Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
More than 200 primary lesions or diseases occur in the oral mucosa, gingiva, teeth, jaws, and minor or major salivary glands. In addition, secondary abnormalities of the oral mucosa or salivary glands can be caused by systemic diseases or drugs. The most common or important of these diseases may be observed during physical examination.
Painful, short-lasting ulcerations can be caused by mechanical trauma, immunologic mechanisms, or bacterial or viral infections ( Table 393-1 ). Soon after formation, oral mucosal ulcers become covered by a white to gray pseudomembrane, analogous to the yellow scabs on dry skin. Pseudomembrane-covered ulcers are distinguished from white hyperkeratotic lesions by their clinical features: pseudomembranes are removeable and painful, and they have a flat surface with an erythematous periphery. Traumatic ulcers are characteristically located on the tongue or inside the cheeks or lips close to the chewing surfaces of the teeth.
| TYPE/DISEASE | CLINICAL FEATURES |
|---|---|
| INSIDIOUS ONSET, CHRONIC | |
| Multiple or Bilateral | Shallow ulcers on mucosa, skin, or both |
| Pemphigus vulgaris | Begin as fragile, short-duration blisters |
| Mucous membrane pemphigoid | Begin as short-duration blisters |
| Lichen planus | Bilaterally symmetrical lesions (white lacelike with or without erythema) |
| Lupus erythematosus | Asymmetrical lesions, with or without systemic lupus (white with or without erythema) |
| Lichenoid drug reaction | Variable lesions; often unilateral; history of medication use |
| Epidermolysis bullosa | Begin as blisters; lifelong history |
| Solitary | Indurated or cratered ulcers |
| Squamous cell carcinoma | Most common on tongue, oropharynx, lip, mouth floor |
| Adenocarcinomas, various | Salivary tumors most common; on palate, cheeks, mouth floor |
| Tuberculosis | Usually painful |
| Actinomycosis | Often associated with draining sinus tract |
| Deep mycoses (particularly histoplasmosis, coccidioidomycosis) | Associated with systemic infection; can resemble carcinoma clinically |
| Midline (lethal) granuloma | Associated with necrosis, may perforate palate; usually an NK/T-cell lymphoma or granulomatosis with polyangiitis |
| Bony osteonecrosis | Associated with prior cancer, radiation therapy or bisphosphonate/antiresorptive agent use |
