig. 50.4 . The RV shares the IVS with the LV, which normally arches into the RV and is an important determinant of its shape. The free wall of the RV is thin compared to that of the LV, and measures 3–5 mm in thickness. Myocardial fibres are oriented predominantly in the longitudinal plane; hence, contraction is primarily longitudinal rather than radial.
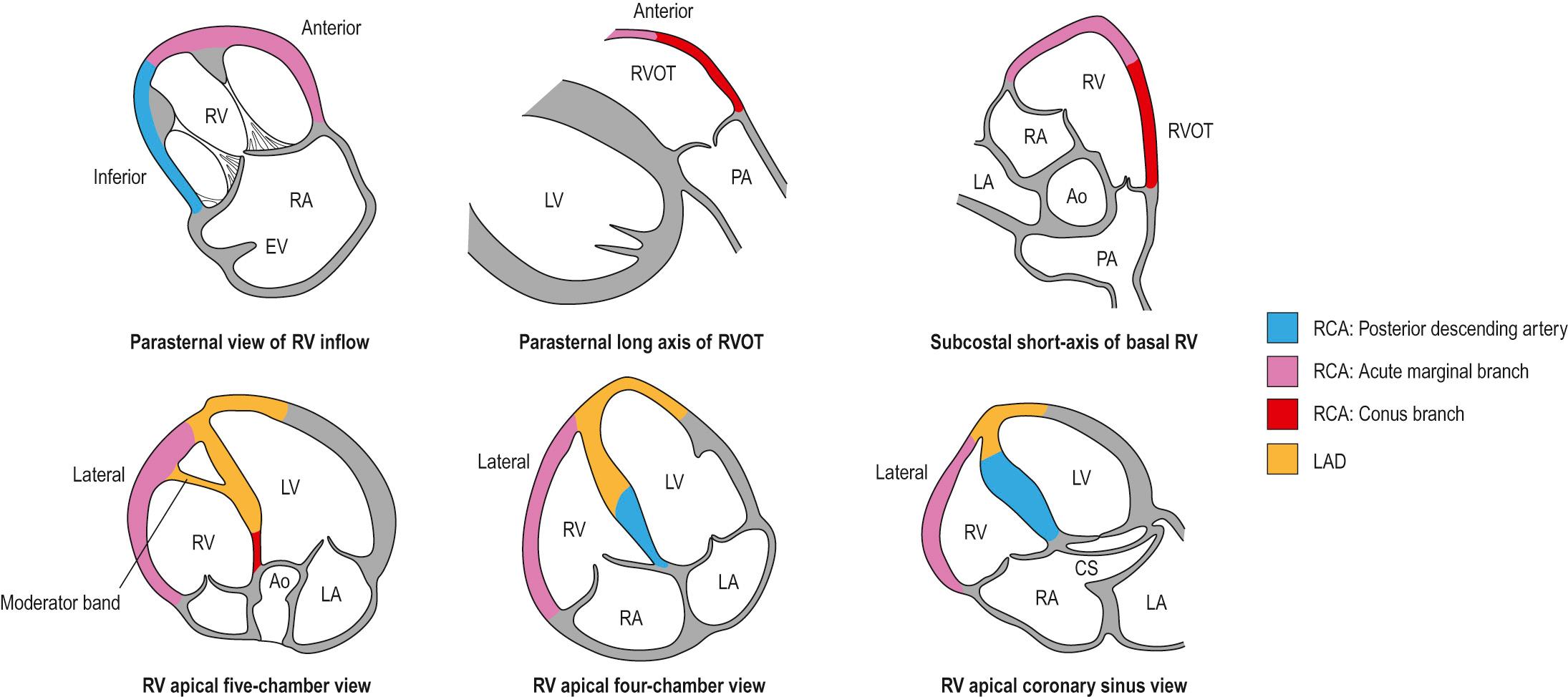
Due to its complex anatomy, echo assessment of the RV is carried out using TTE from multiple imaging planes (see Table 50.1 ; Fig. 50.1 ). TOE is rarely required for assessment of the RV alone, except in situations in which access to primary windows is limited, such as in ventilated patients or in those with severe chest deformity. Anatomically, the RV is identified by the following features: an apically displaced trileaflet atrioventricular (tricuspid) valve; heavily trabeculated endocardium; the moderator band; and three or more papillary muscles supporting the tricuspid valve leaflets. Like the LV, full evaluation of the RV should include assessment of its size, morphology and regional and global function.
