Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
It is important to know multiple ways to identify the facial nerve during parotidectomy.
Differentiate between infectious, inflammatory, granulomatous, autoimmune, and neoplastic processes based on history, physical examination, laboratory tests, and radiographic imaging.
Know the prevalence and malignancy rates of neoplasms in each major salivary gland.
Mumps and Staphylococcus aureus are the most common causes of viral and acute suppurative sialadenitis, respectively.
The most common benign salivary gland tumors are pleomorphic adenomas in adults and hemangiomas in children.
The most common malignant salivary gland tumor in the parotid is mucoepidermoid carcinoma.
HIV workup is important in a patient who presents with cystic parotid masses.
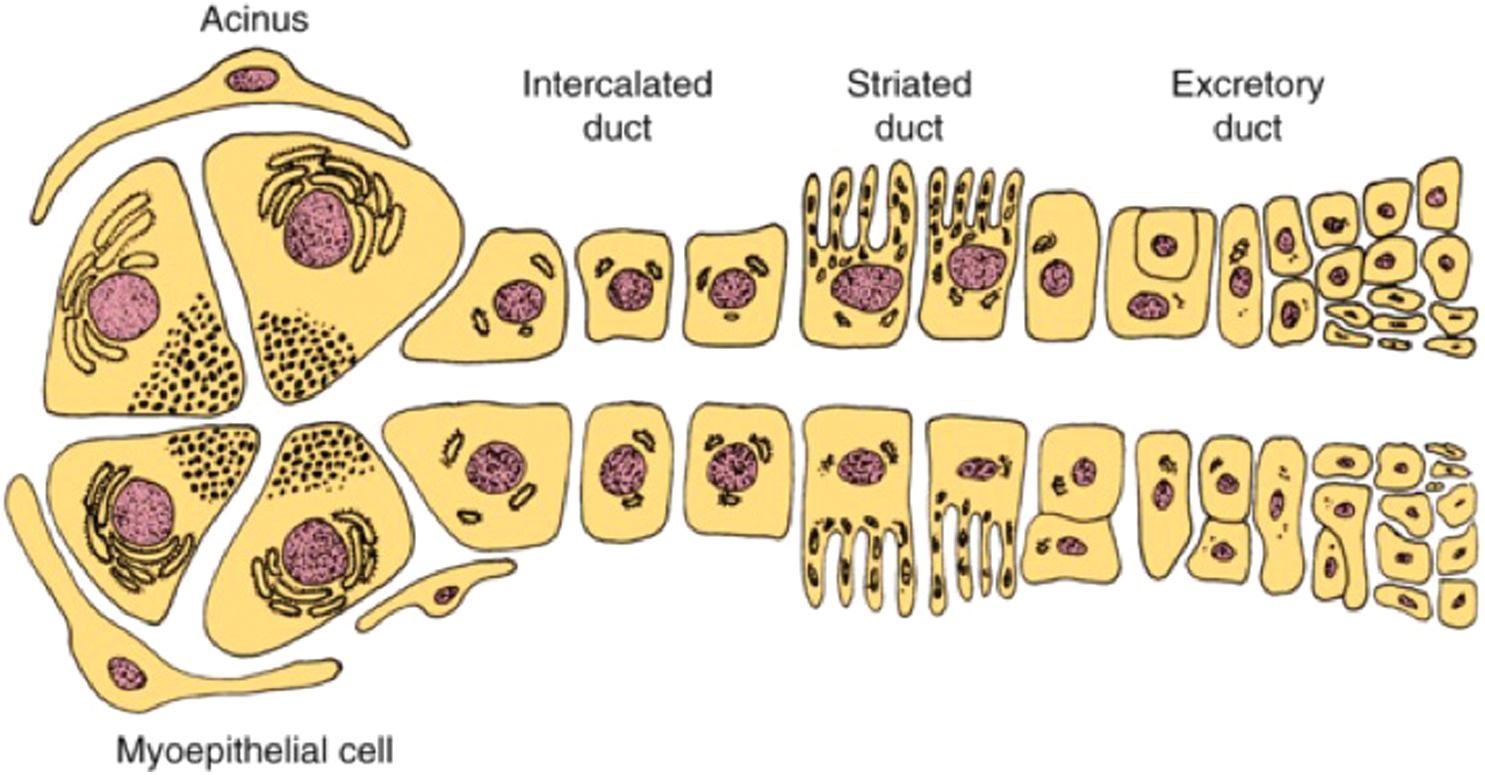
From proximal to distal: Acinar cells –> intercalated duct –> striated duct –> excretory duct. Contractile myoepithelial cells surround the acini and intercalated ducts ( Fig. 15.1 ).
