Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lumbar disc degeneration has been defined by the North American Spine Society Consensus Committee on Nomenclature in terms of morphologic changes involving the anatomic components of the lumbar disc. These changes may include:
Desiccation, fibrosis, vacuum changes, or cleft formation in the nucleus
Fissuring, mucinous degeneration, or calcification in the annulus
Defects and sclerosis of the vertebral endplates
Osteophytes at the vertebral apophysis
Although disc degeneration is virtually universal in the aging spine, disc degeneration is inconsistently and only occasionally associated with pain and functional limitation. Degenerative disc disease (DDD) is broadly defined as a clinical syndrome characterized by manifestations of disc degeneration and symptoms attributed to these changes. Causal connections between degenerative changes and symptoms are often difficult clinical distinctions. No evidence-based consensus exists for differentiating pathologic degenerative disc changes from disc changes associated with normal aging.
Lumbar DDD refers to a continuum of nonradicular pain disorders of degenerative origin. Specifically excluded are symptoms related to disc impingement on neural elements, facet-mediated back pain, and spinal deformities secondary to lumbar DDD (e.g., spondylolisthesis, degenerative scoliosis).
Clinical presentation is characterized by low back pain, which may radiate to the sacroiliac and/or buttock region. Common physical examination findings include tenderness with palpation over the lumbar region and limited lumbar range of motion. In the absence of concomitant facet joint degeneration, discogenic back pain is often more severe with flexion and less severe with extension.
Radiographic findings include disc height loss, decreased lumbar lordosis, vacuum phenomena, osteophytes, and endplate sclerosis. Similar degenerative changes are frequently noted in asymptomatic patients. A change in radiographic alignment, such as retrolisthesis, from supine to standing or from flexion to extension may occur.
