Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In 1941, Dobbie was the first to report the results of surgical reattachment of the distal biceps tendon. He recommended routine tenodesis of the biceps to the brachialis because of the risks associated with anatomic repair from the surrounding neurovascular structures within the antecubital fossa. Improved surgical techniques and a better understanding of the anatomy and biomechanics of the distal biceps tendon subsequently changed this sentiment. Many orthopedic surgeons now advocate early anatomic surgical repair of the distal biceps tendon in young, active patients.
Controversies continue to exist regarding the optimal treatment of distal biceps tendon ruptures. Many of these controversies focus on patient selection, approach to the radial tuberosity, and tendon fixation techniques. The first half of this chapter reviews the relevant pathoanatomy, workup, and treatment of patients with distal biceps tendon ruptures. The second half of the chapter focuses on triceps tendon rupture and repair.
The estimated incidence of distal biceps tendon ruptures has risen from 1.2 to 2.55 per 100,000 population per year according to a recent epidemiologic analysis. Distal ruptures account for only 3% of biceps brachii tendon injuries. The injury is most commonly seen between the fourth and sixth decades of life, with an average age of approximately 50 years (range, 18 to 72 years). Several patient factors have been associated with distal biceps tendon ruptures, with the most significant factor being male sex. Eighty-six percent of distal biceps tendon ruptures occur in the dominant extremity, and they typically occur in highly active people, often with elevated body mass indices. Poisson regression analysis of tobacco use yields a 7.5 times increased risk of distal biceps tendon rupture among persons who smoke. Middle-aged men who use nicotine and anabolic steroids have a higher incidence of bilateral injuries.
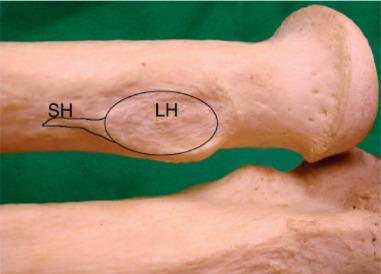
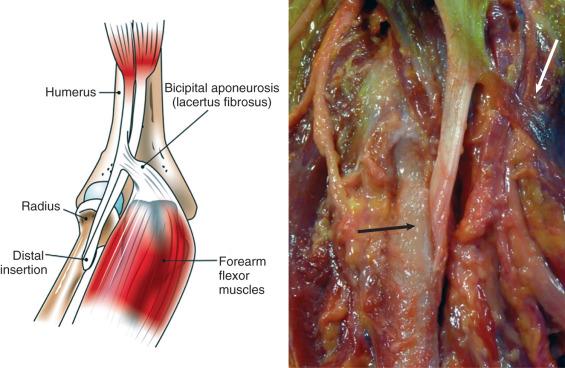
The biceps brachii muscle is contained in the anterior compartment of the arm and is composed of two heads. The long head originates from the supraglenoid tubercle within the shoulder joint, and the short head originates from the coracoid process. The two heads converge at the level of the deltoid tuberosity. The distal tendon gives rise to the lacertus fibrosus (bicipital aponeurosis) before passing deep through the antecubital fossa and inserting onto the radial tuberosity. Anatomic investigation of the distal tendon reveals two distinct attachment sites, with a mean length of 92 mm and a mean width ranging from 2.9 to 6.1 mm. The tendon of the short head, which is more significant, attaches more distally on the tuberosity, and biomechanically acts as a flexor. The tendon of the long head inserts further from the axis of rotation of the forearm and acts as a strong supinator ( Fig. 62.1 ). The lacertus fibrosus spreads out in an ulnar direction and blends into the forearm fascia, ultimately inserting onto the subcutaneous border of the ulna ( Fig. 62.2 ). This aponeurosis may provide stability to the distal tendon.
Innervation of the biceps brachii is via the musculocutaneous nerve, a branch of the lateral cord of the brachial plexus. It penetrates the biceps muscle at an average of 134 mm distal to the acromion and travels between the biceps and the brachialis before it penetrates the deep fascia of the arm and becomes the lateral antebrachial cutaneous nerve, which supplies sensation to the volar-lateral aspect of the forearm.
