Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The history begins with a narrative provided by the parent/caretaker with input from the patient. It should include questions about respiratory symptoms (dyspnea, cough, pain, wheezing, snoring, apnea, cyanosis, exercise intolerance), as well as their chronicity, timing during day or night, and associations with activities including exercise or food intake. The respiratory system interacts with a number of other systems, and questions related to cardiac, gastrointestinal, central nervous, hematologic, and immune systems may be relevant. Questions related to gastrointestinal reflux, congenital abnormalities (airway anomalies, ciliary dyskinesia), or immune status may be important in a patient with repeated pneumonia. The family history is essential and should include inquiries about siblings and other close relatives with similar symptoms, or any chronic disease with respiratory components.
Respiratory dysfunction usually produces detectable alterations in the pattern of breathing. Values for normal respiratory rates are presented in Table 81.1 and depend on many factors—most importantly, age. Repeated respiratory rate measurements are necessary because respiratory rates, especially in the young, are exquisitely sensitive to extraneous stimuli. Sleeping respiratory rates are more reproducible in infants than those obtained during feeding or activity. These rates vary among infants but average 40-50 breaths/min in the 1st few wk of life and usually <60 breaths/min in the 1st few days of life.
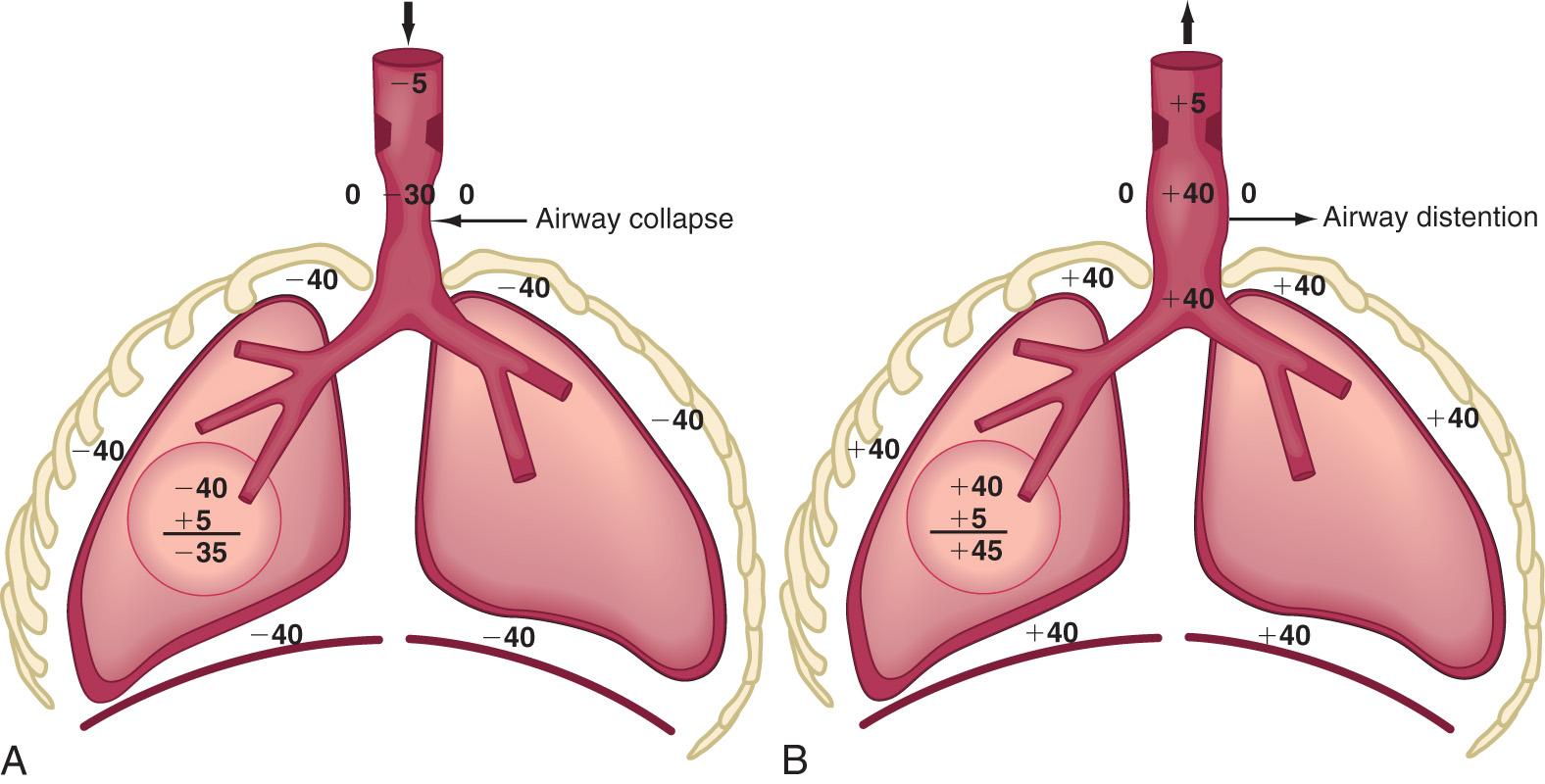
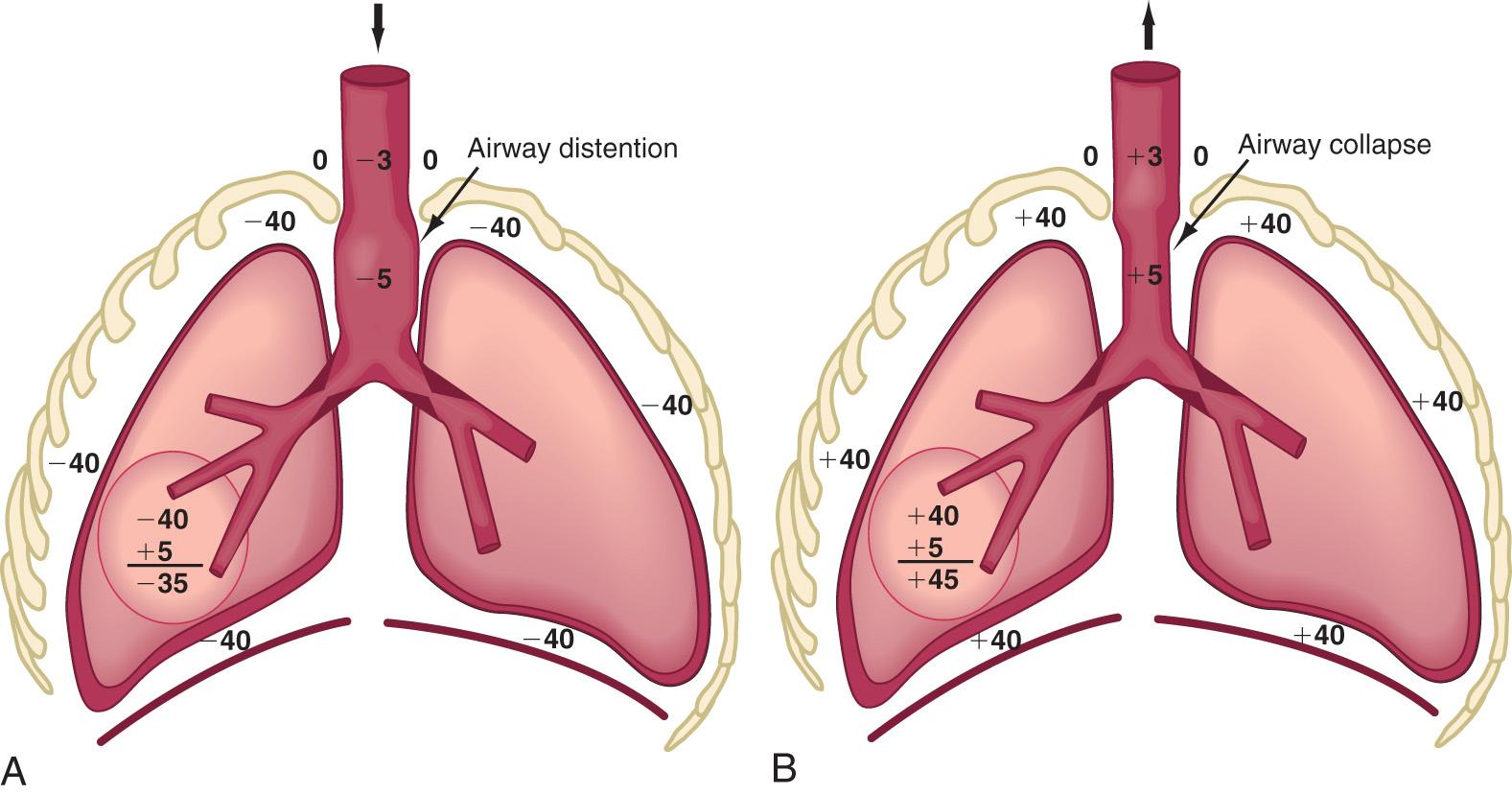
Respiratory control abnormalities can cause the child to breathe at a low rate or periodically. Mechanical abnormalities produce compensatory changes that are generally directed at altering minute ventilation to maintain alveolar ventilation. Decreases in lung compliance require increases in muscular force and breathing rate, leading to variable increases in chest wall retractions and nasal flaring. The respiratory excursions of children with restrictive disease are shallow. An expiratory grunt is common as the child attempts to raise the functional residual capacity (FRC) by closing the glottis at the end of expiration. The FRC is the amount of air left in the lungs after tidal expiration. Children with obstructive disease might take slower, deeper breaths. When the obstruction is extrathoracic (from the nose to the mid-trachea), inspiration is more prolonged than expiration, and an inspiratory stridor (a predominant inspiratory monophonic noise) can usually be heard ( Fig. 400.1 ). When the obstruction is intrathoracic , expiration is more prolonged than inspiration, and the patient often has to make use of accessory expiratory muscles. Intrathoracic obstruction results in air trapping and, therefore, a larger residual volume, as well as a possible increase in FRC ( Fig. 400.2 ).