Magnetic resonance imaging (MRI) findings include disc desiccation, annular fissures, high-intensity zones (HIZ), loss of disc space height, and changes in vertebral endplate morphology. No pathognomonic findings have been identified that permit distinction of asymptomatic age-related changes from symptomatic lumbar DDD, though the Pfirrmann classification system is often used to describe the severity of these changes.
Lumbar discography has been utilized as a provocative test to assess patients with DDD. Although controversial, this test attempts to directly identify a cause and effect relationship between MRI findings of DDD and clinical symptoms. Findings that support a diagnosis of discogenic pain include concordant pain on injection of a specific disc level with absent or minimal pain on injection of adjacent control levels. Additional criteria for diagnosis include pain reproduction with a low pressure/low volume injection and presence of abnormal disc morphology. Discography can accelerate degeneration, especially at otherwise normal “control” levels and should not be obtained in patients with abnormal psychometric profiles, chronic pain illness, worker’s compensation claims, and secondary gain issues.
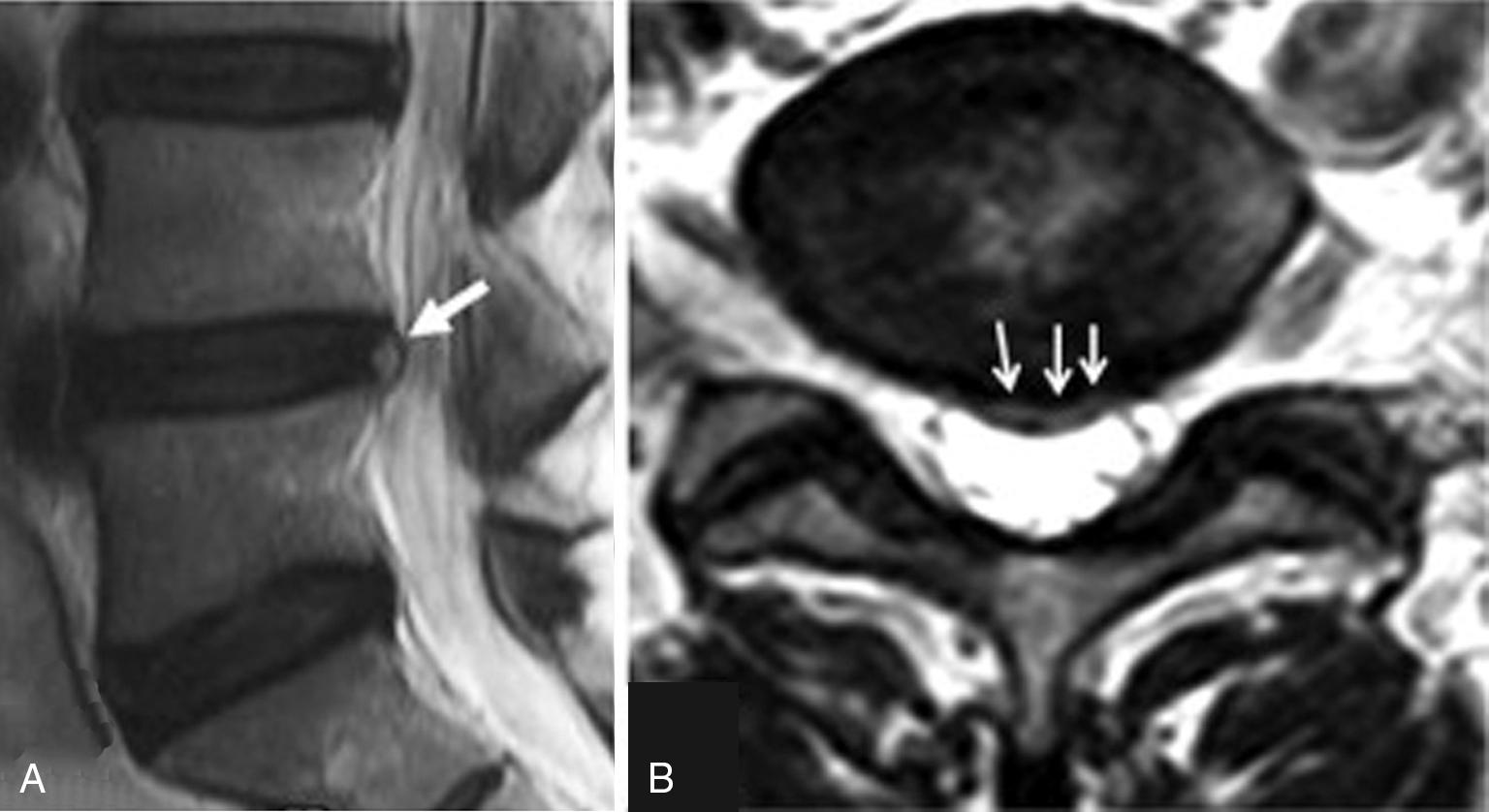
Annular fissures commonly occur as the structural integrity of the annulus of the intervertebral disc is compromised by the degenerative process, but may not always be detected with MRI or discography. Annular fissures are classified as concentric, transverse, or radial types. When fluid or granulation tissue infiltrates an annular fissure, this region may be visualized as an area of increased signal intensity in the posterior annular region on T2-weighted MRI and is termed a high-intensity zone (HIZ). Initial reports suggested that a HIZ was a marker for symptomatic internal disc disruption and concordant pain reproduction with discography. However, additional studies have demonstrated that a HIZ is not a specific marker for symptomatic disc disruption as this finding may be present in many asymptomatic individuals ( Fig. 48.1 ).