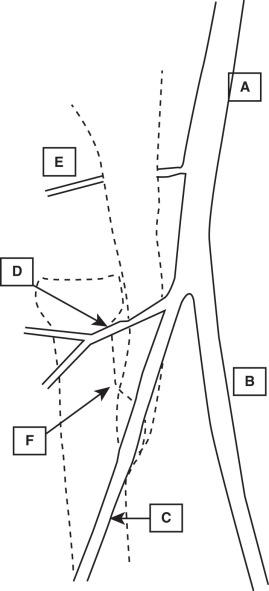
The biceps brachii is in close proximity to many vital neurovascular structures. The brachial artery, brachial vein, and the median nerve lie just medial to the biceps tendon and directly underneath the lacertus fibrosus. The brachial artery bifurcates into the radial and ulnar arteries at the level of the radial head. The radial recurrent artery arises from the radial artery and crosses laterally through the antecubital fossa, lying within the typical surgical field ( Fig. 62.3 ). Lateral to the biceps tendon, the radial nerve enters the proximal forearm between the brachialis and the brachioradialis. The radial nerve divides into the deep and superficial branch anterior to the lateral humeral condyle.
Owing to its dual insertion onto the radial tuberosity, the biceps muscle provides power and endurance for forearm supination and assists the brachialis in elbow flexion. The extent to which the biceps brachii contributes to elbow flexion correlates with the position of the forearm, with increasing contribution as the forearm is supinated. Furthermore, the biceps is able to exert maximum supination strength with the elbow at 90 degrees of flexion.
Morrey et al. performed a biomechanical study of 10 patients to evaluate the differences between conservative management and operative reattachment of distal biceps tendon ruptures. Immediate surgical fixation of the tendon to its insertion ultimately restored normal elbow flexion and forearm supination strength. In the group treated conservatively, an average loss of 40% supination strength and 30% flexion strength occurred. Baker and Bierwagen noted an 86% decrease in supination endurance in patients treated conservatively. Surgical management varies highly in the treatment of distal biceps injuries, both in terms of approach and fixation methods. Prud'homme-Foster et al. demonstrated that, when compared with a one-incision approach, a two-incision approach allows for a more anatomic repair. In their cadaveric study, they demonstrated that forearms repaired anatomically via a two-incision approach demonstrated 15% more supination torque at neutral pronosupination and 40% more supination torque at 45 degrees of supination compared with tendons fixed nonanatomically via a one-incision approach.
Classification of distal biceps tendon ruptures is based on chronicity, degree of tear (partial vs. complete), and extent of retraction. The Ramsey classification uses these three characteristics to help guide treatment by predicting the ability to reattach the distal biceps tendon primarily to the radial tuberosity ( Box 62.1 ).
The mechanism of injury is nearly always a forceful, eccentric contraction of the biceps muscle. Examples of this mechanism include a preacher curl performed with excessive weight by a weight lifter and forcible extension of the elbow during an attempted tackle by a football player. The most common description and localization of initial pain is an abrupt, intense tearing sensation in the antecubital fossa. A palpable or audible “pop” is frequently recounted. Patients may report sudden and persistent weakness, especially with forearm supination and elbow flexion. As days pass and the swelling diminishes, the patient may notice a cosmetic deformity of the arm as the biceps retracts proximally. Many patients report the slow migration of skin discoloration from the hematoma within the elbow region toward the wrist over time. In patients with a partial biceps tear, the diagnosis is less clear. They may complain of a vague ache like discomfort within the antecubital region, which is exacerbated with forearm supination.
Inspection of the elbow will often reveal deformity and proximal retraction of the biceps (termed a “Popeye muscle”), swelling, and ecchymosis within the antecubital fossa and medial aspect of the forearm ( Fig. 62.4 ). Palpation elicits tenderness in the antecubital fossa and a defect of the tendon compared with the contralateral arm. In patients with an intact lacertus fibrosus, the deformity may be less pronounced. Weakness and pain with resisted forearm supination compared with the contralateral side is universally observed in complete ruptures.

Other physical examination tests specific for distal biceps tendon ruptures include the hook test and the biceps squeeze test. The hook test was originally described by O'Driscoll et al. and is performed by first placing the patient's arm at 90 degrees of flexion. Next, the examiner attempts to hook the lateral edge of the biceps tendon with the index finger by pulling from a lateral to medial direction within the antecubital fossa. A positive test elicits an intact cordlike distal biceps tendon. The test is reported to have 100% sensitivity and between 85% and 92% specificity. One needs to be sure that they are feeling for the distal biceps tendon, which occasionally may be tricky as they palpate an intact lacertus fibrosus. The biceps squeeze test is similar to the Thompson test for Achilles tendon ruptures. The examiner squeezes the biceps brachii muscle, and in patients with an intact distal tendon, the forearm should supinate. Pain with palpation over the posterolateral aspect of the radial tuberosity while pronating the forearm is suggestive of distal biceps tendinopathy.