| ACUTE ONSET, OFTEN SELF-LIMITING | |
| Clusters | Usually small and shallow ulcers; history of blisters |
| Primary herpes simplex | Any oral mucosal site, associated with fever, malaise; often widespread |
| Recurrent herpes simplex | Unilateral, only on keratinized mucosa (gingiva, hard palate, or lip) |
| Varicella-zoster | Unilateral lesions along neural distribution |
| Herpangina | Usually bilateral on soft palate |
| Measles (rubeola) | Precede skin rash; associated with fever, malaise |
| Solitary or Multiple (without Clustering) | Variable, usually without history of blisters |
| Traumatic ulcers | Usually solitary; history of trauma |
| Aphthous stomatitis (canker sores) | Circular, often multiple, shallow, only on nonkeratinized mucosa |
| Behçet syndrome | Oral lesions similar to recurrent aphthae |
| Erythema multiforme | Multiple lesions, often involve lower labial mucosa with hemorrhagic crust |
| Drug reaction | Appropriate history of drug use |
| Necrotizing sialometaplasia | Deep ulcers, usually on palate; can be associated with trauma |
| Primary syphilis | Solitary, indurated, painless, any site |
| Gonorrhea | Painful, surrounded by erythema, usually in oropharynx |
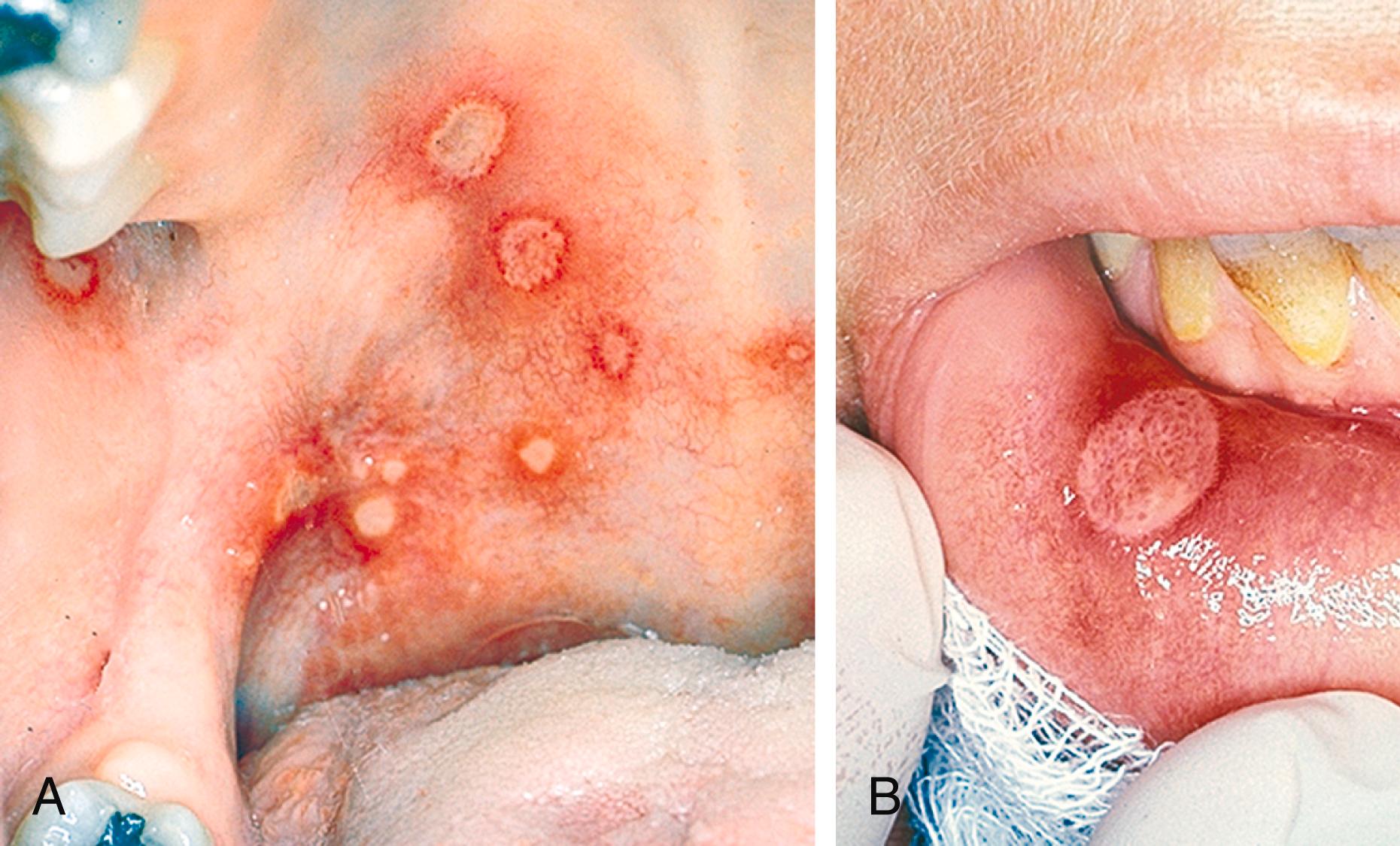
These idiopathic recurrent ulcers are common, afflicting up to 20% of the population and can be found on nonkeratinized mucosa: the buccal mucosa, ventral tongue, lips, and alveolar mucosa ( Fig. 393-1 ). They form well-defined, usually shallow, circular ulcers that may be single or multiple. There are three clinical forms: (1) minor, which are flat and less than 0.5 cm in diameter and last 5 to 10 days; (2) major, which have raised borders, are deeper, solitary, greater than 0.5 cm, and often last for weeks or months; and (3) herpetiform, which are usually clusters of very small ulcers that resemble recurrent herpetic lesions but are not preceded by vesicles and do not occur on keratinized mucosa. A viral or bacterial pathogenesis has not been established for any of these forms. Lesions clinically indistinguishable from minor aphthae occur in Behçet syndrome ( Chapter 249 ). Aphthae are rarely associated with anemias or gluten-sensitive enteropathy ( Chapter 126 ) and may become more frequent and severe in association with human immunodeficiency virus (HIV) infection ( Table 393-2 ).