Approximately 1500 mL of saliva is produced daily. At rest, the submandibular glands are the most active (producing two-thirds of all saliva). When stimulated by nausea, food, olfaction, or mastication, the parotid glands become the most active.
The parotid gland ( Fig. 15.2 ) is located in the lateral face (parotid space), bordered by the masseter muscle anteriorly/medially, the zygomatic arch superiorly, the tragal cartilage posteriorly, the angle/ramus of the mandible posteriorly/medially, and the sternocleidomastoid muscle (SCM) inferiorly. It is enveloped by the parotidomasseteric fascia, a continuation of the superficial layer of the deep cervical fascia.
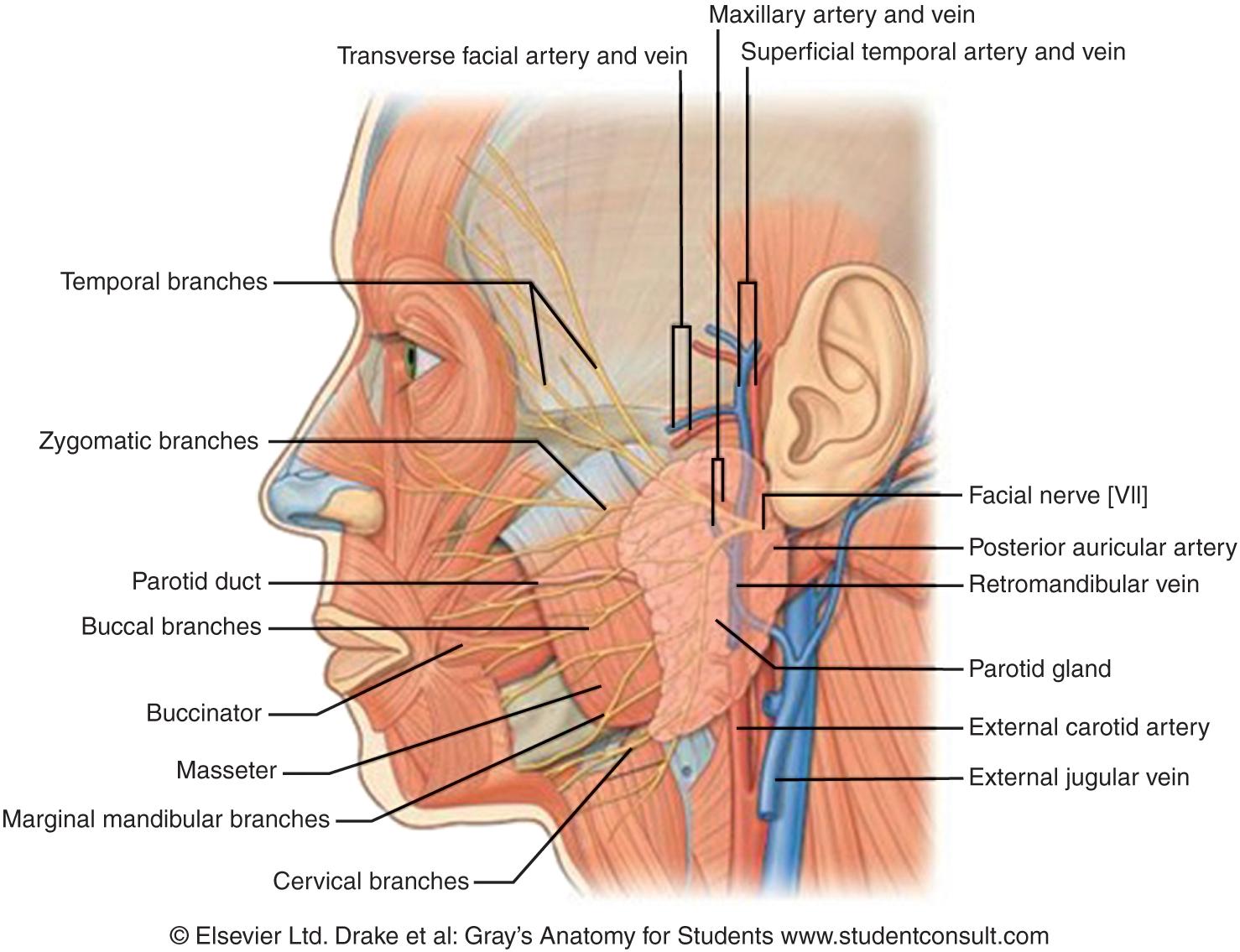
The external carotid artery lies medial to the parotid and branches into the maxillary and superficial temporal arteries. Venous anatomy is variable: the maxillary and superficial temporal veins form the retromandibular vein and join the external jugular vein.
