Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Management of early-onset scoliosis (EOS) requires an understanding of not only spinal deformity but also of the natural history and growth of the spine, thorax, and lungs.
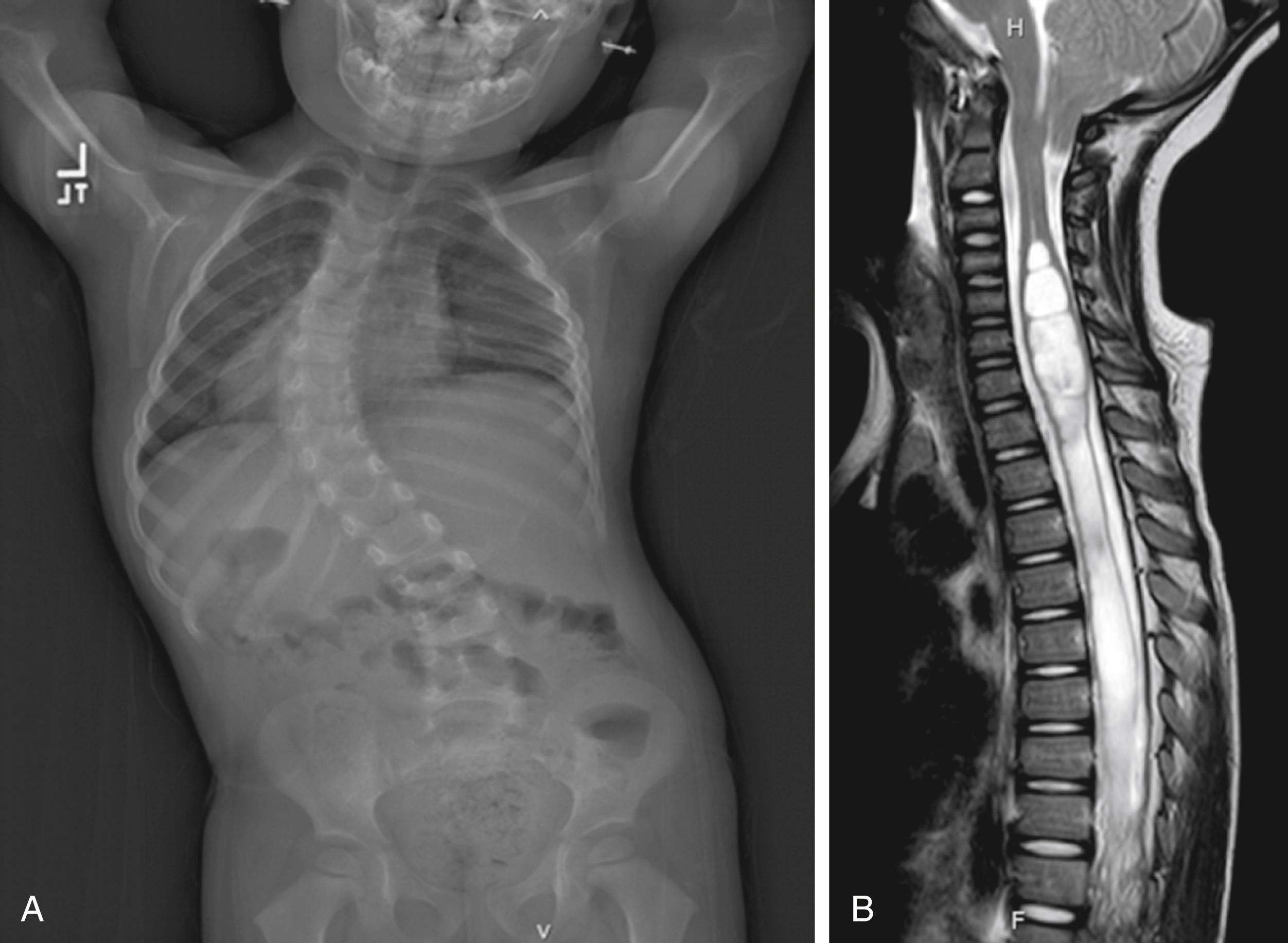
Idiopathic EOS is a diagnosis of exclusion and should not be presumed. Magnetic resonance imaging is recommended in EOS because 13% to 25% of presumed idiopathic EOS cases will have an underlying anomaly identified on imaging.