| Kaposi sarcoma (human herpesvirus type 8) |
| Candidiasis (pseudomembranous, hyperplastic, and/or erythematous lesions) |
| Other opportunistic fungal infections (e.g., histoplasmosis or coccidioidomycosis) |
| Aphthous ulcers (increased frequency, duration, or size) |
Virus-associated epithelial hyperplasias
|
| Herpes zoster (varicella-zoster virus) |
| Exaggerated forms of gingivitis and inflammatory periodontal disease |
| Decreased salivary gland function |
| Parotid gland enlargement (lymphoepithelial lesion) |
| Non-Hodgkin lymphoma (e.g., plasmablastic lymphoma) |
Minor or herpetiform aphthous ulcers are generally self-limiting within a week or two and may not require treatment unless they occur frequently. Topical steroids, such as fluocinonide gel or ointment, can reduce the severity and duration of the lesions only if applied with prodromal symptoms or earliest signs. A freshly prepared suspension of tetracycline or doxycycline in water used as a mouth rinse at the onset of symptoms also reduces the severity and duration of disease. Unfortunately, none of these treatments prevent recurrent ulcers. Major aphthae usually require treatment with prednisone (e.g., 40 mg daily for 3 days); failure to respond significantly should prompt incisional biopsy to exclude neoplasia. Unfortunately, no treatment will cure a patient of recurrent aphthous stomatitis. Laser therapy may promote healing and pain relief in patients with recurrent aphthous stomatitis, although this approach has not been proven in clinical trials.
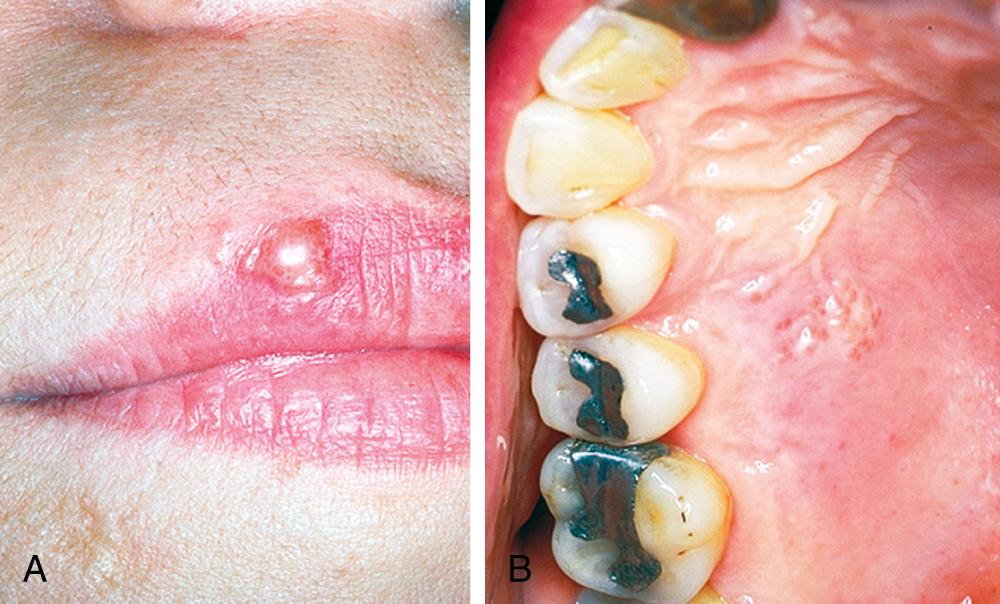
Several types of virus (most commonly herpes simplex type 1; Chapter 345 ) cause multiple oral mucosal vesicles that last only a few hours or days and then become irregular shallow ulcers. In the initial infection by herpes simplex virus, usually in children, numerous vesicles may appear on any oral mucosal site (called primary herpetic gingivostomatitis), accompanied by malaise, headache, fever, and cervical lymphadenopathy. Patients previously exposed to this virus may develop recurrent (secondary) lesions that appear as clusters of small vesicles, most commonly on the lips (herpes labialis) and less commonly on the keratinized mucosa of the gingiva or hard palate ( Fig. 393-2 ). Such lesions contain live virus and tend to recur at the same site but less frequently with increasing age.