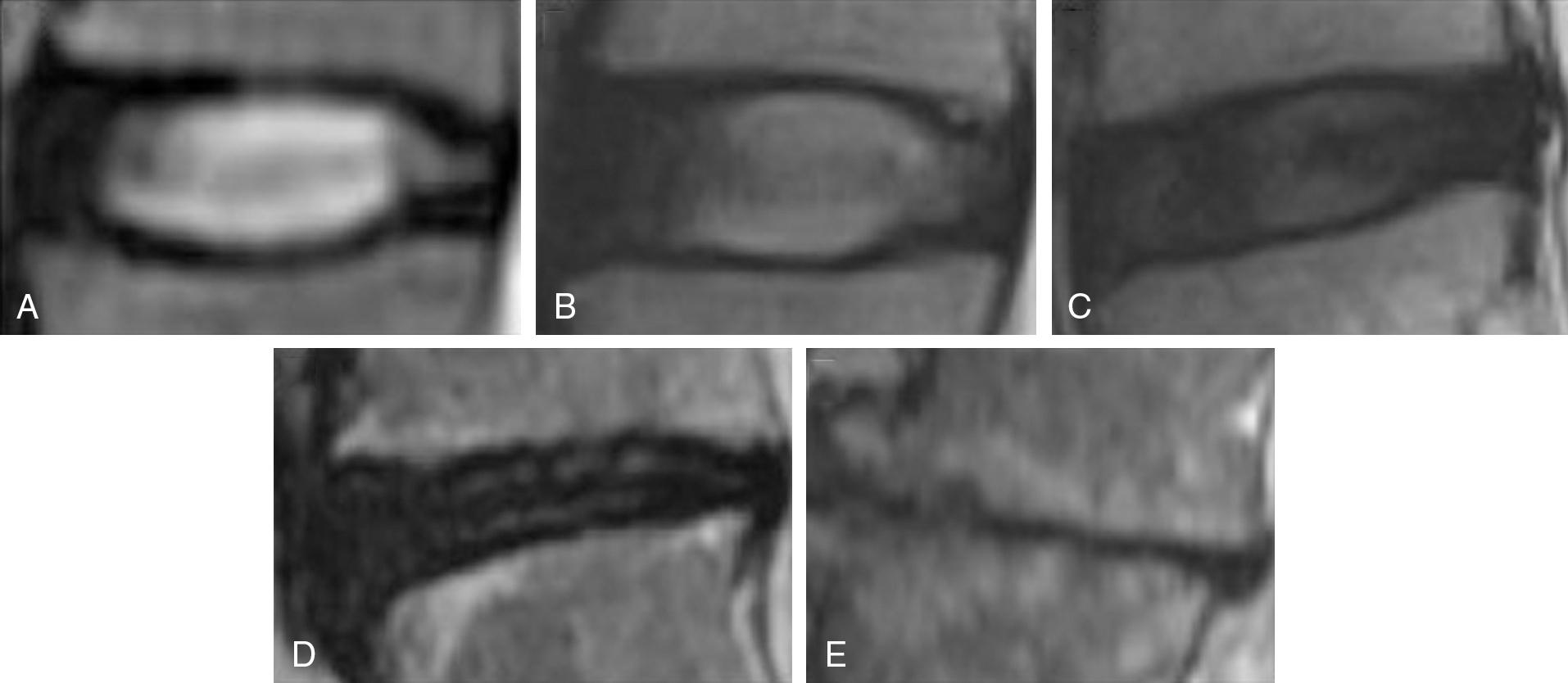
The Pfirrmann classification is a five-grade system, which considers disc structure, the distinction between the nucleus pulposus and annulus fibrosus, signal intensity of the disc nucleus, and intervertebral disc height.
Grade 1: Defined as a homogenous nucleus pulposus, high T2 signal intensity, clear distinction of the nucleus and annulus, and normal disc height.
Grade 2: Defined as an inhomogenous nucleus pulposus with or without horizontal bands, high T2 signal intensity, clear distinction of the nucleus and annulus, and normal disc height.
Grade 3: Defined as an inhomogenous, gray nucleus pulposus, intermediate T2 signal intensity, unclear distinction of the nucleus and annulus, and normal to slightly decreased disc height.
Grade 4: Defined as an inhomogenous, gray to black nucleus pulposus, intermediate to low T2 signal intensity, loss of distinction of the nucleus and annulus, and normal to moderately decreased disc height.
Grade 5: Defined as an inhomogenous, black nucleus pulposus, low T2 signal intensity, loss of distinction of the nucleus and annulus, and severe loss of disc height ( Fig. 48.2 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here