Lung percussion has limited value in small infants because it cannot discriminate between noises originating from tissues that are close to each other. In adolescents and adults, percussion is usually dull in restrictive lung disease, with a pleural effusion, pneumonia, and atelectasis, but it is tympanitic in obstructive disease (asthma, pneumothorax).
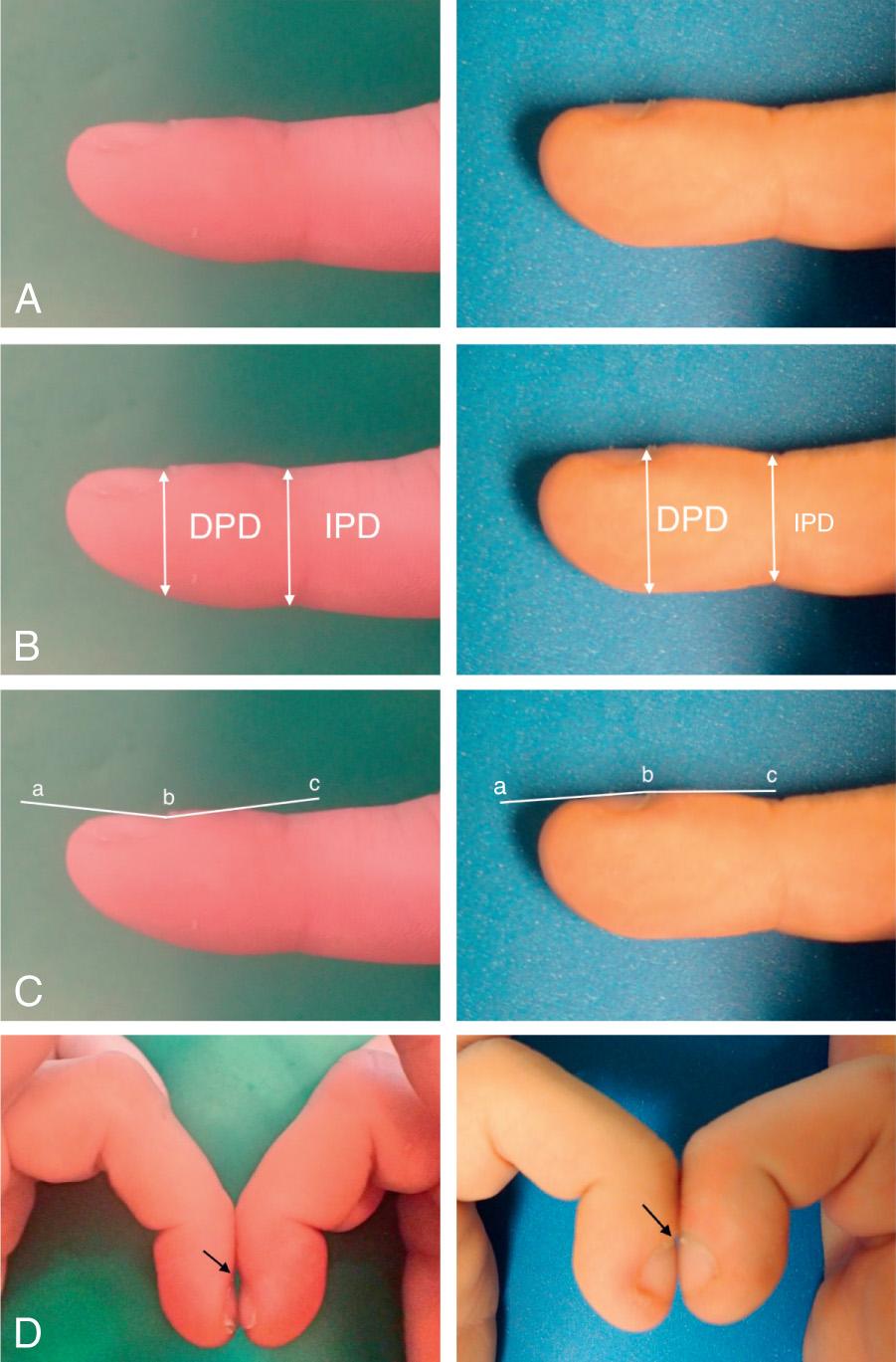
Auscultation confirms the presence of inspiratory or expiratory prolongation and provides information about the symmetry and quality of air movement. In addition, it often detects abnormal or adventitious sounds such as stridor ; crackles or rales , high-pitched, interrupted sounds found during inspiration and more rarely during early expiration, which denote opening of previously closed air spaces; or wheezes , musical, continuous sounds usually caused by the development of turbulent flow in narrow airways ( Table 400.1 ). Digital clubbing is a sign of chronic hypoxia and chronic lung disease ( Fig. 400.3 ) but may be a result of nonpulmonary etiologies ( Table 400.2 ).