Although widespread vaccination has reduced the incidence, similar mucosal vesicles may also accompany the initial infection by the varicella-zoster virus in children with chickenpox ( Chapter 346 ), and unilateral lesions may occur if herpes zoster ( Chapter 346 ) affects branches of the trigeminal nerve. Uncommonly, oral mucosal ulcers may be caused by different types of coxsackievirus ( Chapter 349 ), appearing on any oral site in hand-foot-and-mouth disease or on the soft palate or pharynx in herpangina. After infection by the measles (rubeola) virus, small ulcers (Koplik spots; see Fig. 338-2 in Chapter 338 ) may form on the inside of the cheeks 1 to 2 days before development of the skin rash ( Chapter 338 ). Patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection ( Chapter 336 ) may have a variety of oral manifestations, including erosions, ulcers, bullae, vesicles, and pustules.
Patients who receive radiation therapy for cancers where the radiation fields include the oral cavity are at risk for the development of oral mucositis ( Chapters 18 and 176 ). Oral mucositis is also common in patients who receive intensive chemotherapy for malignancies, such as patients who have leukemia ( Chapter 167, Chapter 170 ) or undergo hematopoietic stem cell transplantation ( Chapter 163 ). Oral mucositis also occurs in about 20 to 40% of patients treated with chemotherapy for other solid tumors. Risk factors include smoking, poor oral hygiene, a lower pretreatment neutrophil count, and the depth of treatment-induced neutropenia. Agents with higher risks include anti-angiogenic tyrosine kinase inhibitors (e.g., axitinib, cabozantinib, pazopanib, sorafenib, and sunitinib) and mammalian target of rapamycin (mTOR) inhibitors (e.g., everolimus), as well as etoposide, fluorouracil, and methotrexate. The pathobiology is cytotoxic damage to rapidly dividing cells, predominantly basal cells of the mucosal epithelium, by chemotherapy and radiation.
Patients can develop pain and sensitivity to irritating substances, which can be avoided by the patient. Mild mucositis may be difficult to confirm on examination, but oral ulceration is the hallmark of the condition. Bleeding occurs with more severe mucositis. A complete blood count with differential is helpful, and the patient should also be assessed for any signs of dehydration ( Chapter 7 ).
For patients with mild symptoms, a bland mouthrinse (e.g., normal saline or sodium bicarbonate in water) as a “swish and spit” can be symptomatically helpful. For moderate pain that does not interfere with oral intake, patients should avoid hard-consistency, rough, or sharp foods; alcohol; and smoking. A 2% oral lidocaine solution can be added to a normal saline or sodium bicarbonate mouthrinse. For more severe mucositis, topical agents include a doxepin mouthrinse and “Magic” mouthwashes. For more severe pain that interferes with eating, dehydration, neutropenia, or suspected systemic infection, expert consultation and typically hospitalization must be considered. For radiation-induced mucositis, a diphenhydramine/lidocaine/antacid mouthwash can reduce the incidence and severity of mucositis, and dexamethasone mouthwash can provide analogous benefits for patients receiving mTOR inhibitors.
In this potentially recurrent disease, painful oral mucosal ulcerations develop rapidly, with or without target-like skin lesions. It may be associated with a previous viral infection or hypersensitivity to a food or drug. The affected patients, usually young adults with minimal or no systemic symptoms, have irregularly shaped ulcers that can be small and few or involve large areas of the mucosa; the most common sites are the lower labial mucosa and vermilion. On the vermilion of the lips, bilateral hemorrhagic crusting is a characteristic finding. These lesions can be distinguished from those of primary herpes by the absence of oral vesicles and systemic symptoms or by the presence of characteristic skin lesions ( Chapter 406 ). A major variant of this disease is Stevens-Johnson syndrome, in which ocular, genital, and other lesions may accompany the oral lesions.