Parasympathetic innervation: inferior salivatory nucleus –> glossopharyngeal nerve (CN IX) –> Jacobson’s nerve –> lesser petrosal nerve –> otic ganglion –> auriculotemporal nerve.
Stensen’s duct travels superficial to the masseter, pierces the buccinator muscle, and enters the oral cavity opposite the second maxillary molar. The duct is approximately 1.5 centimeters inferior to the zygoma.
The facial nerve separates the parotid into superficial and deep lobes (not a true fascial plane). The retromandibular vein is a surrogate radiographic landmark for the facial nerve.
The submandibular gland ( Fig. 15.3 ) is inferior and deep to the mandible in the submandibular triangle (defined by the anterior and posterior bellies of the digastric muscle and the mandibular body). The mylohyoid muscle divides the gland into superficial and deep lobes. In the surgical field from the neck, retraction of the mylohyoid muscle reveals the lingual nerve, Wharton’s duct (submandibular duct), and hypoglossal nerve lying superficial to the hyoglossus muscle.
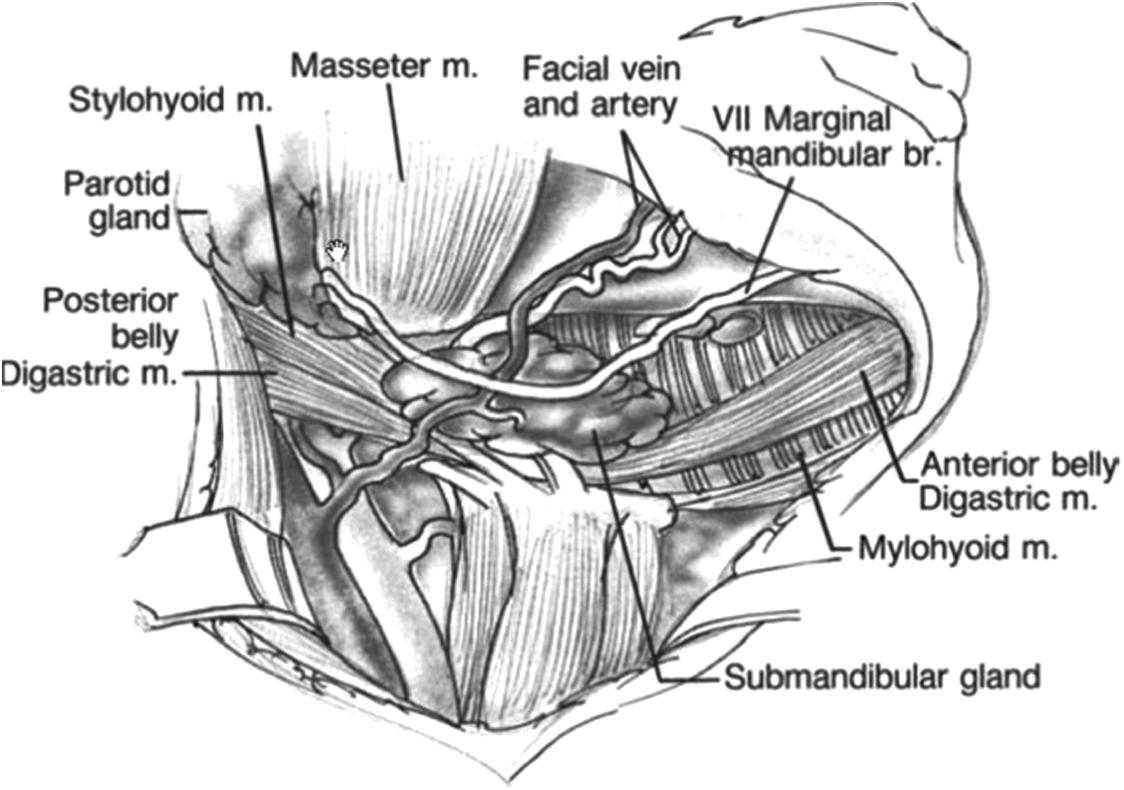
The facial artery travels obliquely and deep to the posterior belly of the digastric muscle along the posterior surface of the submandibular gland. The facial artery curves over the mandible body at the superior aspect of the gland. The facial vein travels anterior to the gland.