| BASIC SOUNDS | MECHANISMS | ORIGIN | ACOUSTICS | RELEVANCE |
|---|---|---|---|---|
| Lung | Turbulent flow, vortices, other | Central (expiration), lobar to segmental airways (inspiration) | Low pass filtered noise (<100 to >1,000 Hz) | Regional ventilation, airway caliber |
| Tracheal | Turbulent flow, flow impinging on airway walls | Pharynx, larynx, trachea, large airways | Noise with resonances (<100 to >3,000 Hz) | Upper airway configuration |
| ADVENTITIOUS SOUNDS | ||||
| Wheezes | Airway wall flutter, vortex shedding, other | Central and lower airways | Sinusoidal (<100 to >1,000 Hz, duration typically >80 msec) | Airway obstruction, flow limitation |
| Rhonchi | Rupture of fluid films, airway wall vibration | Larger airways | Series of rapidly dampened sinusoids (typically <300 Hz and duration <100 msec) | Secretions, abnormal airway collapsibility |
| Crackles | Airway wall stress-relaxation | Central and lower airways | Rapidly dampened wave deflections (duration typically <20 msec) | Airway closure, secretions |
| CARDIAC |
|
|
|
| HEMATOLOGIC |
|
|
| GASTROINTESTINAL |
|
|
|
|
|
|
|
|
|
| OTHER |
|
|
|
|
|
|
|
|
|
| UNILATERAL CLUBBING |
|
|
|
|
The main function of the respiratory system is to remove carbon dioxide from and add oxygen to the systemic venous blood brought to the lung. The composition of the inspired gas, ventilation, perfusion, diffusion, and tissue metabolism has a significant influence on the arterial blood gases.
The total pressure of the atmosphere at sea level is 760 torr. With increasing altitude, the atmospheric pressure decreases. The total atmospheric pressure is equal to the sum of partial pressures exerted by each of its component gases. Alveolar air is 100% humidified, so in alveolar gas calculations, the inspired gas is also presumed to be 100% humidified. At a temperature of 37°C (98.6°F) and 100% humidity, water vapor exerts pressure of 47 torr, regardless of altitude. In a natural setting, the atmosphere consists of 20.93% oxygen. Partial pressure of oxygen in inspired gas (Pi o 2 ) at sea level is therefore (760 − 47) × 20.93% = 149 torr. When breathing 40% oxygen at sea level, Pi o 2 is (760 − 47) × 40% = 285 torr. At higher altitudes, breathing different concentrations of oxygen, Pi o 2 is less than at sea level, depending on the prevalent atmospheric pressures. In Denver (altitude of 5,000 feet and barometric pressure of 632 torr), Pi o 2 in room air is (632 − 47) × 20.93% = 122 torr, and in 40% oxygen, it is (632 − 47) × 40% = 234 torr.
Minute volume is a product of V T and respiratory rate. Part of the V T occupies the conducting airways (anatomic dead space), which does not contribute to gas exchange in the alveoli. Alveolar ventilation is the volume of atmospheric air entering the alveoli and is calculated as (V T − dead space) × respiratory rate. Alveolar ventilation is inversely proportional to arterial P co 2 (Pa co 2 ). When alveolar ventilation is halved, Pa co 2 is doubled. Conversely, doubling of alveolar ventilation decreases Pa co 2 by 50%. Alveolar P o 2 (Pa o 2 ) is calculated by the alveolar air equation as follows, where R is the respiratory quotient. For practical purposes, PA co 2 is substituted by arterial P co 2 (Pa co 2 ), and R is assumed to be 0.8. According to the alveolar air equation, for a given Pi o 2 , a rise in Pa co 2 of 10 torr results in a decrease in PA o 2 by 10 ÷ 0.8, or 10 × 1.25, or 12.5 torr. Thus proportionately inverse changes in PA o 2 occur to the extent of 1.25× the changes in PA co 2 (or Pa co 2 ).