Primary syphilis may arise as a solitary, indurated, painless ulcer on the oral mucosa that resolves spontaneously in 4 to 6 weeks ( Chapter 295 ). Uncommonly, Neisseria gonorrhoeae ( Chapter 275 ) may cause oral ulcers, usually in the soft palate and pharynx, which may be confused with oral ulcers of other causes.
About 4% of all cancers occur in the mouth, most commonly as squamous cell carcinomas of the mucosal epithelium ( Chapter 176 ). Oral carcinoma occurs usually in the fifth decade or beyond, in men twice as frequently as in women, and is associated with long-term use of tobacco in more than 80% of cases.
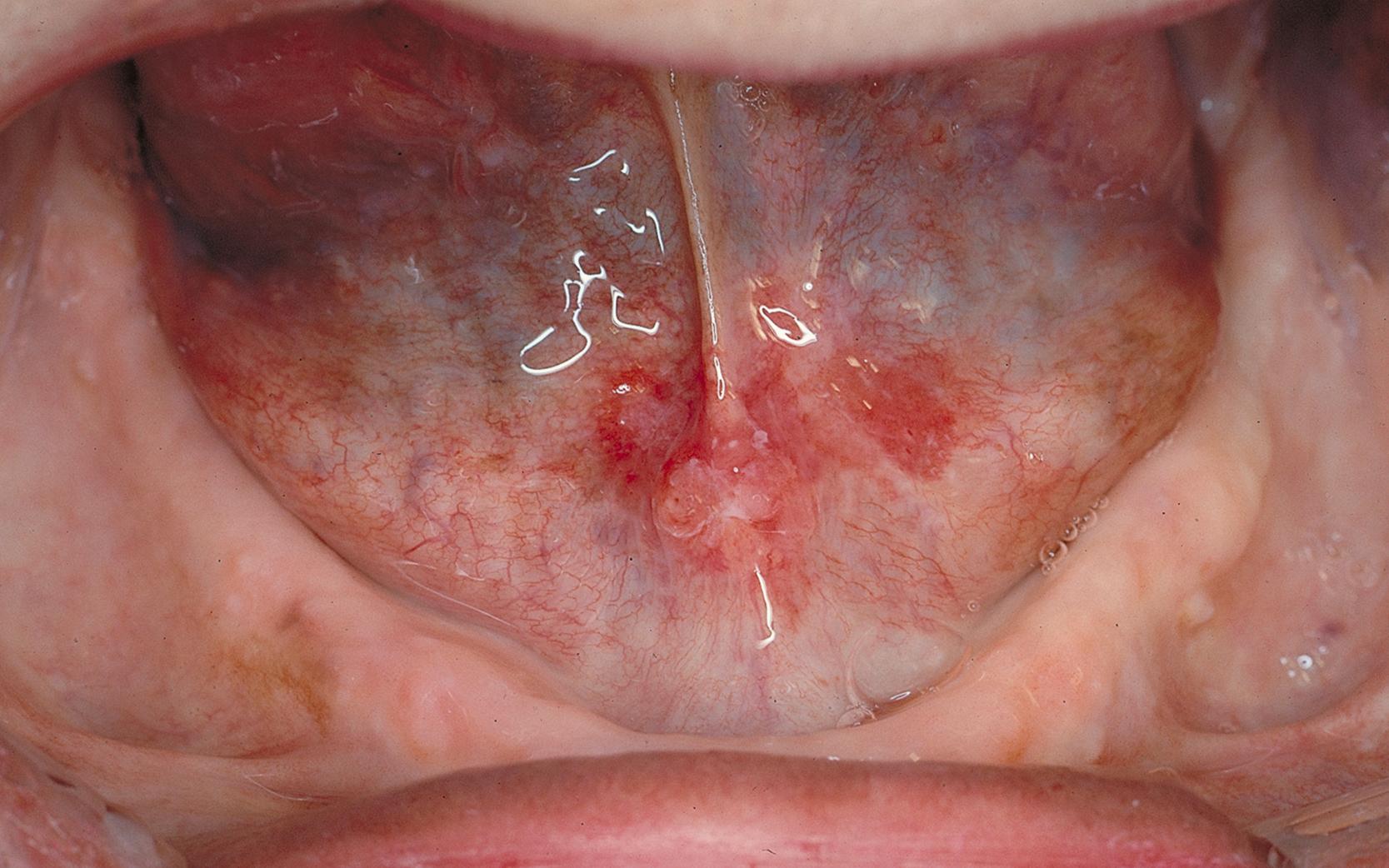
Oral carcinoma usually arises as a chronic, indurated, cratered ulcer, but white (leukoplakia) and especially red (erythroplakia) macular lesions ( Table 393-3 ; Fig. 393-3 ) frequently exhibit premalignant epithelial dysplasia or early carcinoma. Oral carcinomas spread to cervical lymph nodes. The overall 5-year survival rate is about 50%, but early treatment of small, localized lesions can lead to survival rates as high as 90%. Nevertheless, current guidelines find insufficient evidence to recommend for or against screening in asymptomatic adults.
