Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tricuspid regurgitation (TR) is most frequently functional, not related to primary tricuspid leaflet pathology but secondary to another disease process that produces right ventricular dilation, distortion of the subvalvular apparatus, tricuspid annular dilation, or a combination of these.
Severe TR due to a flail leaflet is associated with adverse outcomes favoring early surgical repair.
TR negatively impacts clinical outcome and survival, regardless of left ventricular ejection fraction or severity of pulmonary hypertension.
Tricuspid valve repair is the preferred treatment for TR in the absence of severely dysplastic or damaged leaflets.
When tricuspid valve replacement is required, bioprosthetic valves are usually preferred over mechanical valves, although long-term mortality rates are similar for both.
Transcatheter tricuspid valve interventions are an emerging therapy for patients with functional TR.
Tricuspid stenosis occurs infrequently and is rarely seen in isolation.
Differentiation of primary valve abnormalities from valve dysfunction that is secondary to pulmonary hypertension or primary right-sided heart disease is an important first step in the evaluation and management of tricuspid valve disease. Primary tricuspid disease may be caused by rheumatic or carcinoid heart disease, tricuspid valve prolapse, endocarditis, trauma, or congenital heart disease. Tricuspid regurgitation (TR) is most frequently secondary or functional, occurring as a consequence of tricuspid annular dilation and right ventricular (RV) remodeling due to right-sided chronic pressure or volume overload.
Changes in RV structure and function occur in response to pressure and volume overload and the extent of RV remodeling. Chronic volume overload results from TR and causes RV enlargement, primarily in the radial rather than the longitudinal direction, , which can lead to further tricuspid annular dilation and worsening TR. RV systolic function occurs earlier in the disease course than is typical for left-sided volume overload conditions. , However, as with left-sided valve disease, RV volume and systolic function are expected to improve after intervention for primary valvular disease unless an irreversible decline in contractility has occurred.
RV volume overload is also associated with abnormal or paradoxical ventricular septal motion; the septum moves toward the center of the RV in systole and moves rapidly posteriorly in diastole—a pattern opposite of normal. In these patients, the reversed curvature of the septum is most marked in end-diastole. In contrast, in patients with pressure overload, the maximum reversed curvature is more evident and occurs early in diastole.
The response of the RV to chronic pressure overload (e.g., from pulmonary hypertension or pulmonary stenosis) differs from that of the left ventricle (LV). Although the initial response is an increase in wall thickness, ventricular dilation may occur, depending on the acuteness and severity of the pressure overload. If there is a gradual increase in RV pressure, RV size and systolic function may remain normal with a compensatory increase in RV wall thickness. After intervention to relieve pressure overload, an improvement in RV systolic function may occur as a result of the decreased RV afterload. RV dimensions and systolic function improve in most patients after lung transplantation, supporting the concept that systolic function improves with decreased afterload. ,
With an acute increase in RV pressure, such as with acute pulmonary embolism, decreased RV systolic function and clinical right heart failure may be seen, with mean pulmonary pressures of only 20 to 40 mmHg. Acute or subacute RV pressure overload often results in RV dilation with secondary annular dilation and TR. This superimposes a volume overload state, engendering a vicious cycle of RV dilation and worsening TR.
After a thorough history and physical examination, echocardiography remains the cornerstone of diagnosis of tricuspid valve disease. The same principles as for evaluation for other valves are followed to confirm the presence and severity of valvular stenosis and regurgitation. Correct diagnosis of the mechanism of tricuspid stenosis (TS) or TR and assessment of the extent of RV modeling are critical to determine the most appropriate treatment strategy. Specific echocardiographic assessment of TR and TS is described later.