After the alveolar gas composition is determined by the inspired gas conditions and process of ventilation, gas exchange occurs by the process of diffusion and equilibration of alveolar gas with pulmonary capillary blood. Diffusion depends on the alveolar capillary barrier and the amount of available time for equilibration. In health, the equilibration of alveolar gas and pulmonary capillary blood is complete for both oxygen and carbon dioxide. In diseases in which the alveolar capillary barrier is abnormally increased (alveolar interstitial diseases) and/or when the time available for equilibration is decreased (increased blood flow velocity), diffusion is incomplete. Because of its greater solubility in liquid medium, carbon dioxide is 20 times more diffusible than oxygen. Therefore, diseases with diffusion defects are characterized by marked alveolar-arterial oxygen (A-aO 2 ) gradients and hypoxemia. Significant elevation of CO 2 does not occur as a result of a diffusion defect unless there is coexistent hypoventilation.
Venous blood brought to the lungs is “arterialized” after diffusion is complete. After complete arterialization, the pulmonary capillary blood should have the same P o 2 and P co 2 as in the alveoli. The arterial blood gas composition is different from that in the alveoli, even in normal conditions, because there is a certain amount of dead space ventilation as well as venous admixture in a normal lung. Dead space ventilation results in a higher Pa co 2 than PA co 2 , whereas venous admixture or right-to-left shunting results in a lower Pa o 2 compared with the alveolar gas composition ( Fig. 400.4 ). Pa o 2 is a reflection of the amount of oxygen dissolved in blood, which is a relatively minor component of total blood oxygen content. For every 100 torr P o 2 , there is 0.3 mL of dissolved O 2 in 100 mL of blood. The total blood oxygen content is composed of the dissolved oxygen and the oxygen bound to hemoglobin (Hb). Each gram of Hb carries 1.34 mL of O 2 when 100% saturated with oxygen. Thus 15 g of Hb carries 20.1 mL of oxygen. Arterial oxygen content (Ca o 2 ) , expressed as mL O 2 /dL blood, can be calculated as (Pa o 2 × 0.003) + (Hb × 1.34 × S o 2 ), where Hb is grams of Hb per deciliter of blood and S o 2 is percentage of oxyhemoglobin saturation. The relationship of P o 2 and the amount of oxygen carried by the Hb is the basis of the O 2 -Hb dissociation curve ( Fig. 400.5 ). The P o 2 at which Hb is 50% saturated is referred to as P 50 . At a normal pH, Hb is 94% saturated at P o 2 of 70, and little further gain in saturation is accomplished at a higher P o 2 . At P o 2 <50, there is a steep decline in saturation and therefore the oxygen content.
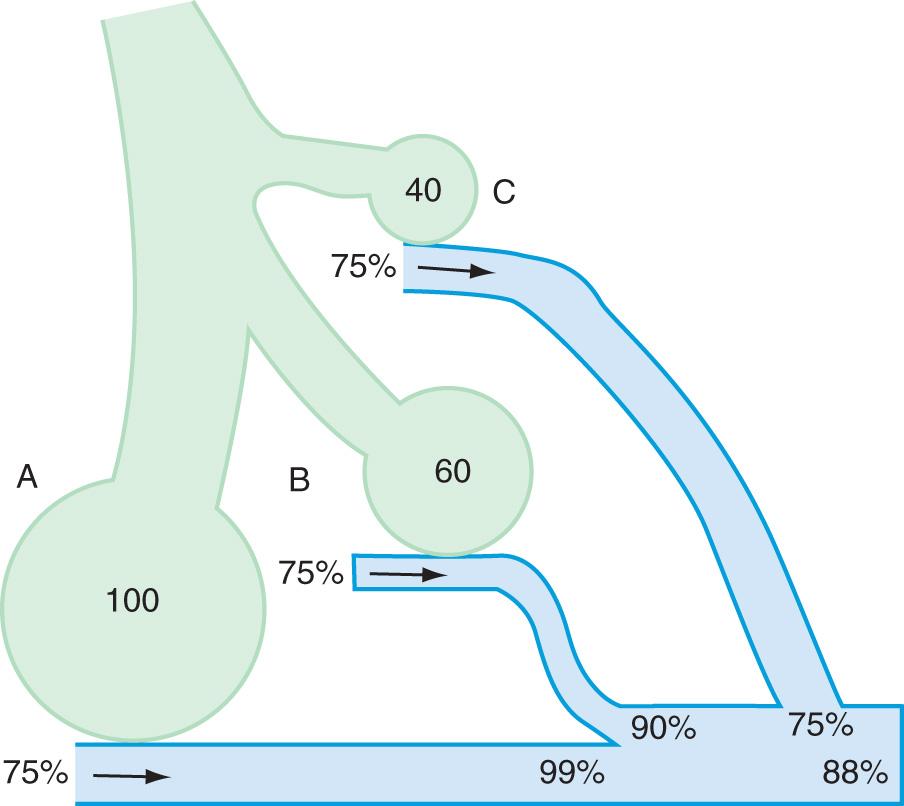
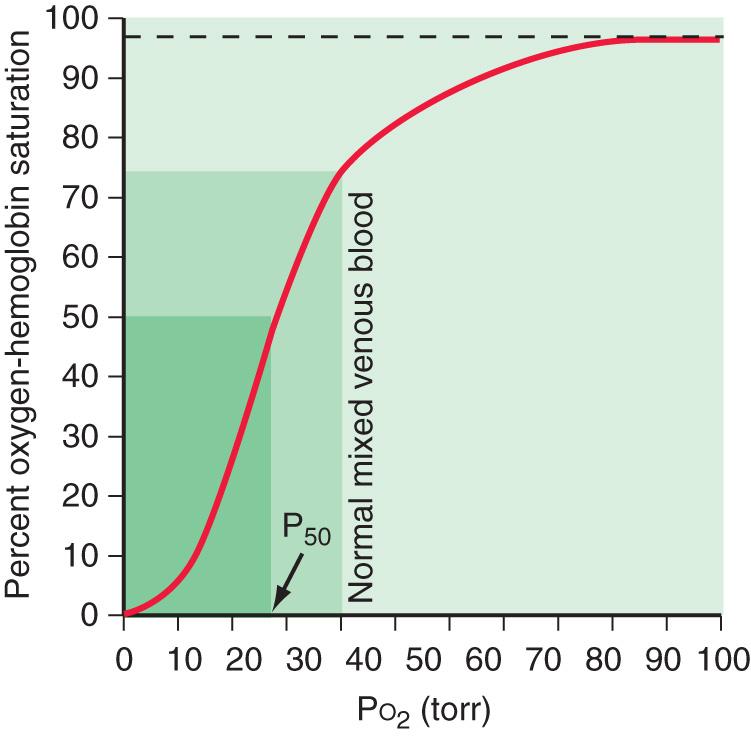
Oxygen delivery to tissues is a product of oxygen content and cardiac output. When Hb is near 100% saturated, blood contains approximately 20 mL oxygen per 100 mL or 200 mL/L. In a healthy adult, cardiac output is approximately 5 L/min, oxygen delivery 1,000 mL/min, and oxygen consumption 250 mL/min. Mixed venous blood returning to the heart has a P o 2 of 40 torr and is 75% saturated with oxygen. Blood oxygen content, cardiac output, and oxygen consumption are important determinants of mixed venous oxygen saturation. Given a steady-state blood oxygen content and oxygen consumption, the mixed venous saturation is an important indicator of cardiac output. A declining mixed venous saturation in such a state indicates decreasing cardiac output.