| WHITE LESIONS (PLAQUES) |
| Squamous cell carcinoma (early) Frictional keratosis (buccal mucosa at dental occlusal line) Leukoplakia (with or without dysplasia) Smokeless tobacco–associated lesions Nicotine stomatitis (palate) Lichen planus (reticular and plaque types) Pseudomembranous candidiasis (thrush) Hyperplastic candidiasis (candidal leukoplakia) Hairy leukoplakia (immunosuppression related, often with HIV infection; usually on lateral tongue) Geographic tongue (benign migratory glossitis) Mucous patch or condyloma latum of secondary syphilis Pseudomembrane-covered ulcers (see Table 393-1 ) |
| RED OR BLUE LESIONS (MACULAR, MACULOPAPULAR) |
| Squamous cell carcinoma (early) Erythroplakia (epithelial dysplasia) Erythematous (atrophic) candidiasis Median rhomboid glossitis Mucocutaneous diseases (see Table 393-1 ) Angular cheilitis Telangiectasias and purpuras (red to blue) Kaposi sarcoma (blue to purple) |
Over the past two decades, there has been a rapid increase in a type of head and neck cancer associated with human papillomavirus (HPV) type 16 ( Chapter 344 ). Occurring primarily at the base of the tongue and tonsillar region of the oropharynx, this form of nonkeratinizing squamous cell carcinoma is seen in younger patients who typically lack the history of smoking and alcohol. Other features of the disease include advanced stage at presentation and its favorable response to radiation and chemotherapy ( Chapter 176 ). In the absence of concurrent tobacco use, the 5-year survival rate is over 80%.
Prescription drugs that can be responsible for chronic oral mucosal ulcerations include barbiturates, β-blockers, nonsteroidal anti-inflammatory drugs, allopurinol, isoniazid, and many others. Several mucocutaneous diseases can cause chronic multifocal oral mucosal lesions composed of ill-defined areas of erythema and ulceration. They are among the most difficult oral lesions to diagnose and are discussed later with the red lesions (see Table 393-3 ). Several microbial infections or underlying osteonecrosis (e.g., with the use of bisphosphonates and other antiresorptive medications) can lead to indurated, chronic oral mucosal ulcerations with moderate symptoms (see Table 393-1 ).
White plaques are commonly found in the mouth and, like ulcerations, have a wide variety of causes and outcomes (see Table 393-3 ). The clinical descriptor term leukoplakia applies to a white plaque that does not rub off and whose appearance does not indicate another disease. Leukoplakia can occur in any area of the mouth and usually exhibits benign hyperkeratosis on biopsy. On long-term follow-up, about 7% of these lesions undergo malignant transformation into squamous cell carcinoma. Leukoplakias that are shown on biopsy to contain epithelial dysplasia have a higher rate of transformation to cancer than those that do not, thereby emphasizing the important role of biopsy for these lesions. Areas of leukoplakia with a corrugated surface or mixed with areas of erythema are often found in the lower labial or buccal vestibule of patients who use smokeless tobacco.
Frictional keratoses are often found posterior to the lower molar teeth as irregular white plaques and on the buccal mucosa as white lines adjacent to the dental occlusion. Unlike leukoplakia, these lesions rarely become malignant.