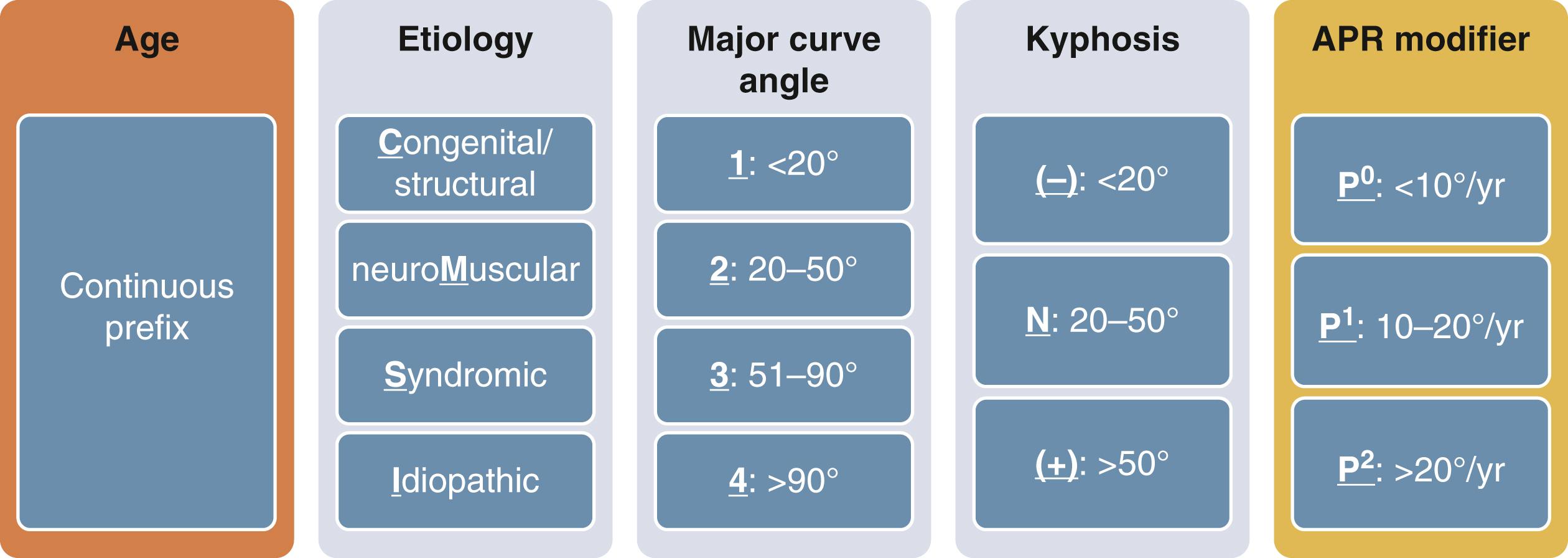
The Classification of Early-Onset Scoliosis should be used to facilitate treatment, communication, and research.
Elongation-derotation-flexion/Mehta casting is an effective treatment for EOS, but results differ between idiopathic and nonidiopathic populations. Casting should begin once progression is clear, as results decline if casting is begun after 18 months of age in idiopathic EOS. Bracing results have yet to match those of casting.
No consensus exists on when to transition to operative treatment, but it is clear that delay, as long as there is not undue progression of scoliosis, is beneficial. Complication rates decline with each additional year of delay. We begin to consider transition to operative treatment when scoliosis reaches 60 to 70 degrees.
Resection and short fusion may be considered earlier for children with congenital EOS, such as an isolated hemivertebra.
Surgical options include distraction-based and compression-based techniques, and also guided growth. Distraction-based techniques are currently most widely used, with magnetically expandable control rods an option. Spine-based and rib-based thoracic fixation are options in distraction-based surgery.
