Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In an 1866 report titled “Concerning a very rare case of insufficiency of the tricuspid valve caused by a congenital malformation,” Dr. Wilhelm Ebstein (1836-1912), a German physician, described the unusual cardiac findings of a 19-year-old laborer who died of cyanotic heart disease. He accurately described the characteristic anatomic and hemodynamic abnormalities of Ebstein malformation ( Fig. 130-1 ). By 1950, only three case reports of Ebstein malformation had been published.
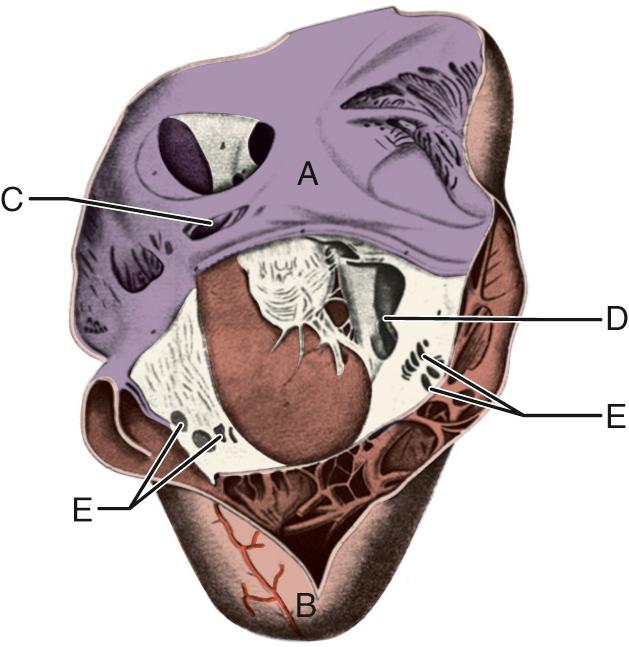
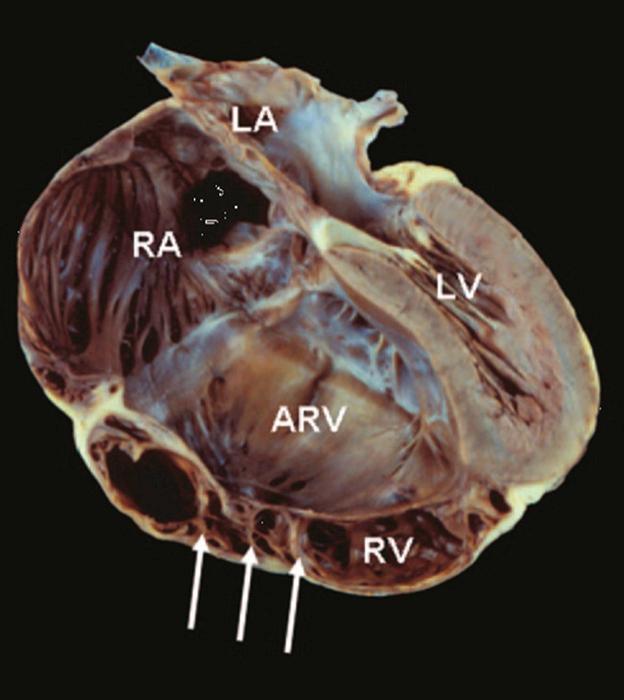
Ebstein malformation of the tricuspid valve (TV) is characterized by ( Fig. 130-2 ):
Failure of delamination of the septal, inferior, and anterior leaflets of the TV with subsequent adherence of the leaflets to the underlying myocardium
Apical displacement of the functional TV annulus (septal>inferior>anterior)
Dilation of the atrialized portion of the right ventricle (RV)
Anterior leaflet fenestrations, redundancy or tethering
Dilation of the true anatomic TV annulus
There is a highly variable TV morphology; the valve is almost always incompetent, and rarely stenotic. The anterior leaflet is usually large and is attached to the annulus; however, it may contain several fenestrations ( Fig. 130-3 ) and have various points of incomplete delamination. The chordae tendinea may be short and poorly formed.