RV size is usually assessed qualitatively in comparison to LV size and is done from the four-chamber view; the size of the RV is usually not more than two-thirds of the LV cavity in this view. The RV is considered moderately enlarged when its size is equal to that of the LV and severely enlarged if it exceeds that of the LV. With significant dilation, the RV may displace the LV and occupy the apex of the heart. Dilation can occur in volume and pressure overload conditions of the RV and should prompt a search for the aetiology, such as an atrial septal defect, tricuspid regurgitation, pulmonary regurgitation or elevated pulmonary artery pressures.
Volume and pressure overload states can also alter the shape and result in distinct contraction patterns of the IVS. Both conditions can cause flattening and leftward shift of the septum towards the LV. In pressure overload the shift is present throughout the cardiac cycle and is most pronounced at end-systole, whereas in volume overload conditions the shift is seen primarily in diastole with relative sparing in end-systole. A bouncing motion of the IVS during inspiration, referred to as septal bounce, is a sign of ventricular independence and is typically seen in constrictive pericarditis. Abnormal septal motion is also commonly seen in patients after cardiac surgery; the exact mechanism for this is not known.
Hypokinesis of the free wall can be due to global or regional dysfunction. Regional wall motion affecting the free wall can be seen in RV infarction, pulmonary embolism or cardiomyopathies. Global function of the RV is an important predictor of surgical outcome and should be assessed preoperatively. This is done qualitatively by visual assessment or semi-quantitatively using fractional area change (FAC), or by a non-volumetric method such as tricuspid anular plane systolic excursion (TAPSE). FAC is the percentage of area change within the RV between diastole (EDA) and systole (ESA), and is derived by the formula FAC = EDA–ESA/EDA × 100.
Simultaneous assessment of all parts of the RV is not possible from any view and therefore quantitative assessment of volume and function is not possible by echocardiography.
Abnormal contraction pattern of the IVS can cause difficulty in assessing RV function.
The left atrium (LA) is posteriorly located at the base of the heart. It has four components: a venous portion that receives four pulmonary veins (PVs); the left atrial appendage (LAA); the vestibule that opens into the mitral valve; and the interatrial septum (IAS) shared with the RA. The LAA is a finger-like projection located anterolaterally and is trabeculated by fine pectinate muscles. The LAA is multilobulated in the majority of hearts. The ridge between the LAA and left upper pulmonary vein is an infolding of the serous pericardium and is variably referred to as the posterolateral ridge, coumadin ridge or ligament of Marshall. The coronary sinus and the great cardiac vein run on the epicardial surface of the LA and occupy the left atrioventricular groove.
The LA is assessed using TTE from the parasternal short axis and apical windows (see Fig. 50.1 ; Table 50.1 ). These views help to image the walls of the LA, and to assess its size and any gross abnormalities such as a tumour or a large thrombus. The resolution of TTE is usually insufficient to visualize posterior structures (pulmonary veins and left atrial appendage) and this is undertaken using TOE.
