Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The feasibility of arterial reconstruction was first realized in the early 1900s through pioneering early studies performed by Carrell and Guthrie at the University of Chicago, as well as Bernheim at Johns Hopkins University. The availability of a safe heparin formulation, as developed by Best at the University of Toronto by the late 1940s, enabled arterial bypass grafting to be a practical intervention for the treatment of limb ischemia. In 1951 Kunlin reported using reversed great saphenous vein for femoral popliteal artery bypass grafting to successfully treat foot gangrene. In describing his experience with 17 vein bypass graft procedures, Kunlin was the first to introduce the end-to-side anastomosis as a means of preserving collateral branches near the thrombotic zone. He advocated a two-suture technique with separate heel and toe sutures. Heparin was administered and maintained postoperatively, followed by coumadin anticoagulation. Whereas a small number of vein grafts were performed for treatment of vascular injuries in World War II, during the Korean and Vietnam wars traumatic arterial injuries treated with vein bypass emerged as an alternative treatment to simple ligation or amputation. Likewise, in the 1950s case series replicated Kunlin’s approach with reports of excellent results with vein bypass grafting to treat chronic limb ischemia. By the end of the 1960s arterial bypass with venous conduit was a well-accepted treatment for symptomatic limb ischemia. Although endovascular techniques have emerged as an option for infrainguinal revascularization, arterial bypass grafting with venous conduit is still regarded as the gold standard with which endovascular techniques are compared with regard to efficacy and durability in the treatment of lowerextremity ischemia.
Tibial and peroneal artery bypass procedures are indicated for the treatment of ischemic rest pain, chronic ischemic ulcerations, gangrene of the foot, and highly selected patients with short distance claudication. Patients with critical limb ischemia (CLI) however, comprise the vast majority of patients for whom distal revascularization procedures are performed; many vascular surgeons only consider tibial level bypass grafting for CLI.
Coronary artery disease. Patients undergoing tibial artery bypass are more likely to have vascular disease and comorbidities of greater severity than those undergoing more proximal bypass. Given the ubiquitous presence of coronary artery disease in patients with peripheral arterial disease, patients with CLI should be considered for assessment of cardiac status before vascular reconstruction. In addition to a preoperative electrocardiogram, an echocardiogram and noninvasive cardiac stress testing with cardiac imaging are often selectively used to assist with preoperative risk stratification. This information can also be useful in postoperative management. According to American College of Cardiology/American Heart Association guidelines, coronary revascularization is not indicated in patients with stable coronary artery disease undergoing vascular surgery, including lower extremity arterial reconstruction.
Risk factor modification. Medical therapy should be optimized before lower extremity revascularization. Specifically, hypertension and diabetes should be under good control. Smoking cessation is encouraged. Beta-blockers should be continued through the perioperative period, and consideration should be given to initiation of beta-blockers in select beta-blocker naïve patients. Patients should be on a statin medication preoperatively. Statin use has been shown to decrease the rate of perioperative myocardial infarction and cerebral ischemic events in vascular surgical patients and may increase vein graft patency.
Antiplatelet therapy. All patients with peripheral arterial disease, including those undergoing lower extremity bypasses, should be on antiplatelet medication, preferably aspirin (81-325 mg/day) or clopidogrel (75 mg/day).
Imaging. Digital subtraction arterial angiography is the preoperative imaging modality of choice to determine revascularization targets for tibial artery bypass. Detailed views of the foot and lower leg, including a lateral view, are needed to best identify patent arteries to determine the best distal target for the bypass.
Conduit selection. The quality of the conduit is the most important factor in the success of a lower extremity bypass procedure. Great saphenous vein is the conduit of choice in leg bypass grafts, particularly when the reconstruction is carried to tibial and pedal vessels. Ultrasound vein mapping should be performed preoperatively to identify optimal venous conduit.
Wounds. Operative planning must take into account the location of chronic or infected wounds when deciding where to place incisions. Before lower extremity revascularization, active infection should be controlled by antibiotics and aggressive wound care should be initiated.
Tunneling. For reversed vein bypass grafts, the graft should be tunneled while maintaining proper orientation and with the graft fully distended to avoid kinking or twisting.