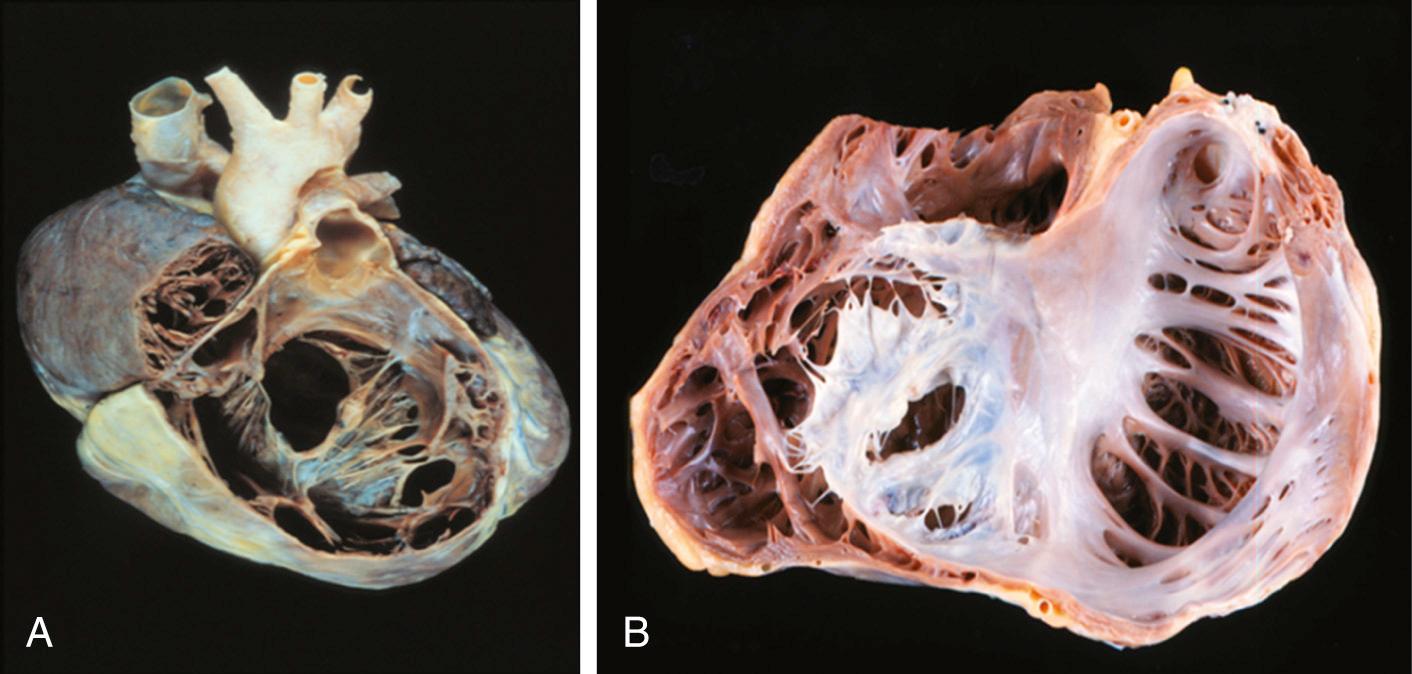
The inferior and septal leaflet development is variable and most often rudimentary and may even be absent due to failure of the delamination process. The leading edges may be freely mobile with chordal or papillary muscular support, or they may be tethered (adherent) to the endocardium (linear attachment). The point of maximal displacement is at the commissure between the inferior and septal leaflets. In normal hearts, the downward displacement of the septal and posterior leaflets in relation to the anterior mitral valve leaflet is less than 8 mm/m 2 body surface area. The spectrum of abnormality in Ebstein malformation can range from only minimal displacement of the septal and inferior leaflets to an imperforate membrane or muscular shelf between the inlet and trabecular zones of the RV. The range of variability is infinite, and the most important pathologic finding is “failure of delamination” of the leaflets. There often is marked dilation of the true TV annulus, which is not displaced, and a large chamber separating the true annulus from the functional RV is the “atrialized” portion of the RV (aRV).
The RV is divided into two regions: the area involved with the malformation (i.e., the inlet portion or the aRV) that is functionally integrated with the right atrium (RA), and the area that is not involved by the malformation and consists of the other two components of the RV—the trabecular and outlet portions, which constitute the functional RV. The “atrialized” portion of the RV can become disproportionately dilated and may account for more than half of the RV volume. The majority (>  ) of hearts with Ebstein malformation have RV dilation. Dilation often involves not only the atrialized inlet portion of the RV but also the functional RV apex and outflow tract. In some cases, RV dilation is so marked that the ventricular septum is deviated leftward, compressing the left ventricular (LV) chamber. In such cases, the short-axis view demonstrates a circular RV and a D-shaped LV.
) of hearts with Ebstein malformation have RV dilation. Dilation often involves not only the atrialized inlet portion of the RV but also the functional RV apex and outflow tract. In some cases, RV dilation is so marked that the ventricular septum is deviated leftward, compressing the left ventricular (LV) chamber. In such cases, the short-axis view demonstrates a circular RV and a D-shaped LV.
The most common associated cardiac defects include :
Atrial septal defect (ASD): either patent foramen ovale or an ASD, mostly secundum, is present in 80% to 94% of the patients
Ventricular septal defect with or without pulmonary atresia
RV outflow tract obstruction: this can occur secondary to structural abnormalities (pulmonary valve stenosis or pulmonary atresia), branch pulmonary artery stenosis, and rarely the displaced TV
Patent ductus arteriosus
Coarctation of the aorta
Accessory conduction pathways (Wolff-Parkinson-White [WPW] syndrome) are present in up to 15% to 20% of patients and may predispose patients to arrhythmias. The majority of these pathways are located around the orifice of the malformed TV.