The American Heart Association (AHA)/American College of Cardiology (ACC) guidelines and the European Society of Cardiology (ESC) valvular heart disease guidelines recommend staging of valve lesions to define progression and severity of valvular heart disease. Stage A represents patients at risk for valve dysfunction; stage B represents those with progressive valve disease; and stages C (asymptomatic) and D (symptomatic) represent those with severe valve dysfunction ( Tables 23.1 and 23.2 ).
| Structural Abnormality | Valve Hemodynamics | Hemodynamic Consequences | Symptoms |
|---|---|---|---|
| Stage A: At Risk | |||
| Primary Mild structural abnormality (e.g., rheumatic or prolapse) Functional (secondary) None or mild annular dilation |
None or trivial | Normal right-sided chambers and filling pressures | None due to TR |
| Stage B: Progressive | |||
| Primary Progressive structural abnormality (e.g., moderate-severe prolapse) Functional (secondary) Mild annular dilation, moderate leaflet tethering |
Mild Jet area < 5 cm 2 Parabolic CW contour Moderate Jet area < 5–10 cm 2 VC < 0.7 cm Dense CW jet, varied contour Blunted systolic hepatic vein flow |
Mild Normal right sided chambers Moderate Normal RV size Normal–mild RA enlargement Normal–mild IVC dilation, normal RA pressure |
None due to TR |
| Stage C: Asymptomatic Severe TR | |||
| Primary Flail or severely damaged leaflets Functional (secondary) Severe annular dilation |
Jet area > 10 cm 2 VC > 0.7 cm Dense CW jet, early-peaking dagger-shaped contour Systolic hepatic vein flow reversal |
Dilated RV/RA/IVC ↑RA pressure V-wave on examination Diastolic septal flattening |
None due to TR |
| Stage D: Symptomatic Severe TR | |||
| Primary Flail or severely damaged leaflets Functional (secondary) Severe annular dilation (>40 mm or >21 mm/m 2 ), severely tethered leaflets |
Jet area > 10 cm 2 VC > 0.7 cm Dense CW jet, early peaking dagger shaped contour Systolic hepatic vein flow reversal |
Dilated RV/RA/IVC ↑RA pressure V-wave on examination Diastolic septal flattening Decreased RV systolic function |
Right heart failure Fatigue Ascites Abdominal discomfort Dyspnea Anorexia Edema |
Trivial or mild TR, which may be incidentally identified by transthoracic echocardiography (TTE) obtained for other purposes, is a common physiologic finding in patients with structurally normal tricuspid valves. In contrast, patients with structural tricuspid valve abnormalities are at risk for progressive valve disease and even those with trivial TR should be staged and monitored for symptoms and severity of valve disease, including extent of RV remodeling. Whereas there are guideline recommendations for all stages of TR, only stage C and D criteria are described for TS (see Table 23.2 ).
| Stage | Structural Abnormality | TS Severity | Consequences | Symptoms |
|---|---|---|---|---|
| C and D: severe TS | Thickened, distorted, or calcified leaflets | PHT ≥ 190 ms Valve area ≤ 1.0 cm 2 Gradient > 5–10 mmHg at HR of 70 beats/min a |
Dilated RA/IVC | Asymptomatic or right heart failure, affected by associated valve disease severity: Fatigue Hepatic congestion Abdominal discomfort Dyspnea Edema |
a Tricuspid valve gradients vary and are affected by cardiac output, heart rate, and respiratory phases.
Advanced RV dysfunction resulting in worsening heart failure is associated with increased mortality rates after tricuspid valve surgery. Although echocardiography can provide morphologic assessment of RV dimensions and function, accurate measurements are difficult because of the complex three-dimensional (3D) anatomy of the RV. , 3D echocardiographic imaging improves estimation of RV volumes over two-dimensional (2D) imaging, but cardiac magnetic resonance (CMR) imaging is more accurate and reproducible. However, assessment of RV function by CMR is less accurate than assessment of the LV.
Tricuspid annular plane systolic excursion using M-mode echocardiography is a simple and reproducible measurement of RV longitudinal function that correlates well with other echocardiographic measures of RV function, including RV ejection fraction, but it may be less accurate in special populations such as those with congenital heart disease. ,
Other measures of RV function, including the right-sided index of myocardial performance (Tei index) and measurements of peak systolic velocity and displacement of the tricuspid annulus using tissue Doppler imaging, are feasible and have prognostic value for patients with pulmonary hypertension and other pathologies. , RV longitudinal strain, as measured by echocardiography, can be used to evaluate global and regional RV contractility; reduced longitudinal strain predicts disease progression in pulmonary arterial hypertension. , ,
The extent of RV hypertrophy can be assessed qualitatively based on the thickness of the RV free wall. , Timing of ventricular septal motion also provides insight into RV function (discussed earlier) but is often better appreciated by M-mode rather than 2D echocardiography. In cases of RV enlargement, careful assessment of the atrial septum and pulmonary veins is critical to exclude a left-to-right shunt. Transesophageal echocardiography (TEE) should be performed if uncertainty remains after TTE imaging.