Clinical observations and interpretation of blood gas values are critical in localizing the site of the lesion and estimating its severity ( Table 400.3 ). In airway obstruction above the carina (subglottic stenosis, vascular ring), blood gases reflect overall alveolar hypoventilation. This is manifested by an elevated PA co 2 and a proportionate decrease in Pa o 2 as determined by the alveolar air equation. A rise in Pa co 2 of 20 torr decreases Pa o 2 by 20 × 1.25 or 25 torr. In the absence of significant parenchymal disease and intrapulmonary shunting, such lesions respond very well to supplemental oxygen in reversing hypoxemia. Similar blood gas values, demonstrating alveolar hypoventilation and response to supplemental oxygen, are observed in patients with a depressed respiratory center and ineffective neuromuscular function, resulting in respiratory insufficiency. Such patients can be easily distinguished from those with airway obstruction by their poor respiratory effort.
| LESION | EFFECT | TYPICAL ABG |
|---|---|---|
| Central (above the carina) airway obstruction, or Depressed respiratory center, or Ineffective neuromuscular function |
Uniform alveolar hypoventilation | Early increase in P co 2 . Proportionate decrease in P o 2 depending on alveolar air equation Response to supplemental oxygen: Excellent |
| Intrapulmonary airway obstruction | Venous admixture mismatch | Mild: ↓ P co 2 , ↓ P o 2 . Moderate: “normal” P co 2 , ↓↓ P o 2 . Severe: ↑↑ P co 2 , ↓↓↓ P o 2 . Response to supplemental oxygen: good |
| Alveolar–interstitial pathology | Diffusion defect R → L shunt | Early decrease in P o 2 depending on severity Normal or low P co 2 , ↑ P co 2 if fatigue develops Response to supplemental oxygen: fair to poor |
In intrapulmonary airway obstruction (asthma, bronchiolitis), blood gases reflect ventilation-perfusion imbalance and venous admixture. In these diseases, the obstruction is not uniform throughout the lungs, resulting in areas that are hyperventilated and others that are hypoventilated. Pulmonary capillary blood coming from hyperventilated areas has a higher P o 2 and lower P co 2 , whereas that coming from hypoventilated regions has a lower P o 2 and higher P co 2 . A lower blood P co 2 can compensate for the higher P co 2 because the Hb-CO 2 dissociation curve is relatively linear. In mild disease, the hyperventilated areas predominate, resulting in hypocarbia. An elevated Pa o 2 in hyperventilated areas cannot compensate for the decreased Pa o 2 in hypoventilated areas because of the shape of the O 2 -Hb dissociation curve. This results in venous admixture, arterial desaturation, and decreased Pa o 2 (see Fig. 400.4 ). With increasing disease severity, more areas become hypoventilated, resulting in normalization of Pa co 2 with a further decrease in Pa o 2 . A normal or slightly elevated Pa co 2 in asthma should be viewed with concern as a potential indicator of impending respiratory failure. In severe intrapulmonary airway obstruction, hypoventilated areas predominate, leading to hypercarbia, respiratory acidosis, and hypoxemia. The degree to which supplemental oxygenation raises Pa o 2 depends on the severity of the illness and the degree of venous admixture.