A standard elbow radiographic trauma series (i.e., anteroposterior, lateral, and oblique views) should be obtained to evaluate for other causes of anterior elbow pain. Generally there are no signs of acute bony injury, but anterior soft tissue swelling may be appreciated. In rare cases an avulsion fracture of the radial tuberosity may occur and should be visible on radiographs.
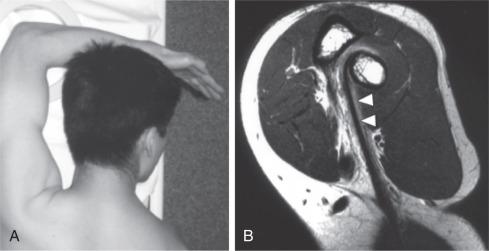
Magnetic resonance imaging (MRI) is an excellent modality for assessment of the integrity of the distal biceps tendon, but it is not always necessary to make or confirm the diagnosis. MRI is valuable for differentiating complete from partial tears in equivocal cases, such as in obese patients and persons with an intact lacertus fibrosus. Positioning the arm for an MRI with the elbow flexed, shoulder abducted, and the forearm supination, the so-called “FABS view,” allows for complete imaging of the distal biceps tendon, typically on a single image ( Fig. 62.5 ).
Nonoperative treatment may be considered especially for elderly, low demand individuals and those with partial tendon ruptures wishing to avoid surgery. The typical nonoperative protocol consists of a brief period of immobilization, analgesia, and physical therapy. The goals of physical therapy are the restoration of range of motion (ROM) with gradual elbow flexion and forearm supination strengthening. Patients who elect nonoperative treatment must be counseled on the risk of chronic activity-related pain, fatigue, loss of supination strength between 40% and 60%, and flexion strength of up to 30% and endurance. Patients also must be made aware that outcomes after delayed repair (>4 weeks) may be inferior to those obtained with acute repair and may require tendon grafting or be deemed irreparable.
Once the decision is made to treat a distal biceps tendon rupture surgically, several factors must be carefully taken into consideration prior to proceeding. These include patient factors such as occupation and function, history of anabolic steroids use, how much time has elapsed from the injury, how to expose of the radial tuberosity (one vs. two incisions) and how best fixate the tendon to bone. To date no single surgical plan has demonstrated clear superiority; operative treatment must be tailored to the individual patient and the proficiency of the surgeon.
Injury chronicity is perhaps the most important factor for the surgeon to consider. Early diagnosis may prevent tendon retraction permitting easier reattachment of the biceps tendon to the radial tuberosity regardless of the integrity of the lacertus fibrosus. In this regard, primary reattachment is generally reliable if performed within 4 weeks of the injury. An intact lacertus fibrosus may minimize tendon retraction and increase the window for reattachment beyond 4 weeks. Concurrent rupture of the lacertus fibrosus will lead to proximal retraction of the tendon and formation of scar tissue with attachment to the adjacent brachialis muscle. Delayed surgery often necessitates extensive scar dissection to liberate the coiled tendon and regain critical length for primary reattachment.
Primary repair may not be possible in persons with chronic injuries, and tendon autograft/allograft reconstruction may be offered to these patients as an alternative to nonoperative care. The most commonly used autografts are semitendinosus and fascia lata, whereas the standard allograft is the Achilles tendon. Delayed reconstruction with use of a tendon graft historically has a less predictable outcome than early anatomic repair of the native tendon. Improvements in strength and endurance are possible, but delayed reconstruction may be reserved for symptomatic patients with significant disability.
Nonanatomic repair or distal biceps tenodesis to the brachialis muscle was first proposed in an effort to decrease complications associated with anatomic reattachment. Several studies have evaluated the efficacy of nonanatomic repair and have found excellent return of flexion strength but, predictably, little or no improvement in forearm supination strength. With modern anatomic reattachment techniques, the complication rate has decreased and nonanatomic repair has largely fallen from favor. One exception is a patient with a chronic, irreparable tear who has a chief complaint of activity-related pain and cramping rather than weakness and loss of endurance.