Estimation of pulmonary pressures is an essential component of the examination of patients with right-sided valve disease. RV pressures can be estimated noninvasively from the velocity of the tricuspid regurgitant jet (V TR ) and the appearance of the inferior vena cava. Most patients have some degree of TR that permits estimation of the right ventricular-to-atrial pressure gradient (ΔP RV−RA ), as described in the simplified Bernoulli equation:
where ΔP = change in pressure; RA = right atrium; RV = right ventricle; TR = tricuspid regurgitation; and V = velocity.
This Doppler-derived pressure gradient is added to an estimate of right atrial pressure based on the size and respiratory variation of the inferior vena cava caliber. However, in severe, wide-open TR, in which the right ventricular-to-atrial pressure gradient may be reduced by equilibration of pressures between the chambers, RV systolic pressure may be underestimated by echocardiography.
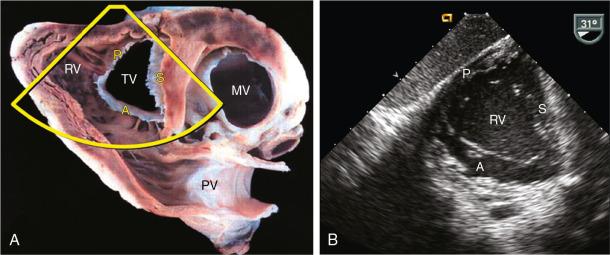
The normal tricuspid valve is characterized by three sail-like leaflets: anterior, posterior, and septal ( Fig. 23.1 ). The anterior leaflet is the largest and most anatomically constant of the three; the posterior and septal leaflets are smaller and vary more in size and position. The number of tricuspid valve papillary muscles varies. The larger anterior papillary muscle is most consistently present and supplies chordae to the anterior and posterior leaflets. A septal papillary muscle is absent in up to 20% of normal subjects, , and the septal leaflet may insert directly into the RV free wall, typically more apically (≤10 mm) than the septal portion of the anterior mitral valve leaflet. , , It is the least mobile of the three leaflets and has the most support from the fibrous trigone.
The normal tricuspid annulus is elliptical and nonplanar or saddle-shaped. It is longer in the septal-to-lateral dimension (from the aortic valve to the lateral free wall) than in the anterior-to-posterior dimension, with high points at the anteroseptal aspect (adjacent to the aortic valve and RV outflow tract) and the posterolateral aspect (adjacent to the free wall) and low points at the posteroseptal and anterolateral aspects , ( Figs. 23.2 and 23.3 ). The septal part of the tricuspid annulus includes the fibrous trigone, and as the RV dilates, the tricuspid annulus enlarges primarily outward along the free wall of the RV laterally, adjacent to the anterior and posterior leaflets. , , It becomes more circular and flattens, affecting coaptation of the anterior and posterior leaflets. , ,
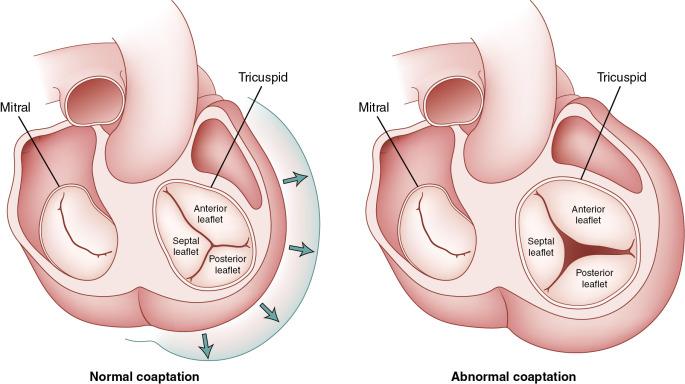
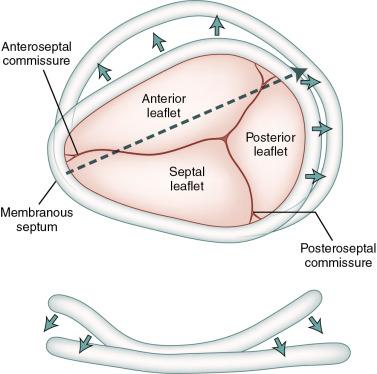
Recommendations for surgical intervention for severe functional TR are based on the severity of tricuspid annular dilation (see Table 23.1 ). The AHA/ACC and ESC valvular heart disease guidelines define severe tricuspid annular dilation (stage C or D) as a tricuspid annulus of at least 40 mm or greater than 21 mm/m 2 . However, tricuspid annular size varies among normal individuals throughout the cardiac cycle and with different echocardiographic views.