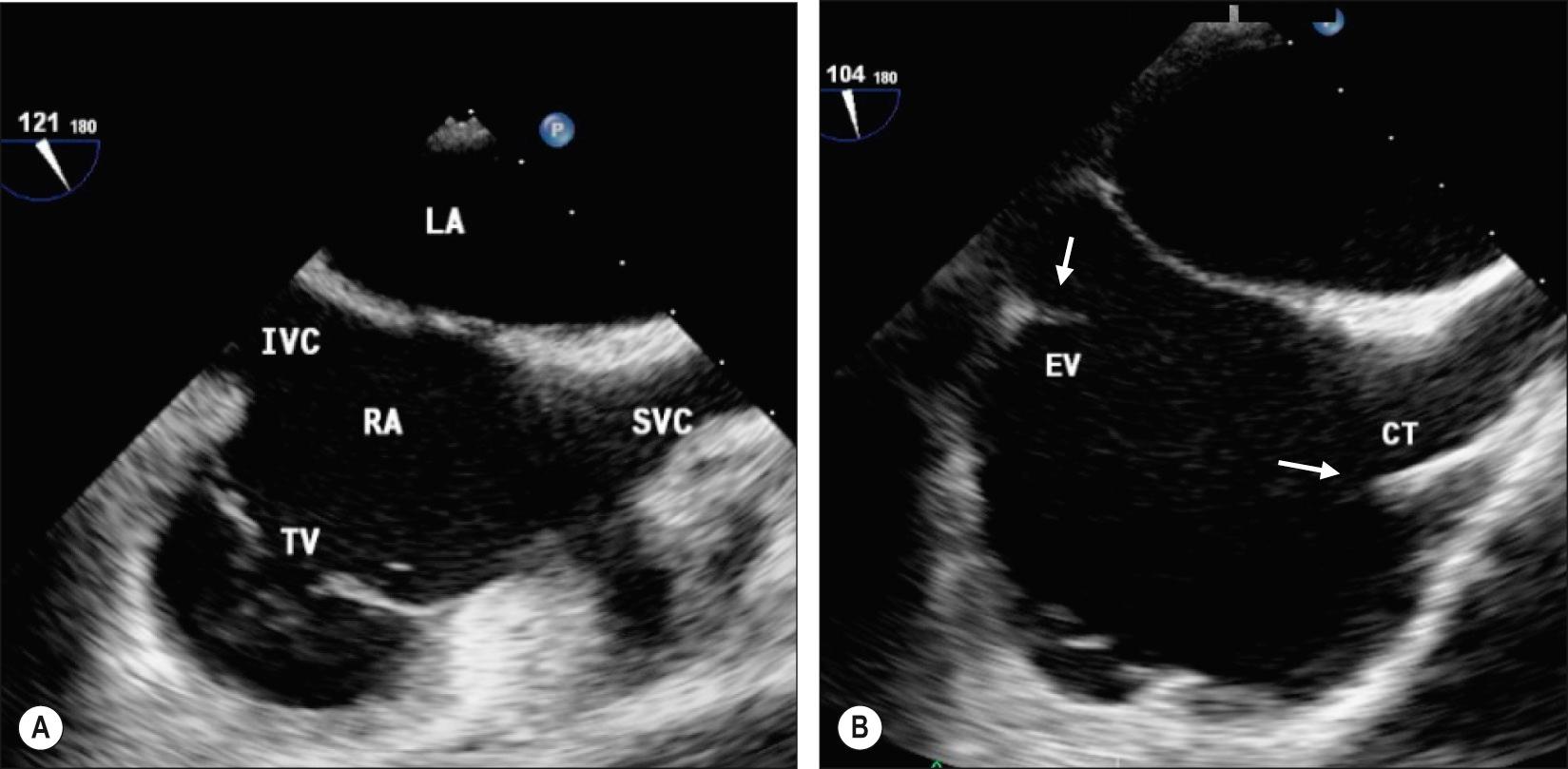
The LAA is imaged using TOE by electronically scanning between 0 and 120° in the mid-oesophageal (ME) position ( Fig. 50.5 ). Right-sided PVs are identified in the ME 0° or bicaval views. Left-sided PVs are close to the LAA and are best seen in the LAA views. In addition to identifying the normal pulmonary venous drainage, Doppler assessment of the PV can provide information on LA function and pressure.
Dilation of the LA is common in atrial fibrillation, MV disease and LV dysfunction, and is an important predictor of cardiovascular outcome. Left atrial size is measured using either linear dimensions or volumes obtained from multiple imaging planes. Dilation and remodelling associated with atrial fibrillation can result in stagnation and thrombus formation. Stasis of blood can cause a smoke-like appearance within the LA, termed ‘spontaneous contrast’, while thrombus is identified as a well-circumscribed echogenic structure with uniform consistency. Thrombus formation typically occurs within the region of the LAA. Apart from thrombi, the LA can be a site for intracardiac masses, especially myxoma.
The LAA has multiple lobes and scanning in multiple planes is important to assess all the lobes.
Pectinate muscles within the LAA and the posterolateral ridge can be mistaken for thrombus, and careful evaluation of the LAA from multiple imaging planes using 2D/3D and Doppler echocardiography is required to identify a true thrombus.
LA dilation can be asymmetric and linear measurements should be carried out in multiple planes to assess the size.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here