In alveolar and interstitial diseases, blood gas values reflect both intrapulmonary right-to-left shunting and a diffusion barrier. Hypoxemia is a hallmark of such conditions occurring early in the disease process. Pa co 2 is either normal or decreased. An increase in Pa co 2 is observed only later in the course, as muscle fatigue and exhaustion result in hypoventilation. Response to supplemental oxygen is relatively poor with shunting and diffusion disorders compared with other lesions.
Most clinical entities present with mixed lesions. A child with a vascular ring might also have an area of atelectasis; the arterial blood gas reflects both processes. The blood gas values reflect the more dominant lesion.
An arterial blood gas analysis is probably the single most useful rapid test of pulmonary function. Although this analysis does not specify the cause of the condition or the specific nature of the disease process, it can give an overall assessment of the functional state of the respiratory system and clues about the pathogenesis of the disease. Because the detection of cyanosis is influenced by skin color, perfusion, and blood Hb concentration, the clinical detection by inspection is an unreliable sign of hypoxemia. Arterial hypertension, tachycardia, and diaphoresis are late, and not exclusive, signs of hypoventilation.
Blood gas exchange is evaluated most accurately by the direct measurement of arterial pressure of oxygen (P o 2 ), pressure of carbon dioxide (P co 2 ), and pH. The blood specimen is best collected anaerobically in a heparinized syringe containing only enough heparin solution to displace the air from the syringe. The syringe should be sealed, placed in ice, and analyzed immediately. Although these measurements have no substitute in many conditions, they require arterial puncture and have been replaced to a great extent by noninvasive monitoring, such as capillary samples and/or oxygen saturation.
The age and clinical condition of the patient need to be taken into account when interpreting blood gas tensions. With the exception of neonates, values of arterial P o 2 <85 mm Hg are usually abnormal for a child breathing room air at sea level. Calculation of the alveolar–arterial oxygen gradient is useful in the analysis of arterial oxygenation, particularly when the patient is not breathing room air or in the presence of hypercarbia. Values of arterial P co 2 >45 mm Hg usually indicate hypoventilation or a severe ventilation–perfusion mismatch, unless they reflect respiratory compensation for metabolic alkalosis (see Chapter 68 ).
In infants up to at least 6 mo of age, a pneumothorax (see Chapter 122.14 ) can often be diagnosed by transilluminating the chest wall using a fiberoptic light probe. Free air in the pleural space often results in an unusually large halo of light in the skin surrounding the probe. Comparison with the contralateral chest is often very helpful in interpreting findings. This test is unreliable in older patients and in those with subcutaneous emphysema or atelectasis.
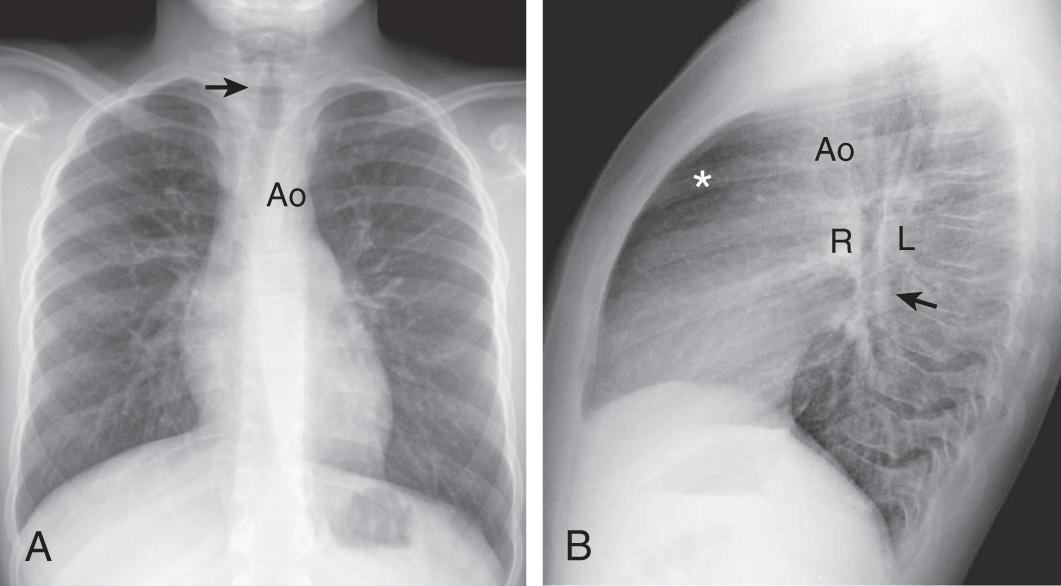
A posteroanterior and a lateral view (upright and in full inspiration) should be obtained, except in situations in which the child is medically unstable ( Fig. 400.6 ). Portable images although useful in the latter situation, can give a somewhat distorted image. Expiratory images can be misinterpreted, although a comparison of expiratory and inspiratory images may be useful in evaluating a child with a suspected foreign body (localized failure of the lung to empty reflects bronchial obstruction: Chapter 414 ). Although images taken in a recumbent position are difficult to interpret when there is fluid within the pleural space or a cavity, if pleural fluid is suspected (see Chapter 429 ), decubitus images are indicated.