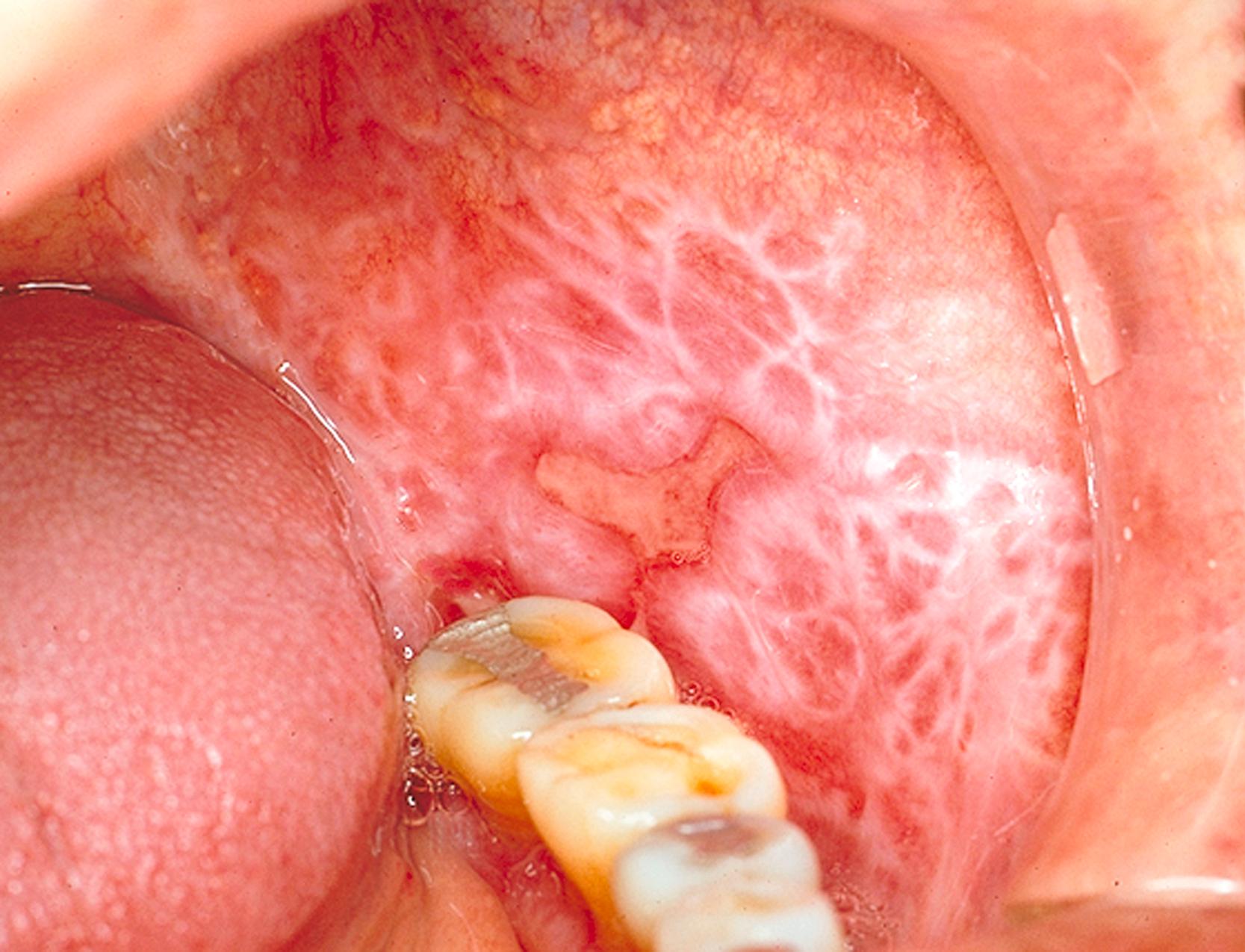
Oral lesions of lichen planus ( Chapter 405 ) occur in about 1% of the population, usually as multiple, bilaterally symmetrical reticular (lattice-like) white lesions, with or without adjacent areas of erythema (atrophy or erosion) or irregular ulcers ( Fig. 393-4 ). The presence of mucosal atrophy, erosion, or ulceration usually causes pain and sensitivity to certain foods. Most lesions can be adequately controlled by topical application of fluocinonide or clobetasol gel or ointment (0.05%, three times a day) for periods of several weeks, although recurrence is common.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here