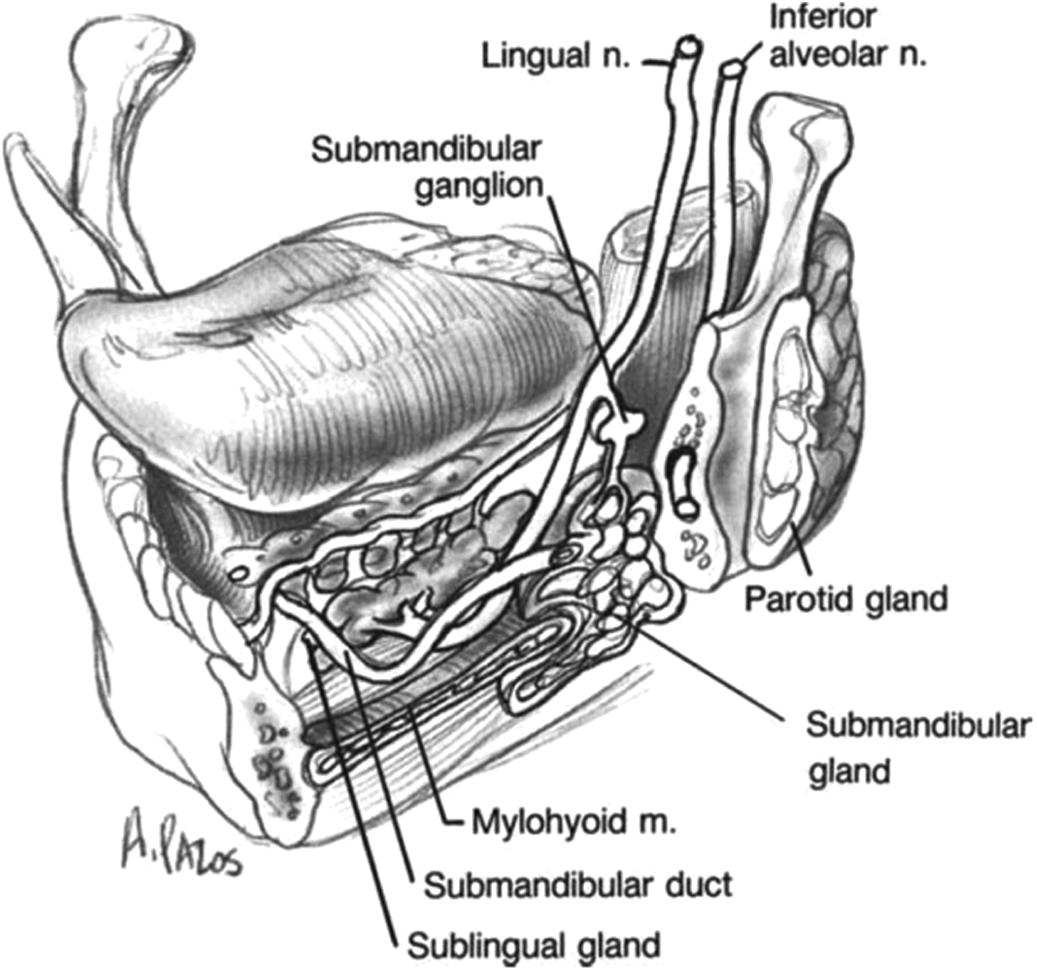
Parasympathetic innervation: superior salivatory nucleus –> nervus intermedius –> chorda tympani –> submandibular ganglion –> lingual nerve.
The sublingual gland ( Fig. 15.4 ) is located adjacent to the lingual frenulum, lateral to the genioglossus and geniohyoid muscles, and superficial to the mylohyoid muscle. The blood supply is from the branches of the facial and lingual arteries. Parasympathetic innervation is the same as for the submandibular gland. The sublingual gland drains into the oral cavity through the ducts of Rivinus or into Wharton’s duct via the Bartholin duct.
Staphylococcus aureus is the most common bacteria that causes sialadenitis. Treatment consists of antibiotics effective against β-lactamase-producing bacteria (i.e., amoxicillin-clavulanate) or culture-directed antibiotics plus hydration, warm compresses, gland massage, and sialagogues.
The submandibular gland is most affected by sialolithiasis due to the more viscous/mucinous saliva that travels superiorly against gravity in Wharton’s duct. Treatment options include the following:
Conservative management with sialagogues, warm compresses, antibiotics, massage, and hydration
Open sialolithotomy
Sialendoscopy (<6 millimeter sialoliths)
Lithotripsy
Excision of salivary gland
Mumps is still the most common cause of viral parotitis, although most infections have been eliminated by vaccination.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here