Much debate exists as to whether to perform a one or two incision repair technique. The discussion focuses on the ability to anatomically reattach the biceps tendon to the footprint of the radial tuberosity and the complications associated with each approach. Originally the surgery was performed using a one-incision technique to expose the radial tuberosity through the antecubital fossa. Given the relatively high rate of nerve injury, Boyd and Anderson developed a two-incision technique to expose the footprint through an additional posterolateral approach. Attachment of the biceps tendon through the posterolateral approach permits a more anatomic reconstruction to the radial tuberosity and requires less extensive anterior exposure, theoretically decreasing the risk of iatrogenic nerve injury. Furthermore, Hasan et al. demonstrated that through a single incision approach, only 9.7% of the repair site was within the original footprint, compared with 73.4% for the double incision approach. Critics of this two-incision approach point to the unique risk of radioulnar synostosis. Failla et al. responded to this drawback by reporting a case series of four patients with radioulnar synostosis who were treated with a modification of the Boyd and Anderson procedure involving a muscle-splitting approach between the common extensor mass and the supinator. This modification allows exposure of the radial tuberosity without violating the ulnar periosteum and decreases the risk of radioulnar synostosis. A subsequent study revealed that the rate of radioulnar synostosis increases if the posterolateral incision is made over the subcutaneous border of the ulna rather than over the common extensors.
Four fixation techniques are presently being used to reattach the distal biceps tendon to the radial tuberosity: transosseous tunnels, suture anchors, interference screws, and cortical fixation buttons (or a combination thereof). Several biomechanical studies have compared fixation strength and stiffness between the different fixation techniques. In general, all fixation methods provide adequate fixation strength compared with the intact tendon, with the highest load to failure achieved using a cortical fixation button ( Table 62.1 ).
| Study | LOAD TO FAILURE (N) | ||||
|---|---|---|---|---|---|
| Intact Tendon | Transosseous Tunnel | Suture Anchor | Interference Screw | Cortical Fixation Button | |
| Berlet et al. | 307 (±142) | 220 (±54) | |||
| Lemos et al. | 203 | 263 | |||
| Idler et al. | 204 (±76) | 125 (±23) | 178 (±54) | ||
| Greenberg et al. | 177 | 584 | |||
| Mazzocca et al. | 310 | 381 | 232 | 440 | |
Acute operative fixation of the distal biceps may be offered to patients who require strength and endurance with elbow flexion and forearm supination. Nonoperative treatment of complete ruptures will yield between 12% and 40% loss of supination strength, up to 86% loss of supination endurance, and consistently decreased Disabilities of the Arm, Shoulder and Hand (DASH) and European Society of Surgery of the Shoulder and Elbow scores. Conversely, early anatomic reconstruction of the distal biceps can restore elbow flexion and supination strength and endurance and demonstrates higher clinical and functional outcomes. When considering nonoperative treatment, the practitioner needs to consider the patient's functional status and needs to inform patients of the sequelae should they proceed with this option.
Our preferred technique is a single-incision anatomic repair of the distal biceps tendon using a combination of both a fixation button and an interference screw. To perform this technique, a transverse incision is made anterior to the radial tuberosity with the arm in extension, usually 3 to 4 cm distal to the elbow flexion crease. An alternative approach is a longitudinal incision over the radial tuberosity, which is more extensile than a transverse approach. The antecubital veins are ligated or mobilized. The lateral antebrachial cutaneous nerve is identified lateral to the biceps course and carefully protected to avoid traction injury. To access the footprint of the radial tuberosity, the leash of radial recurrent artery is identified and ligated. At this point the ruptured tendon is either found locally (when the lacertus fibrosus is intact) or proximal blunt dissection is carried out if the tendon has retracted (i.e., when the lacertus fibrosus is torn). Along the original course of the tendon, large seromas are frequently discovered and evacuated. As the chronicity of the injury increases, a pseudosheath of fibrous scar tissue may mimic the actual tendon. Often this pseudosheath must be carefully débrided to unveil the native tendon end buried within this “cocoon.” Once retrieved, many surgeons will place a clamp (e.g., an Allis clamp) at the terminal tendon and manually release proximal adhesions or even “water ski” with the tendon to achieve maximal excursion. To aid in this, the tourniquet may need to be deflated as this may tether the biceps muscle. Using a heavy nonabsorbable suture (e.g., No. 2 FiberWire, Ticron, or Ethibond), a whipstitch is woven through the distal biceps tendon from proximal to distal, leaving two long limbs exiting the terminus.