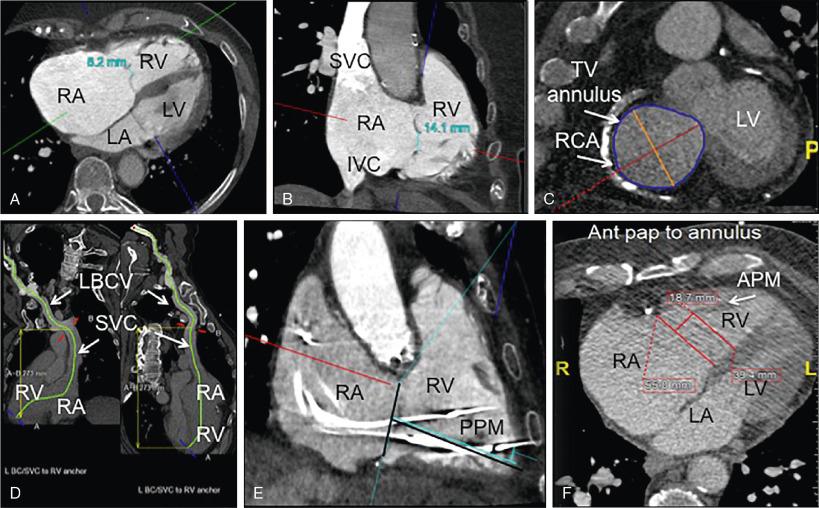
Consistent measurement of the tricuspid annulus is critical for making decisions about surgical and transcatheter interventions. The tricuspid annulus is typically measured from its mid-septal to mid-anterior points in the apical four-chamber view in early diastole, when the annulus size is largest. , Whereas 2D TTE is the most widely used technique to assess tricuspid annular size, cardiac computed tomography (CT) and CMR can also demonstrate proximity to surrounding structures for planning of surgical and transcatheter procedures and may provide precise annular measurements when 2D echocardiographic images are technically difficult or not feasible , , ( Fig. 23.4 ).
The three tricuspid valve leaflets can rarely be seen simultaneously by standard 2D TTE; this usually requires angling through different views: parasternal long-axis of the RV inflow, short-axis at the aortic valve level, apical four-chamber, and subcostal windows. Typically, only two leaflets can be imaged in one view, and the anterior leaflet is the one most consistently visualized by echocardiography.
In the apical four-chamber view, the anterior leaflet is adjacent to the RV free wall, and the septal leaflet is opposite and adjacent to the septum. In the parasternal RV inflow view, the anterior leaflet is visualized in the near field, but the opposite leaflet may be the septal or the posterior leaflet. Accurate identification of the three leaflets can be difficult unless a short-axis image of the tricuspid valve can be obtained from a modified subcostal view or from a transgastric view by TEE. , Real-time 3D echocardiography may be required to correctly and consistently identify all three tricuspid valve leaflets, , and cardiac CT or CMR may be useful, particularly in patients with congenital heart disease such as Ebstein anomaly. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here