Working with small-caliber arteries. Surgical loupes are required for accuracy. Delicate handling and fine instrumentation are needed to avoid unnecessary trauma or vasospasm; strategies such as tourniquet control and intraluminal occlusion may be applied in circumstances of highly calcified recipient vessels.
Limited outflow. A distal arteriovenous fistula may increase graft patency. Long-term anticoagulation with warfarin may increase graft patency when prosthetic grafts are used.
Selection of conduit for tibial bypass is of paramount importance. The best conduit is great saphenous vein, but when not available, another source of vein should be obtained. As such, preoperative vein mapping using duplex ultrasound should be performed before tibial bypass to identify the optimal venous conduit. In general, thin-walled veins, 3 to 5 mm in diameter, serve as good conduits.
Failure rates are high with use of an inadequate conduit. The ipsilateral great saphenous vein is preferred, but if unavailable or inadequate, adequate contralateral great saphenous vein is the next best choice. Saving a contralateral great saphenous vein for a possible future coronary or contralateral lower extremity bypass is a fallacious argument. The best available vein should be used for the current operation and not saved for a future potential operation. If adequate great saphenous vein is not available, single-segment arm vein is preferred, usually cephalic vein for tibial bypass, followed by spliced, composite vein composed of the best available venous conduits.
Prosthetic conduits are inferior for tibial bypass. However, if reasonable autogenous conduit is not available, a prosthetic conduit can be used for tibial bypass. Adjuncts, such as heparin-impregnated grafts and Linton patch angioplasty, at the distal anastomotic site have been advocated to improve results. Acceptable short-term results have been reported.
The selection of an adequate inflow site is dictated by the preoperative imaging studies and the amount of available conduit. Preferably, the inflow pulse should be strong and not distal to known high-grade stenoses. Depending on conduit availability, preoperative angiographic assessment may allow correction, either by angioplasty or stenting, of proximal lesions to potential inflow sites. At operation, the inflow artery is palpated to assess pulsatility, plaque presence and location, and its suitability for clamping and anastomosis. Arteries suitable for inflow to the tibials are the common femoral artery, profunda femoris artery, superficial femoral artery and the above- and below-knee popliteal arteries. Occasionally, proximal tibial vessels can also be used as inflow sources. The more distal the inflow source, the shorter the length of conduit required, and in general, shorter conduits are preferred over longer conduits.
Should there be any question regarding the adequacy of inflow of the selected artery for the proximal anastomosis, a pressure gradient can be measured at that location by comparing the measured pressure with the systemic pressure. Some surgeons recheck the pressure after intraarterial administration of a vasodilator at the site, such as 200 mcg of nitroglycerine or 30 mg of papaverine. After the administration of a vasodilator, a gradient of 15 to 20 mm Hg systolic pressure is considered significant.
The outflow target vessel for receipt of the bypass should be in continuity with the pedal vessels. However, the peroneal artery is an acceptable target vessel, despite the lack of direct communication to the pedal circulation. Arteries distal to the outflow target should be free of hemodynamically significant stenoses.
Heavily calcified tibial arteries encountered at operation should not preclude anastomosis provided the lumen is patent. Modified cutting “armor piercing” needles may be helpful in constructing the anastomosis in these circumstances, in addition to the strategies noted earlier.
Open wounds pose a risk of contamination to the operative field, potentially exposing the vascular graft to infection and increasing the risk of a wound infection. Preoperative incision planning needs to take into account open wounds in the lower extremity. In addition, the operative sites should be chosen so that the graft is adequately covered with viable tissue. Incisions should be made as far away from open wounds as feasible. Grossly infected or large wounds are excluded from the operative field by first scrubbing with a povidone-iodine preparation (Betadine) and then isolating the wound with an Ioban (3M, St. Paul), iodophor-impregnated adhesive occlusive dressing. A piece of gauze may be left in the wound bed to soak up drainage. Feet are routinely covered with sterile bags to also help limit contamination.
Dissection of tibial vessels should be done with minimal handling to avoid vasospasm. A combination of sharp and blunt dissection using fine-tipped tonsil dissectors or mosquito-type clamps with fine Metzenbaum scissors or tenotomy scissors works well. Self-retaining retractors are used to provide exposure. Dissection-induced vasospasm can be relieved by topical application of papaverine.