The radial tuberosity is exposed with the elbow in full extension and maximal passive supination to protect the posterior interosseous nerve. A retractor may be placed by the radial aspect of the tuberosity, but care must be exercised to avoid excessive lateral retraction to prevent injury to the posterior interosseous nerve. A 3.2-mm guide pin is then drilled bicortically through the radial tuberosity. An acorn-shaped reamer is passed over the guide pin to create a unicortical tunnel. The suture limbs are passed through a fixation button, and the button is passed bicortically through the radial tuberosity. The tendon is advanced approximately 1 cm into the tunnel and the sutures are tied, securing the biceps tendon within the radial tuberosity ( Fig. 62.6 ). An interference screw is placed into the tunnel, displacing the tendon more distally and ulnar to better recreate the anatomic insertion site.

Rehabilitation protocols vary depending on the surgical technique and patient compliance. Early in the postoperative course, a period of immobilization or protective splinting is typical. Gentle passive ROM is permissible within the first few weeks. Some surgeons use a hinged brace to block terminal elbow extension initially, which is meant to protect the healing tendon from high tensile forces. After 3 weeks, patients may begin active assisted ROM, and full active motion is usually achieved 6 to 8 weeks after surgery. Resistive exercises are restricted until 8 weeks after surgery, at which time a gradual approach to biceps strengthening exercises is prudent to avoid a repeat tendon rupture. Although many patients prefer a home exercise regimen, it may be wise to refer noncompliant patients to a physical or occupational therapist for guidance and supervision during this phase. Most patients recover ROM and desired strength between 3 and 6 months after surgery.
Cheung et al. evaluated early self-administered passive ROM exercises. After surgery, a hinged elbow brace locked at 90 degrees of flexion was immediately applied. On the first postoperative day, the brace was unlocked to allow passive ROM exercises from 60 degrees to full flexion with full forearm rotation. The elbow extension block was reduced at 2 weeks to 40 degrees, at 4 weeks to 20 degrees, and at 6 weeks to full extension. Strength training was begun at 8 weeks. With this protocol of immediate elbow motion following distal biceps tendon reattachment, no deleterious effects on healing or strength were observed.
Return to sport after distal biceps tendon rupture has not been specifically studied. The general consensus is that patients may return to unrestricted activities at 16 to 20 weeks after surgery. Athletes who participate in contact sports, such as football and rugby players, may need the full 20 weeks to permit tendon maturation and to prevent a repeat rupture.
Several studies have evaluated the outcome of one- and two-incision distal biceps tendon repairs. Both techniques improve DASH scores and elbow flexion and forearm supination strength.
Karunakar et al. reported on 21 patients after use of the modified Boyd and Anderson technique with bone tunnels. At 44 months all patients reported good to excellent results. Compared with the uninjured arm, endurance was decreased 38% in supination and 33% in flexion. A 15% rate of heterotopic ossification was noted.
McKee et al. compared one-incision repairs with two suture anchors, using the uninjured arm as a control. At final follow-up, no difference was found in DASH scores. Strength was 96% in flexion and 93% in supination compared with the uninjured side. No differences in ROM were observed.
In a study evaluating outcomes after EndoButton (Smith and Nephew, Andover, MA) fixation, Peeters et al. reported an average Mayo Elbow Performance Score of 94 points. Isokinetic testing showed 80% recovery of flexion strength and 91% recovery for supination. Of 26 patients, 2 experienced asymptomatic heterotopic ossification, and three had asymptomatic disengagement of the EndoButton.
Grewal et al. performed a direct comparison between one-incision repairs using suture anchors and the modified Boyd and Anderson approach using bone tunnels. They found no difference in patient reported outcomes for pain and function at 2 years postoperatively. The one-incision cohort had greater improvement in flexion (142.8 vs. 131.1 degrees) but an overall higher complication rate, with the majority of complications being lateral antebrachial cutaneous nerve palsies. Similarly, Shields et al. found a higher incidence of lateral antebrachial cutaneous neuropraxia following one-incision repairs, but found no difference in strength or ROM and equivalent patient reported outcomes. Schmidt et al. investigated factors that determine strength after distal biceps reattachment and found a two-incision approach to better restore strength than a one-incision approach with no ultimate differences in forearm motion between groups.
Several fixation techniques may be used to affix the tendon to the radial tuberosity. Fixation techniques and respective load to failure are reviewed in Box 62.2 . Techniques that increase the load to failure may allow earlier rehabilitation after surgery.
Football
Weight lifting
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here