Early-onset scoliosis (EOS) is broadly defined as scoliosis with onset before 10 years of age. Defining EOS based on age of onset seeks to acknowledge the very different natural history of EOS in contrast to that of adolescent idiopathic scoliosis. Progressive untreated EOS is associated with a shortened lifespan owing to progressive restrictive pulmonary dysfunction and ensuing cardiopulmonary compromise. , Within the broad age range encompassed by the current cut-off point of 10 years of age there are certainly large differences in prognosis––9 years of age at onset of scoliosis is clearly not the same as 2 years of age. The purpose of this chapter is to review the natural history of EOS, consequences of deformity on pulmonary development and spinal growth, and treatments including bracing, casting, and operative care.
The Classification of Early-Onset Scoliosis (C-EOS) is the current standard classification system for EOS, and has been shown to have excellent interobserver and intraobserver reliability. , The key element of the C-EOS is etiology which can be classified as congenital/structural, neuromuscular, syndromic, or idiopathic ( Fig. 20.1 ). Further subclassification is based upon age as a continuous variable, magnitude of scoliosis, kyphosis, and annual progression rate. From a management perspective, the key determination is often binary: idiopathic versus nonidiopathic EOS. In an effort to facilitate communication and research efforts, consensus-based classification systems have also been created for growth-friendly spine implants and complications of growing spine surgery. ,
A thorough history and physical examination are required on initial assessment of the child with EOS. Idiopathic EOS is a diagnosis of exclusion, and signs and symptoms indicative of a nonidiopathic etiology may manifest over time. A referral to a geneticist can be very helpful. Ideally, radiographs are upright and biplanar; however, this may not be possible for the youngest children or those with developmental delays. Standing radiographs are preferred to sitting, and sitting are preferred to supine. Supine traction films are not routinely necessary; however, they can provide clarity in terms of better revealing the bony anatomy and providing a more objective assessment of the flexibility of the deformity. They are often helpful with surgical decision-making. Neural axis anomalies (NAAs) have been identified in 13% to 25% of children with presumed idiopathic EOS ( Fig. 20.2 ). In a study of children with presumed idiopathic EOS younger than three years of age, there was a 39% incidence of NAA in those with a scoliosis 29.5 degrees or greater (13/33) as opposed to 0% in those with smaller magnitudes of scoliosis (0/20). This provides a useful guideline for when to obtain magnetic resonance imaging (MRI), but caution is advised because the sample size is small. We also obtain an MRI in all children with atypical deformities, increased kyphosis, progressive deformity, and congenital scoliosis, and in those with abnormalities on neurological examination or comorbid conditions in which NAAs are common. MRI is recommended prior to initiating any treatment, including bracing or casting. MRI can often be coordinated with the first cast application to reduce anesthetics.