Tunneling the graft requires a rigid tunneling device that allows passage of the vein graft from the inflow site to the outflow artery without twisting or kinking. Tunneling is performed before heparinization and may be anatomic or subcutaneous.
Vascular clamps are preferably placed on soft portions of the artery. A Wylie subclavian clamp is a reliable choice for control of the common femoral artery. Its jaws can be oriented anterior or posterior to the long axis of the artery, compressing the usually soft anterior artery wall flat against the posterior plaque. Clamping the artery walls side to side, fractures the posterior plaque along its length in an uncontrolled manner. If suitable, the superficial femoral artery and profunda femoris artery can be controlled with small vascular clamps or vessels loops. Balloon occlusion with a Fogarty embolectomy catheter inflated with heparinized saline can also effectively control inflow arteries unsuitable for clamping. In operative sites where the artery is deep, tightened vessel loops can help raise the artery into the wound, easing the awkwardness of “working in a hole.”
Vascular control of smaller arteries can be achieved with double-looped, tightened vessel loops, small vascular clamps, Fogarty balloon catheters or intraluminal vessel occluder, such as the Flo-rester (Synovis Surgical Innovations, St. Paul). The vessels are rarely unable to be locally controlled in the incision; however, a sterile tourniquet may also be used to provide proximal vascular control. The use of the tourniquet obviates the need for complete circumferential dissection of the artery, which facilitates the procedure when significant inflammatory changes exist between the artery and the vein. A tourniquet is used after the proximal anastomsis has been completed and the vein graft tunneled to the site of the distal anastomosis. With the patient fully heparinized, the foot and leg are elevated and exsanguinated with an Esmarch bandage, followed by the inflation of a low thigh tourniquet to 300 mm Hg. Placement of a tourniquet around the upper calf should be avoided because of the potential risk of injury to the peroneal nerve as it crosses the head of the fibula. Complications are uncommon with tourniquet times of less than 1 hour.
Because of the long length of venous conduit required to perform distal bypasses, the distal diameter of the conduit, which serves as the inflow end of a reversed vein graft, may be small when compared with the inflow artery. The venous hood can be augmented by incorporating a venous side branch into the heel of the hood configuration ( Figs. 45-1 and 45-2 ). The in situ or nonreversed vein bypass technique provides a method for optimal size matching of the vein conduit to the inflow and outflow arteries, which is preferred by some surgeons for tibial bypass grafting.
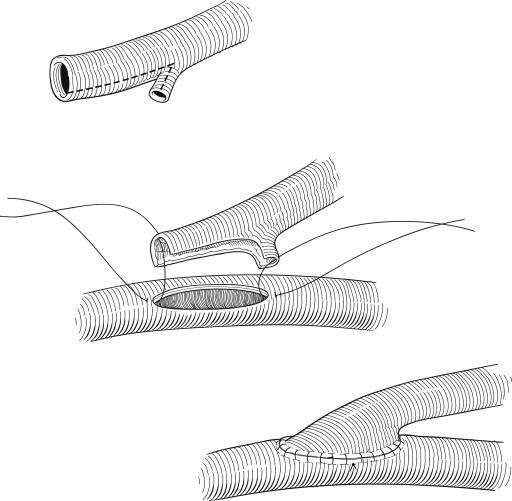
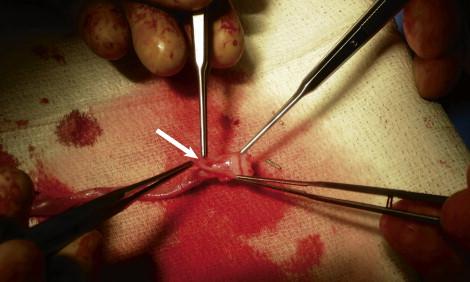
The distal anastomosis is performed with either 6-0 or 7-0 double-armed, nonabsorbable monofilament suture. Heel and toe stitches are placed to anchor the anastomosis, and then the sutures are run toward the midportion of the anastomosis. Another method that is useful in small, visually constrained fields is to “parachute” the heel stitches. This allows the graft to float above the field, providing an unobstructed field of view within which to place heel sutures. Once the heel sutures are placed, the anastomosis can be pulled down and completed in the standard fashion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here