Left-sided lesions (uncommon)
Mitral valve prolapse
Accessory mitral valve tissue
Subaortic stenosis
Bicuspid or atretic aortic valve
Muscle bands in the LV cavity
Myocardial changes resembling LV non-compaction
Congenitally corrected transposition of the great arteries (cc-TGA): In patients with cc-TGA, an abnormal systemic atrioventricular valve (morphologic TV) that fulfills the criteria of Ebstein valve is present in 15% to 50% of cases. This Ebsteinoid displacement of the TV into the morphologic RV is different from the classic right-sided Ebstein malformation in that there is usually lack of atrialization of the RV free wall.
Several classifications have been proposed for Ebstein malformation. In general, classification systems of Ebstein malformation are difficult since there are infinite variations in the anatomy and no two hearts are alike.
Carpentier in 1988 proposed the following :
Type A: the volume of the true RV is adequate
Type B: a large atrialized component of the RV exists, but the anterior leaflet of the TV moves freely
Type C: severe restriction of the anterior leaflet movement that can cause significant RV outflow tract obstruction
Type D: near complete atrialization of the ventricle except for a small infundibular component
Another classification proposed four types of Ebstein malformation based on valve analysis during surgery. This is our preferred approach, which is to describe the exact anatomy of each of the involved structures of the heart as visualized at the time of surgery ( Table 130-1 ). This includes comment about the extent of failure of delamination of each leaflet, status of the leading edges of the leaflets, degree of displacement of the septal leaflet, description of the aRV, and size of the RA and RV.
| Type | Anterior Leaflet | Posterior Leaflet | Septal Leaflet | Atrialized RV Chamber Size | |
|---|---|---|---|---|---|
| Size | Mobility | ||||
| I | Larger | Mobile | Apically displaced, dysplastic, or absent | Varies from relatively small to large | |
| II | Relatively small and displaced in a spiral fashion toward the apex | Moderately large | |||
| III | Restricted motion; shortened, fused, and tethered chordae; direct insertion of papillary muscles into the anterior leaflet is frequently present | Displaced, dysplastic, and usually not reconstructible | Large | ||
| IV | Severely deformed; displaced into the RVOT; few or no chordae; direct insertion of the papillary muscles into the leading edge of the valve is common | Typically dysplastic or absent | Represented by a ridge of fibrous material descending apically from the membranous septum | Nearly the entire RV cavity is atrialized; TV tissue is displaced into the RVOT and may cause obstruction of blood flow (functional tricuspid stenosis) | |
Genetic factors in Ebstein malformation are heterogeneous. Most cases are sporadic and familial Ebstein is rare. Rare cases of cardiac transcription factor NKX2.5 mutations, 10p13-p14 deletion, and 1p34.3-p36.11 deletion have been described in association with Ebstein malformation. The results of a mutational analysis in a cohort of 141 unrelated probands with Ebstein malformation has been reported; eight were found to have a mutation in the gene MYH7, and six of the eight patients also had LV noncompaction. This result may warrant genetic testing and family evaluation in this subset of patients.
The functional impairment of the RV and the incompetence of the deformed TV retard forward flow of blood through the right side of the heart into the lungs. Moreover, during contraction of the atrium, the atrialized portion of the RV (which is adjacent to and in continuity with the RA) balloons out (if very thin) or acts as a passive reservoir, thus decreasing the volume to be ejected. During ventricular systole, the atrialized RV contracts, creating a pressure wave that impedes venous filling of the RA, which is in the diastolic phase. In most cases, there is a communication between the left and right atria, resulting from either patency of the foramen ovale or a distinct secundum ASD. The shunt of blood through the septal opening is generally from right to left, but may be bidirectional in some patients. The overall effect of these structural abnormalities on the RA is to produce gross dilation, which may reach enormous proportions, even in infants. This dilation leads to further incompetence of the TV and further widening of the interatrial communication.
As a consequence of atrial dilation, atrial tachyarrhythmias are common and become more likely as time goes on. In addition, approximately 15% of patients will have one or more accessory conduction pathways associated with WPW syndrome, and 1% to 2% of patients will have atrioventricular nodal reentrant tachycardia (AVNRT). In end-stage heart failure, ventricular arrhythmias can be present.
Clinical presentations vary widely, because they depend on the anatomic severity and can range from a severely symptomatic neonate to an asymptomatic octogenarian.
The most common presentation varies with age at presentation :
Fetuses: an abnormal routine prenatal scan (86%)
Neonates: cyanosis (74%)
Infants: heart failure (43%)
Children: an incidental murmur (63%)
Adolescents and adults: arrhythmia (42%), decreased exercise tolerance, fatigue, or right-sided heart failure
Secondary to significant tricuspid regurgitation
Can appear soon after birth, because of high pulmonary vascular resistance
Often improves as pulmonary vascular resistance decreases
Can occur at a later age
Can recur and can be insidious in onset
Secondary to atrial tachyarrhythmia (atrial flutter and fibrillation most common)
May be present in 20% to 30% of cases
Some of these arrhythmias are due to WPW syndrome
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here