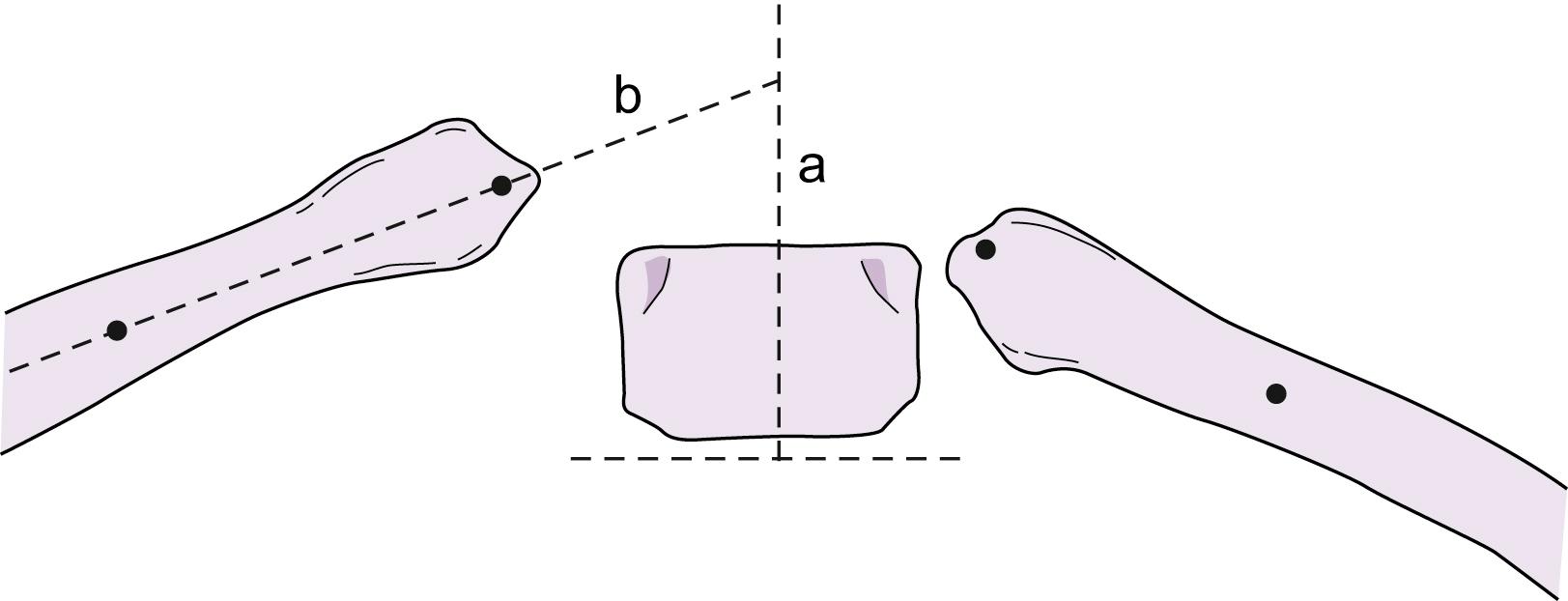
When considering treatment of children with idiopathic EOS (historically “infantile idiopathic scoliosis”) one must differentiate between progressive and spontaneously resolving curvatures. Idiopathic EOS is slightly more common in males and often presents with a left thoracic deformity. Spontaneous resolution may occur in up to 90% of patients. A rib-vertebral angle difference (RVAD) of less than 20 degrees at the apical vertebrae was associated with spontaneous resolution of scoliosis in 83% of cases, whereas 83% of those with an RVAD 20 degrees or greater were progressive ( Fig. 20.3 ). Scoliosis 20 degrees or greater, thoracolumbar curves, phase 2 ribs, and double major curves are also associated with progression.
Campbell defined thoracic insufficiency syndrome (TIS) as the inability of the thorax to support normal respiration or lung growth. Factors which contribute to TIS include spinal deformity, chest wall deformity, and impairment of chest wall mechanics. Management of EOS is focused upon avoiding or mitigating TIS, which requires an understanding of spinal growth, growth of the thorax, and pulmonary development.
The spine grows at variable rates during childhood and adolescence. Diméglio’s work found increases in thoracic height of 1.4 cm per year from birth to age 5 years, 0.6 cm per year from 5 to 10 years, and 1.2 cm per year between age 10 years and skeletal maturity. , Longitudinal growth of the thoracic spine, or thoracic height, is only one component of thoracic growth. In children without spinal deformity, thoracic volume at the age of 4 years is 33% of adult thoracic volume, reaching 55% at the age of 10 years. Thoracic volume triples between ages 4 and 16 years and doubles between ages 10 and 16 years. Pulmonary development is dependent upon sufficient volumetric growth of the thorax. Initial volumetric growth of the thoracic is a result of alveolar hyperplasia, which peaks between birth and age 2 years, and ends by 8 years of age. , Further increases in pulmonary, and thus thoracic, volume are a consequence of alveolar hypertrophy.
Historically, management of EOS focused on control of spinal deformity, often proceeding to early spinal fusion to create a straight, but short, spine. Studies demonstrating impaired pulmonary function in children who underwent early fusion, as well as increasing understanding of TIS, have modified current treatment goals towards preservation and promotion of growth, while maintaining control of spinal deformity. There is also an evolving consideration of the potential impact of treatments upon chest wall mechanics. Thoracic height and total spine length have been proposed as convenient measurements, which may help guide treatment. , “Sufficient” values from these measurements have yet to be determined, and they should not be goals in and of themselves, given that respiratory mechanics vary between patients based upon the heterogeneous nature of EOS and the various treatment options available.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here