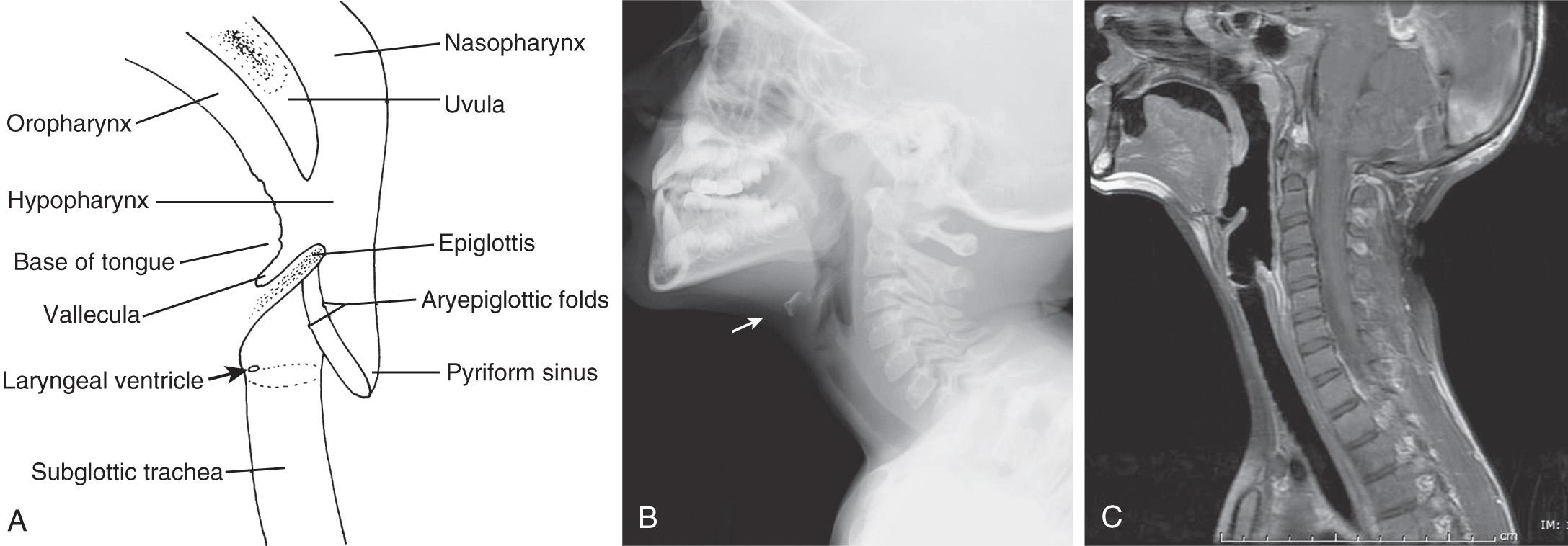
A lateral view of the neck can yield invaluable information about upper airway obstruction (see Chapter 412 ) and particularly about the condition of the retropharyngeal, supraglottic, and subglottic spaces (which should also be viewed in an anteroposterior projection) ( Fig. 400.7 ). Knowing the phase of respiration during which the film was taken is often essential for accurate interpretation. Magnified airway images are often helpful in delineating the upper airways. Patients with suggested obstruction should not be unattended in the radiology department.
The general utility of radiologic examination of the sinuses is uncertain because a large number of images have positive findings (low sensitivity and specificity). Imaging studies are not necessary to confirm the diagnosis of sinusitis in children younger than age 6 yr. CT scans are indicated if surgery is required, in cases of complications caused by sinus infection, in immunodeficient patients, and for recurrent infections that are not responsive to medical management.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here